Acknowledgements
This guide was written by Natalie Lovell, Policy Analyst, and Jo Bibby, Director, Healthy Lives Strategy, at the Health Foundation.
Thank you to all the public health experts and others who contributed to this guide.
Introduction
This guide provides an overview of self-management support and the key components for effective implementation.
It is for people with a role where they can implement self-management support, such as commissioners, health care professionals, service managers, people in voluntary or community groups and patient leaders.
The guide will be useful both for those starting their self-management support journey and those building on and improving the support that they already provide.
With the help of short case studies, it highlights how action can create improvements in the health of the whole population, for the lasting benefit of individuals, society and the economy.
The guide has been written for anyone with an interest in people’s health and wellbeing. It will be especially useful to those new to the social determinants of health.
What is self-management support and why is it important?
Every day, people with long-term health conditions, their family members and carers will make decisions, take actions and manage a broad range of factors that contribute to their health. Self-management support acknowledges this and supports people to develop the knowledge, confidence and skills they need to make the optimal decisions and actions.
Most of the time, people manage their own health and wellbeing, rather than health professionals or services taking on this role. Health policy, and increasing evidence of positive outcomes, highlight the benefit of supporting people to manage their own health as effectively as possible. These benefits can be felt by people with long-term health conditions, health professionals, providers (both within and beyond the NHS) and commissioners.
Together with good quality clinical care, self-management support ensures that people receive the full range of support they need to manage the physical, emotional and social impact of their long-term health conditions at different stages and ages during their lives.
Self-management support is an important component of person-centred care, which has four principles.
- Affording people dignity, compassion and respect.
- Offering coordinated care, support or treatment.
- Offering personalised care, support or treatment.
- Supporting people to recognise and develop their own strengths and abilities to enable them to live an independent and fulfilling life.
Figure 1: The four principles of person-centred care

For people living with long-term health conditions, self-management support means:
- being active partners in determining outcomes that are important to them and how to achieve them, working in collaboration with health care professionals
- being supported to build knowledge, skills, confidence and resilience to manage the impact of their symptoms and limitations so they can live a full and meaningful life
- being enabled to access the support they need within and beyond health services to better manage their own health and wellbeing on an ongoing basis.
Effective self-management support requires changes across the whole system, from how services are regulated, planned, commissioned and provided, to how health professionals and people with long-term health conditions work together, and how people are supported in between appointments. It also requires these groups to work in partnership, with a common understanding of and commitment to self-management support.
Different technologies can support change, such as online consultations and self-monitoring, and are can also help people to self-manage and deliver services to support them.
Self-management support is important for the following reasons:
- People with long-term health conditions and their carers can enjoy a better quality of life, self-confidence and achieve the outcomes that are important to them.
- People with long-term health conditions experience better clinical outcomes.
- Professionals working in and beyond the NHS can have more meaningful conversations with people with long-term health conditions and greater impact from, and satisfaction with, their practice.
- Services can be delivered in a more ‘joined-up’ and cost effective way.
- Nationally, supporting self-management is part of implementing health and social care policies across the UK and the transformational change needed within our health care services.
Further reading
Self-management support – The Health Foundation person-centred care resource centre
A collection of resources on all aspects of self-management support http://personcentredcare.health.org.uk/person-centred-care/self-management-support
The key policy documents for England, Scotland, Northern Ireland and Wales that promote self-management support
The Five Year Forward View. NHS England www.england.nhs.uk/ourwork/futurenhs/
Gaun Yersel. Health and Social Care Alliance Scotland www.alliance-scotland.org.uk/resources/library/search/gaun+Yersel/
Living with Long Term Conditions: a policy framework. Department of Health, Social Services and Public Safety, Northern Ireland www.dhsspsni.gov.uk/index/long-term-condition.html
Long Term Conditions: changing for the better. NHS Wales www.wales.nhs.uk/sitesplus/863/opendoc/219791
Putting it into practice: an overview
New models of care draw on the principles of self-management support, where the key question shifts from ‘what is the matter with you?’ to ‘what matters to you?’ This can feel like a significant culture change.
The ‘House of Care’ was originally developed by the Year of Care partnership as a model for providing care and support for people living with diabetes. It has since been adapted and applied for all long-term health conditions.
As shown in Figure 2 overleaf, the House of Care depicts the shared responsibility across a health care system (commissioners, health care professionals, organisational processes and people with long-term health conditions) to deliver care and support planning, which is often seen as the gateway to identifying the self-management support needs that individuals have.
Figure 2: The House of Care, Coalition for Collaborative Care (C4CC)
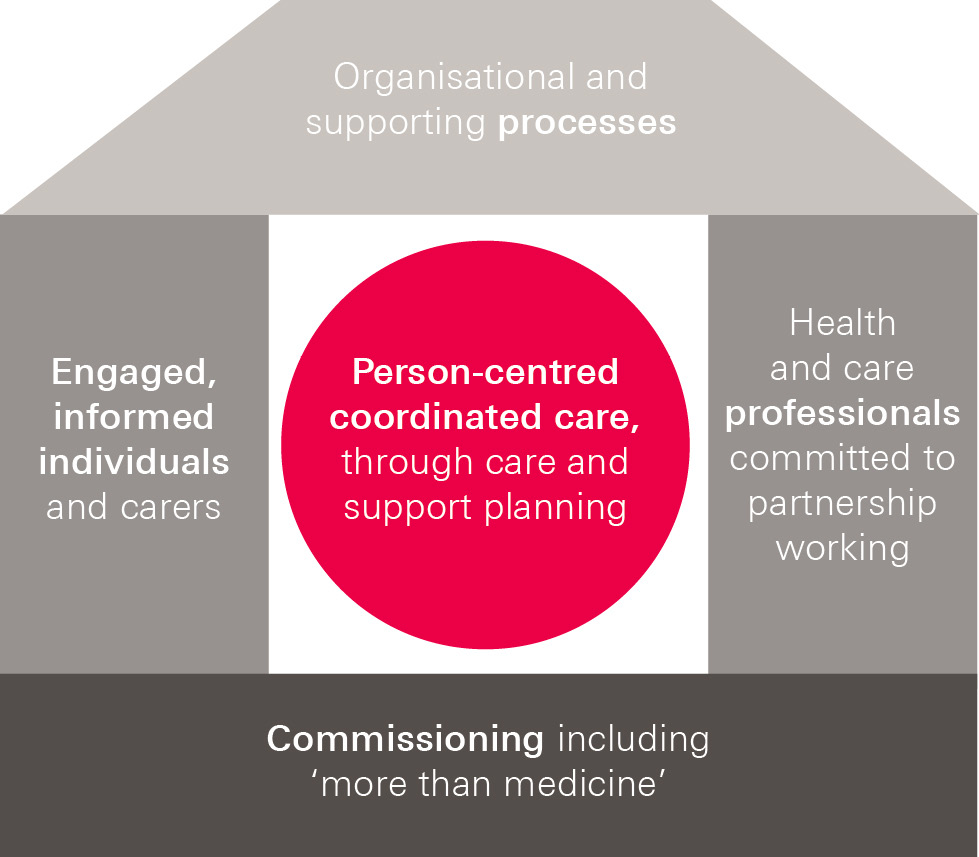
In the specific context of self-management support, this guide covers the following practical elements of the House of Care:
- Commissioning and planning that embeds self-management support within services and ensures that people have access to a range of support that complements their medical care (the floor or foundations of the House of Care).
- People with long-term health conditions and their carers are supported to develop the knowledge, skills and confidence to better manage their own health, for example through courses or coaching (one of the walls of the House of Care).
- Health and care professionals, health coaches and others who support people with long-term health conditions having the knowledge and skills for clinical tasks and collaborative consultations, which have been shown to be effective in supporting and enabling people to self-manage (another wall of the House of Care).
- Organisational systems and processes that enable support for people to self-manage and that help professionals to support them (the roof of the House of Care).
The effectiveness of self-management support depends on how the approach is implemented, rather than just the tools. Some key learning from people who have implemented self-management support is summarised in Figure 3.
Figure 3: Key lessons for implementing self-management support

Further reading
Building the House of Care. Health Foundation.
A case study exploring how Leeds and Somerset are implementing a coordinated approach for people with long-term conditions.www.health.org.uk/buildinghouseofcare
The House of Care Toolkit. NHS IQ
Developed in partnership with NHS England and Coalition for Collaborative Care to support implementing the House of Care at all levels www.nhsiq.nhs.uk/improvement-programmes/long-term-conditions-and-integrated-care/long-term-conditions-improvement-programme/house-of-care-toolkit.aspx
Coalition for Collaborative Care
Alliance of people and organisations committed to making person-centred care happen http://coalitionforcollaborativecare.org.uk/
Putting it into practice: planning and commissioning
Determining what services and support are needed to enable people to self-manage, and securing funding for those activities, can come from a variety of points within a local health economy. These include clinical commissioning groups (CCGs), Health Boards (in Scotland) and provider organisations, as well as national bodies.
The starting point to plan and commission self-management support is working collaboratively with people with long-term health conditions to understand the outcomes that are important to them and how these can best be achieved.
Outcomes-based commissioning has an emphasis on moving away from a system that focuses on payment for activity and instead focuses on commissioning outcomes that are meaningful to local people. When this is applied to commissioning self-management support, clinical outcomes are understood as contributory to the outcomes that are important to people – such as maintaining independence by staying active or in work. People generally need both clinical and non-clinical support to manage the different aspects of their conditions to achieve these broader outcomes. In practice, many outcomes-based commissioned contracts have relevant process measures, such as the number of people referred to a self-management programme or having a care plan.
There is no single approach to deciding what support to provide and how, but there are key components that could be considered.
- Specific self-management support services – these may be clinical or non-clinical services focusing on enabling people with long-term health conditions to self-manage. Examples include health coaching and structured group education programmes for people with long-term health conditions and their carers, or online programmes.
- Wider services – these recognise that people need support on an ongoing basis to maintain their skills and confidence to self-manage and to manage the wider social and lifestyle aspects of their health. Examples include services based in the voluntary and community sector such as walking groups and condition-specific peer support groups.
- Planning organisational processes – to facilitate services to work in a person-centred way. Examples include IT systems that ensure ‘informational continuity’ across a range of providers or enable telephone or Skype consultations, and a system-wide agreed care plan template.
- Providing training for workforces – to ensure people working in health care (from clinical professionals to non-clinical coaches or support workers) have the knowledge, skills and confidence needed to support people to self-manage.
There are a number of commissioning strategies that could be used to encourage providers to deliver self-management support. English commissioning levers include, for example, Commissioning for Quality and Innovation (CQUIN) payments, which enable commissioners to pay providers for local improvement initiatives. There are also national CQUINs that align with self-management support. Other English examples include the Quality Outcomes Framework (QOF), Better Together fund, and ‘direct enhanced’ GP services.
To commission on an outcomes basis, performance management and measurement systems would have a focus on evidence of outcomes as well as activity and costs. Tracking these kinds of outcomes is a new way of working for the NHS, and many outcomes-based commissioning schemes are having to set up new data collection systems to track progress.
Further reading
Thanks for the Petunias. Year of Care.
A guide to developing and commissioning non-traditional providers to support the self-management of people with long-term conditions www.diabetes.org.uk/upload/Professionals/Year%20of%20Care/thanks-for-the-petunias.pdf
Need to nurture: outcomes-based commissioning in the NHS. Health Foundation
Paper detailing the current shape of outcomes based commissioning in England www.health.org.uk/sites/default/files/NeedToNurture_1.pdf
Patients In Control: Commissioning to support self-management of long-term conditions. South East NHS Commissioning Support Unit
Details stages of commissioning, and key questions to ask at each stage http://participation.southeastcsu.nhs.uk/wp-content/uploads/2015/01/Commissioning-to-support-self-management.pdf
Putting it into practice: building knowledge, skills and confidence
When health care is designed to support self-management, people with long-term health conditions and their carers play a more active role in managing their own health. This can mean making difficult lifestyle changes. To do this, they need the knowledge, skills and confidence to manage not only their long-term health conditions but also the practical and emotional impact it has on their lives. When this happens, people enjoy life more, have less pain, have improved clinical outcomes and use health care services less.
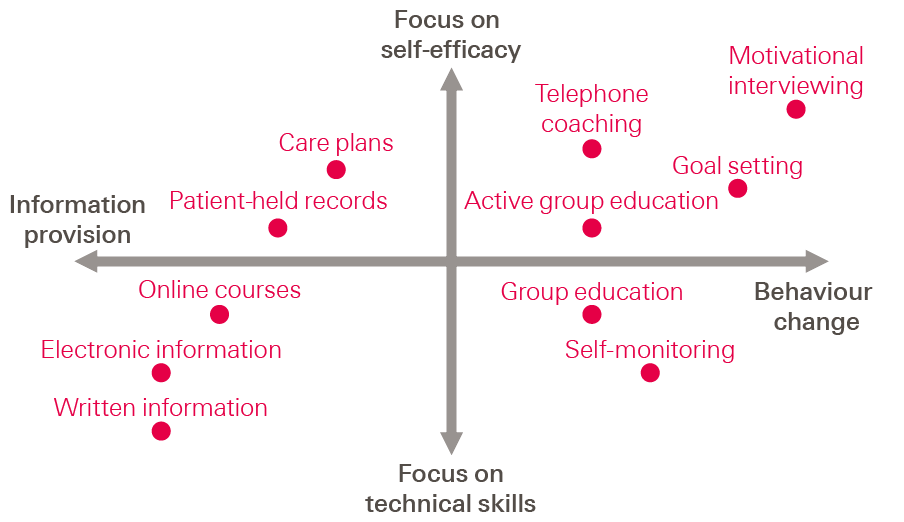
People with long-term health conditions can be given information to increase their knowledge, but that is often needed together with other forms of support to influence behaviour changes such as taking exercise or practising relaxation techniques. Some conditions require people to have technical skills, for example self-administering medication. Self-efficacy refers to people’s beliefs about their confidence and control over their own actions, which might include trying to find further support. All of these qualities can be important for people at different times. Figure 4 shows the strengths of different types of support in relation to the impact on behaviour change, access to information, technical skills and self-efficacy.
Figure 4: Continuum of strategies for self-management support
Common forms of self-management support
- Generic structured education courses: these focus on the common experiences of people with any long-term health condition and carers, such as working with health care professionals, coping with pain and managing fatigue. Examples include the Stanford Model, known as the Expert Patient Programme (EPP), and the Patient Skills Programme from the Health Foundation. These can be helpful in encouraging behaviour change.Example: Patient Skills Programme http://personcentredcare.health.org.uk/resources/patient-skills-programme
- Condition-specific structured education courses: these cover specific skills and knowledge needed to manage different conditions. Examples include the DAFNE (Dose Adjusted For Normal Eating) or DESMOND (Diabetes Education and Self-Management for Ongoing and Newly Diagnosed) courses for people with diabetes. These can be helpful in encouraging behaviour change and technical skills.Example: International Diabetes Federation Peer Leader Manual http://personcentredcare.health.org.uk/resources/peer-leader-manual
- One-to-one coaching: provided face-to-face, over the phone or via Skype, this uses reflective listening and motivational interviewing to support individuals with making changes through goal setting. This form of support focuses on improving self-efficacy and behaviour change. Example: Health Coaching by Medical Assistants to Improve Control of Diabetes, Hypertension, and Hyperlipidemia in Low-Income Patients: A Randomized Controlled Trial http://personcentredcare.health.org.uk/resources/health-coaching-medical-assistants-improve-control-of-diabetes-hypertension-and
- Websites: offering specific programmes or forums to help people understand their condition, access information or learn techniques like relaxation. The focus for this form of support is providing information.Example: The Pain Toolkit http://personcentredcare.health.org.uk/resources/pain-toolkit
- Recovery colleges: focusing on support for people with mental health conditions, these consist of a range of one-off workshops and longer courses, covering understanding of specific mental health conditions, the recovery model, or general skills such as mindfulness. Like the group courses detailed above, these focus on self-efficacy and behaviour change.Example: Briefing: Recovery colleges http://personcentredcare.health.org.uk/resources/briefing-recovery-colleges
Well-commissioned self-management support programmes for local people provide a range or combination of options that are appropriate to people’s needs and preferences, so people can choose what is best for them. In addition, support must be easily accessible – such as holding courses in the evening in non-health-related community venues.
Many people with a long-term health condition can benefit from different forms of self-management support. Some specific examples are given below.
- People with low confidence or self-esteem can benefit from the process of coaching or courses.
- People with mental health conditions can benefit from recovery colleges.
- Men of working age can benefit from activity based groups and one-to-one education.
- Carers can benefit from courses where they meet other carers and can manage the impact of their caring duties.
- Young people can benefit from accessing online support.
- People from different ethnic backgrounds may benefit from culturally led support.
It is important to be aware that the groups highlighted above are often among those least likely to know about available support. Therefore, comprehensive recruitment strategies would include raising awareness among professionals, voluntary groups, local community, housing or social groups.
Much of this support might be provided outside of a traditional consultation between a health care professional and someone with a long-term health condition. However, all of these types of support are strengthened when backed up by professionals using skills such as motivational interviewing, goal setting and problem solving in consultations.
Facilitators and coaches for self-management can be people with long-term health conditions and health care professionals or other trained individuals. Courses with a strong clinical focus may be co-delivered with a health care professional.
Markers for quality, detailed in national guidelines, include the training and supervision of people providing courses and coaching, evidence-based content, outcome audits and provision of supporting material. These must include outcomes for participants and operational effectiveness.
Without ongoing support, people’s knowledge, skills and confidence to self-manage decline over time. Many programmes therefore include creating peer support groups for people completing courses, and at the very least they can enable people to connect with peers and other forms of ongoing support.
Further reading
Example case studies:
- My Health My Way. Dorset NHS
A comprehensive self-management support service, providing coaching, courses and peer support www.myhealthdorset.org.uk
- Recovery college: From mental health patient to recovery student. Health Foundation.
A short film showing a recovery college in action.www.health.org.uk/recovery-college
Supporting Self-Management. National Voices.
A summary of the evidence of the programmes to support people with long-term health conditions www.nationalvoices.org.uk/sites/www.nationalvoices.org.uk/files/supporting_self-management.pdf
Wellbeing Our Way. National Voices.
A programme looking at community and voluntary groups supporting self-management www.nationalvoices.org.uk/engagementprogramme
Standards for Health Management Programmes and Interventions. QISMET.
The national body for quality assurance of self-management education interventions http://qismet.org.uk/certification/
Putting it into practice: peer support and community assets
People with long-term health conditions and their carers often experience further challenges that have an impact on their health, such as social isolation. There is an increasing body of evidence demonstrating the benefits of peer support and community groups in combating isolation and helping people sustain their knowledge, confidence and skills over time.,
The key types of peer and community support are as follows:
- Encouraging and enabling self-management behaviours. This type of support enables people to learn new skills or share practical experiences in ways that create mutual support between people with similar problems. It helps people to develop and maintain the skills and motivation they need to manage their health in the context of their everyday life. Examples include walking groups or condition-specific support groups.
- Providing social and emotional support. This type of support may or may not centre on peers with similar experiences or conditions, but can normalise the rollercoaster of emotions that living with a long-term health condition entails. Examples include online forums or lunch clubs.
- Supporting people to address wider social and lifestyle aspects of their health. This type of support can help people develop health behaviours, reduce isolation, develop a sense of belonging, and cope with some of the broader social determinants of health. Examples include craft classes and advice on employment and finances.
All of this support can be provided by people with long-term health conditions, in volunteer or peer roles, which can also have a positive and direct impact on their own health and self-management confidence.
Peer and community support is beneficial because it can:
- help people to maintain the knowledge, skills and confidence to self-manage
- be available to people ‘on demand’, when they need it
- support non-clinical aspects of health, such as loneliness and confidence
- be tailored, so people can access support for what is important to them and suits them.
To get the best out of peer and community support, there needs to be a wide and appropriate range of support available to people, that is routinely integrated into the health care system and care pathways. Approaches often include providing a single point of access to a range of options, such as the examples below.
- Social prescribing – the health care professional and person identify together the type of activities that will be of benefit, with the professional writing a ‘prescription’ directly to a service or referring the individual to an intermediary, such as a link worker, with whom a package of services can be constructed.
- Signposting – this acts as a bridge between health care professionals and the social activities available, and can be done by a variety of people including health trainers, wellbeing coaches, navigators, and voluntary community services networks.
Further reading
I have never had a patient tell me medicine changed their life. Ollie Hart, C4CC
A blog by a GP discussing the impact of peer and community support for their patients http://coalitionforcollaborativecare.org.uk/gp/i-have-never-had-a-patient-tell-me-medicine-changed-their-life/
More Than Medicine. Nesta.
A detailed report on social interventions that complement clinical care www.nesta.org.uk/sites/default/files/more_than_medicine.pdf
Developing the power of strong inclusive communities. Think Local Act Personal.
Background to community development and support www.thinklocalactpersonal.org.uk/_library/Resources/BCC/Report/TLAP_Developing_the_Power_Brochure_FINAL.pdf
Peers For Progress
International organisation promoting best practice in peer support http://peersforprogress.org/
Putting it into practice: workforce development
Self-management support involves a cultural shift in how we understand the roles, responsibilities and relationship between people living with long-term conditions and the health and social care professionals and others who support them.
All practitioners can use the skills and approaches of self-management support in their practice. For health professionals, it means not only providing clinical care, but helping people to think about their strengths and abilities, identifying their information needs and the changes they can make in their lives to take control, reach their goals and maintain their health and wellbeing.
The tools that provide a structure to achieve this are as follows:
- Care and support planning: helps people set their own aims, then plan the support and care needed to achieve them.
- Collaborative agenda setting: at the start of the consultation, the practitioner and the person talk about and agree the health issues to explore and the problems to solve.
- Recognising and exploring ambivalence: practitioners can explore people’s readiness to change, then respond accordingly.
- Goal setting, action planning and follow-up: the practitioner supports the person to identify a goal they want to achieve and break this down into small achievable actions. Following up goals later involves developing problem-solving skills and exploring solutions to barriers, as well as positive affirmation of progress and effort.
All of these approaches are underpinned by the use of core communication skills that build relationships of trust and rapport. These skills include: open-ended questioning; reflection; empathy; affirmation and normalisation; summarising; signposting; active listening and non-verbal communication. Further skills include health coaching approaches and helping people to explore the importance to them and their confidence of making changes.
Approaches can also be adapted to reflect each person’s level of knowledge, skills and confidence around managing their health condition.
Organisations have an important role in supporting their practitioners to develop and use these skills and embed them into practice. This means providing training and ongoing support and adapting systems and processes. Elements of self-management support are now part of revalidation criteria for doctors.
All members of a team (such as GPs, nurses and practice receptionists) can benefit from training. Training whole teams or workforce groups together is key to:
- ensuring common understanding of self-management support and core tools and techniques
- creating a common language and culture
- creating a critical mass of trained practitioners within a team or service to put the skills into practice across a service or organisation
- improving the ease with which self-management support can be tested and adopted
- enabling practitioners to support each other through the training and later when using the skills in practice.
A combination of face-to-face, role modelling and e-learning teaching methods can be used. Ongoing support to maintain new skills and behaviours within a team can include action learning sets, community interest groups and refresher training, having a senior lead or champion, and building it into supervisions and team meetings. Train the trainer programmes and including elements in organisation induction programmes for new staff can help the sustainability of training schemes.
Further reading
Example case study: Cambridgeshire NHS Trust training
This sets out the experiences of one NHS organisation delivering training in self-management support http://personcentredcare.health.org.uk/sites/default/files/resources/sms_case_study_care_planning_training_cambridge.pdf
Practitioner Development Programme. Health Foundation.
This distils evidence about what works into a clear set of practical tools that clinicians, health coaches and others can learn and use to support people to self-manage http://personcentredcare.health.org.uk/resources/practitioner-development-programme
Agenda setting sheets. Health Foundation person-centred care resource centre
A range of sample agenda setting sheets for people with long-term conditions before appointments http://personcentredcare.health.org.uk/resources?search_api_views_fulltext=agenda&f[0]=field_area_of_care%3A364
Practitioner development. Health Foundation person-centred care resource centre
Collection of resources from a range of sources supporting practitioner development http://personcentredcare.health.org.uk/person-centred-care/self-management-support/implementing-self-management-support/practitioner
The Health Coaching Experience in NHS Midlands and East Health Coaching Review
Review of evidence of large-scale training in self-management skills for health care professionals http://pcc-cic.org.uk/sites/default/files/articles/attachments/dr_penny_newman_the_health_coaching_experience_in_nhs_midlands_and_east_0.pdf
Sustaining and spreading self-management support. Health Foundation.
Lessons from the evaluation of the second phase of the Co-creating Health project www.health.org.uk/sites/default/files/SustainingAndSpreadingSelfManagementSupport.pdf
Putting it into practice: optimising systems and processes
Changes which enable people to self-manage can be made at every level, from what is commissioned to IT systems and individual interactions with people with long-term health conditions. Examples include the following:
- Developing care pathways to create better links and referrals between statutory, voluntary and community sectors. For example, the ALISS project is a co-produced library that can be added to by anyone and is designed to make information about local sources of support easier to access.
- Providing services in different ways. This could be through support groups, emails, text messages, and telehealth, to provide ongoing support between face-to-face appointments. For example, the telehealth service in Newham combines different levels of support for people with a range of conditions via virtual education and symptom monitoring.
- Improving processes to enable people to play a more active role. This could involve providing agenda setting sheets, that help people to think through what they want to get from an appointment; and providing people with test results in advance of the consultation, so they prepare questions in advance.
- Refining IT systems and developing processes to support health care professionals. For example, in Ayrshire and Arran many GPs use the same system so they have developed a ‘tag’ for the records of people with COPD to prompt the GP to check if they have been offered a self-management programme.
Assessing readiness to change and commitment to supporting self-management within an organisation or team is important, and can be done using tools such as the Robert Wood Johnson Foundation assessment. Collaborative working between commissioners, service managers, professionals and people with long-term health conditions enables a shared understanding of challenges and identification of potential solutions.
Embedding processes that support self-management takes place gradually. Having clear goals, encouraging small changes, evaluating the impact of changes and making tweaks to processes as often as necessary before widespread implementation is important. There are a number of different quality improvement tools to support this, such as the Plan, Do, Study, Act cycle (PDSA). The process needs to include effective involvement of people with long-term conditions in the generation of ideas and design phases. This process will help to engage workforces at all levels, encourage ‘buy-in’ and a sense of ownership, and drive cultural change. In the longer term, it is important to evaluate the effectiveness of services and any changes made to assess how well they are meeting people’s needs.
Further reading
Patient and Family Centred Care Toolkit.
The King’s Fund.
Step-by-step guide to understanding people’s experiences of care and what needs to change www.kingsfund.org.uk/projects/pfcc
Quality improvement made simple.
Health Foundation.
A quick guide covering different QI approaches www.health.org.uk/sites/default/files/QualityImprovementMadeSimple.pdf
Co-producing services – co-creating health. 1000 Lives Wales Report from Welsh project sharing learning www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/T4I%20(8)%20Co-production.pdf
Patient Leadership: the start of a new conversation. National Voices.
Introduction to Patient Leadership and co-production of change www.nationalvoices.org.uk/sites/www.nationalvoices.org.uk/files/patient_leadership_briefing_note_0.pdf
Ideas into action: Person-centred care in practice. Health Foundation.
Summary of key learning points from self-management implementation www.health.org.uk/sites/default/files/IdeasIntoActionPersonCentredCareInPractice.pdf
Putting it into practice: measurement and evaluation
Effective measurement and evaluation of self-management support can provide evidence of impact and insight into potential improvements. This can be done at the individual level, service and organisational level, and commissioning and planning level, taking into account what is important at each level. Measurements from different levels can be combined to provide a complete picture of the effectiveness of self-management support. Although tricky, there are emerging resources that can help with measuring what really matters.
Individual level
Developing an understanding of individuals’ experiences and their desired outcomes enables tailored support to be delivered to people with long-term health conditions. This takes into account people’s sense of wellbeing, quality of life, disability, emotion, sense of social support and their confidence to self-manage. Clinical outcomes are also important, such as biomedical disease markers and medication usage.
A range of tools exist to measure this, such as:
- Patient Activation Measure (PAM)
- Health Education Impact Questionnaire (HEIQ)
- Patient Reported Outcome Measures (PROMs)
- Person Centred Outcome Measures (PCOM) or Personally Determined Outcome Measures (PDOMs).,
Qualitative approaches such as surveys and interviews with service users can also be effective, alongside emotional touch points and narratives. A combination of these can be best as it can be challenging to find a measure that captures everything related to the individual.
Service and organisational level
Measures at the individual level can be aggregated with service data to provide detail on where and how improvements can be made. This focuses on service users’ access to timely and appropriate services and outcomes for workforces such as job satisfaction and rates of sickness absence.
Measurement tools include:
- Consultation and Relational Empathy (CARE) Measure
- Person-Centred Care Assessment tool
- Health Literacy Questionnaire.
Observing clinical encounters and service user-led ‘mystery shopping’ can also provide insight into these areas.
Commissioning and planning level
Focusing at a population level, outcomes for local people, impact of local services and associated cost-effectiveness can be incorporated. This understanding can help commissioners support current services and develop new services to effectively promote self-management support.
Informed by meaningful involvement of people with long-term health conditions, measurement and evaluation can help create insight to drive changes to support self-management as effectively and efficiently as possible.
Traditional measurement and evaluation commonly focus on activity and clinical outcomes, with little consideration of what people with long-term health conditions think is important. Person-centred outcomes can be complex to design and measure, but working together with people with long-term health conditions to co-design measurement and evaluation approaches will ensure a person-centred focus.
Further reading
Helping measure person-centred care. Health Foundation.
An in-depth summary of the evidence, techniques and strategies for measuring person-centred care www.health.org.uk/sites/default/files/HelpingMeasurePersonCentredCare.pdf
Evaluation: what to consider. Health Foundation.
A quick guide to support evaluation www.health.org.uk/sites/default/files/EvaluationWhatToConsider.pdf
Measuring what really matters. Dr Alf Collins.
Thought paper on the challenges and opportunities of measuring person-centred care www.health.org.uk/sites/default/files/MeasuringWhatReallyMatters.pdf
References
- The Health Foundation. Person-centred care made simple. London: The Health Foundation, 2014.
- National Voices. Prioritising person-centred care: supporting self-management – summarising evidence from systematic reviews. London: National Voices, 2014. www.nationalvoices.org.uk/sites/www.nationalvoices.org.uk/files/supporting_self-management.pdf
- Kidd L, Lawrence M, Booth J, Rowat A and Russell S. (in press) Development and evaluation of a nurse-led, tailored stroke self-management intervention. BMC Health Services Research.
- Coulter A, Roberts S, Dixon A. Delivering better services for people with long-term conditions. London: The King’s Fund, 2013. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf
- NHS England. Five Year Forward View. London: NHS England, 2014. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
- Year of Care Partnership. Year of Care: Report Findings from the pilot programme. Year Of Care, 2011. www.yearofcare.co.uk/sites/default/files/images/YOC_Report%20-%20correct.pdf
- Coulter A, Roberts S, Dixon A. Delivering better services for people with long-term conditions. London: The King’s Fund, 2013. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf
- Coalition for Collaborative Care. House of Care. Accessed via: http://coalitionforcollaborativecare.org.uk/aboutus/house-of-care/
- The Health Foundation. Ideas into action: person-centred care in practice. The Health Foundation, 2014. www.health.org.uk/sites/default/files/IdeasIntoActionPersonCentredCareInPractice.pdf
- de Silva D. Helping people help themselves. The Health Foundation, 2011.
- Chronic Disease Self-Management Program, Stanford Patient Education Research Centre. http://patienteducation.stanford.edu/programs/cdsmp.html
- Patient Skills Programme, Co-Creating Health, The Health Foundation. http://personcentredcare.health.org.uk/resources/patient-skills-programme
- Dose Adjustment for Normal Eating (DAFNE) www.dafne.uk.com/
- Diabetes Education and Self Management for Ongoing and Newly Diagnosed. (DESMOND) www.desmond-project.org.uk/
- Does Health Coaching Work? The Evidence Centre, NHS East of England http://personcentredcare.health.org.uk/resources/does-health-coaching-work
- Recovery Colleges: A briefing, IMRoc. www.recoverydevon.co.uk/download/IMRoc_Briefing_Recovery_Colleges_final.pdf
- Galdas P, Fell J, Bower P, Kidd L, Blickem C, McPherson K, Hunt K, Gilbody S, Richardson G. The effectiveness of self-management support interventions for men with long-term conditions: a systematic review and meta-analysis. BMJ Open 2015;5:e006620. March 2015. http://bmjopen.bmj.com/content/5/3/e006620.full
- NHS IQ and RCGP. Carers case study. NHS IQ and RCGP, October 2014 www.nhsiq.nhs.uk/media/2563726/carers_case_study_-_tailored_service_middlesborough_and_stockton.pdf
- Macmillan Cancer Support. Self-Management Support For Cancer Survivors: Guidance For Developing Interventions. Macmillan Cancer Support, 2010. www.ncsi.org.uk/wp-content/uploads/Guidance-for-Developing-Cancer-Specific-Self-Management-Programmes.pdf
- QISMET. QIS2012 The Standard for Health Management Programmes and Interventions. QISMET, 2012. http://qismet.org.uk/files/7413/8511/2401/QIS2012_Standard_HMPAI_FINAL_20_04_12_1.pdf
- Newbronner L, Chamberlain R, Borthwick R, Baxter M, Sanderson D. Sustaining and spreading self-management support: Lessons from Co-Creating Health phase 2. London: The Health Foundation, 2013. www.health.org.uk/sites/default/files/SustainingAndSpreadingSelfManagementSupport.pdf
- Nesta. More than Medicine: new services for People Powered Health. London: Nesta, 2013. www.nesta.org.uk/sites/default/files/more_than_medicine.pdf
- Nesta and National Voices. Peer Support: What is it and does it work? London: Nesta and National Voices, 2015.
- Big Lottery Fund. Well-being: The impact of volunteering (Research and Learning Factsheet). Big Lottery Fund.
- National Voices. Care and Support Planning Guide. National Voices. www.nationalvoices.org.uk/sites/www.nationalvoices.org.uk/files/guide_to_care_and_support_planning_final_plainer_version.pdf
- GMC. The Good Medical Practice Framework For Appraisal and Revalidation. Manchester: GMC, 2013. www.gmc-uk.org/static/documents/content/The_Good_medical_practice_framework_for_appraisal_and_revalidation_-_DC5707.pdf
- The Health Foundation. Sustaining and Spreading Self-Management Support: Lessons from Co-Creating Health phase 2. London: The Health Foundation, 2013. www.health.org.uk/sites/default/files/SustainingAndSpreadingSelfManagementSupport.pdf
- A Local Information System for Scotland. www.aliss.org/
- The Health Foundation. Spotlight on diabetes and person-centred care http://personcentredcare.health.org.uk/node/271422 (Click on Telehealth in Newham)
- The Health Foundation Person-centred care resource centre. Developing the way the team works. http://personcentredcare.health.org.uk/person-centred-care/self-management-support/implementing-self-management-support/improving-system-11
- Robert Wood Johnson Foundation. Assessment of Primary Care Resources and Supports for Chronic Disease Self Management (PCRS)-UK version. March 2006. http://personcentredcare.health.org.uk/sites/default/files/resources/primary_care_assessment_tool.pdf
- Wood S, Sieff A. Embed person centred care into mainstream health services. Health Services Journal. November 2014
- Hibbard J, Gilburt H. Supporting people to manage their health: An introduction to patient activation. London: The King’s Fund, 2014. www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/supporting-people-manage-health-patient-activation-may14.pdf
- Osborne R, Elsworth G, Whitfield K. The Health Education Impact Questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns. 2007;66(2):192–201. www.ncbi.nlm.nih.gov/pubmed/17320338
- Nelson E, Eftimovska E, Lind C, Hager C, Wasson J, Lindblad S. Patient reported outcome measures in practice. BMJ. 2015;350:g7818. www.bmj.com/content/350/bmj.g7818
- NHS IQ. Person centred outcomes. NHS IQ www.nhsiq.nhs.uk/improvement-programmes/experience-of-care/person-centered-outcomes.aspx
- Cook A, Miller E. Talking points: Personal outcomes approach: practical guide. Joint Improvement Team, Scotland, 2012. www.jitscotland.org.uk/resource/talking-points-personal-outcomes-approach-practical-guide/
- Glasgow University and Edinburgh University. Consultation and Relational Empathy Measure (CARE). www.caremeasure.org/
- Edvardsson D, Fetherstonhaugh D, Nay R, Gibson S. Development and initial testing of the Person-centred Care Assessment Tool (P-CAT). International Psychogeriatrics. 2010;22(1):101–8.
- OPHELIA www.ophelia.net.au/hlq