Acknowledgements
The authors would like to express their gratitude to those who gave up their time to support this work. This paper would not have been possible without Jo Bibby, who conceived the original idea for this work and provided invaluable thought leadership throughout.
Thanks also to our advisory group, those who peer reviewed this work and colleagues at NHS England and NHS Improvement for providing thoughtful comments on early drafts of this report. We would also like to thank colleagues at the Health Foundation for their support and guidance during the research and production of this report, including Ruth Thorlby, Ben Gershlick, Laura Wallace, Josh Kraindler, Yannish Naik and Tim Horton. Errors and omissions remain the responsibility of the authors alone.
This work draws on research by CLES and The Democracy Collaborative, funded by the Health Foundation, and we would like to thank Neil McInroy, Frances Jones, Tom Lloyd Goodwin, Ted Howard and Katie Parker for their collaboration throughout.
Executive summary
What this report is about and why it matters
Widening health inequalities and growing pressures on health care services have prompted a fundamental conversation about the role of the NHS in prevention and its broader influence in local communities. The British economy is one where wages and living standards are stagnating and 22% of the population live in poverty. People from the most socially deprived areas of England die nearly a decade earlier and spend 18 fewer years in good health than people born in the least deprived areas. And while health care services on their own are insufficient to overcome these inequalities, the NHS could make a far greater contribution to this goal: it is the largest employer in the country, spends billions on goods and services each year and controls significant land and physical assets – all of which make it a powerful ‘anchor institution’.
Anchor institutions are large, public sector organisations that are called such because they are unlikely to relocate and have a significant stake in a geographical area – they are effectively ‘anchored’ in their surrounding community. They have sizeable assets that can be used to support local community wealth building and development, through procurement and spending power, workforce and training, and buildings and land.
Anchors have a mission to advance the welfare of the populations they serve. They tend to receive (or are significant stewards of) public resources, and often have a responsibility to meet certain standards on impact or value. These characteristics mean that the NHS, like other anchors, is well placed to have a powerful voice in where and how resources are spent locally. The NHS can also lead by example, and help spread and champion the principle of anchor institutions in local economies.
The idea of anchor institutions is not new. In the UK, however, other public sectors (such as local government and universities) have arguably been more conscious of their role as anchors., There are signs that this is changing; there is growing enthusiasm across the NHS for how health care organisations make up a key part of the social and economic fabric of communities, and can do more to channel their strategic influence to improve population health.
This report explores how NHS organisations act as anchor institutions. It gives examples of what anchor practices look like in a health care context, and how anchor institutions can maximise their influence on the wider determinants of health, as follows.
- Chapters 1 and 2 introduce the concept of anchor institutions and set out the case for change.
- Chapter 3 discusses employment, and how the NHS can widen access to quality work for communities furthest from the labour market, and be a better employer and place to build a career for more local residents.
- Chapter 4 looks at how procurement and commissioning can derive greater social value by shifting more NHS spend locally and towards organisations that provide greater community benefit.
- Chapter 5 considers how the NHS can make better use of its capital and estate by supporting the development of community assets like affordable housing and creating community spaces for local groups and businesses.
- Chapter 6 looks at how the NHS can promote environmental sustainability in its own operations and in the broader community.
- Chapter 7 discusses how the NHS can accelerate progress and impact at scale by working more effectively as a partner across a place, both within its own structures and with other anchor institutions in the local economy.
The central argument of this report
The size, scale and reach of the NHS means that it has a significant influence on the health and wellbeing of local populations. But how it chooses to function and leverage its resources will determine the extent of that impact. More can be done to support and challenge the NHS to embrace its role as an anchor institution and maximise the social and economic value it brings to local communities.
There are a range of promising anchor activities taking place across the NHS that provide an important foundation from which to advance progress. Though NHS organisations are all in very different stages of their role as anchors, where anchor practices are happening, they tend to be discrete, narrow in scope and not intentionally applied or integrated into central and local systems or organisational strategies. Nor are anchor approaches being evaluated in any systematic way to know where to prioritise efforts and what actions are likely to have the greatest impact on population outcomes.
There are opportunities at each level of the system to help the NHS more consciously adopt an anchor mission and to understand the impact of different approaches so that they become a central part of how NHS organisations function.
Considerations for practice and policy and taking it forward
Supporting NHS organisations to embrace their anchor mission is key to harnessing the NHS’s powerful influence on community health and wellbeing. While NHS organisations face many immediate pressures that can make it difficult to adopt anchor strategies, the examples in this report show how parts of the NHS are taking a pragmatic approach and aligning anchor practices with other strategic objectives. While most change will be delivered at the organisational level, there is a key role for local system, regional and national leaders to help scale approaches, cultivate an anchor mission and support an environment where these practices become an embedded part of how the NHS operates.
This report draws on examples of promising practice and identifies key opportunities to help NHS organisations meet their potential as anchor institutions, regardless of the area of anchor activity being pursued (summarised in Table 1 below). We also surface some of the key tensions that may have to be worked through to balance priorities and direct efforts along an anchor mission, and present some examples of where practices have overcome them. These are summarised in Table 3 and discussed in more detail throughout the report. The report proposes key actions for national and regional policymakers, local system leaders, and NHS providers and networks to help the NHS advance its role as an anchor institution.
Table 1: Steps towards realising the NHS’s potential as an anchor institution
|
Figure 1: What makes the NHS an anchor institution?
Chapter 1: Introduction
It is increasingly accepted that good health is shaped by the conditions in which people live, learn, work and age, with access to clinical care playing an important but more minor role.,,,,,,, In addition to its core purpose of delivering health care services, the NHS has the potential to influence these conditions: it is the largest employer in the UK, spends billions on goods and services each year and controls significant land and physical assets – all of which give it enormous economic clout in local communities. Through its scale, size and relationship with local populations, the NHS represents a powerful ‘anchor institution’ that can positively influence the social, economic and environmental factors that help create good health in the first place.
The idea of anchor institutions is not new. Until now, though, it has mainly been local government and universities that have more consciously recognised their role as anchors., There are signs that this is changing. The NHS Long Term Plan promised to explore the potential of the NHS as an anchor institution and identify examples of NHS initiatives that have benefited their surrounding communities. But how the health service chooses to operate and leverage its resources will determine the extent of that impact. Questions remain as to how the NHS can best be supported and challenged to think differently about the social and economic value it brings to local populations.
This report explores how NHS organisations act as anchor institutions in five areas:
- employment
- procurement and commissioning for social value
- use of capital and estates
- environmental sustainability
- as a partner across a place.
It showcases where NHS organisations are already implementing anchor practices, and discusses opportunities for how practice and policy can evolve to maximise the NHS’s contribution to local communities.
What are anchor institutions?
The term anchor institution gets used in different ways, but for the purposes of this report we are referring to large, public sector organisations that are unlikely to relocate and have a significant stake in a geographical area. Anchors have sizeable assets that can be used to support local community wealth building and development, through procurement and spending power, workforce and training, and assets such as buildings and land. Anchors have a mission to advance the welfare of the populations they serve. They tend to receive (or are significant stewards of) public resources, and often have a responsibility to meet certain standards on impact or value. These characteristics mean that the NHS, like other anchors, is well placed to have a powerful voice in where and how resources are spent. The NHS can also lead by example and help spread and champion the principles of anchor institutions in local economies.
Our approach
This report draws on a number of workstreams, including the following.
- Research commissioned by the Health Foundation and produced by the Centre for Local Economic Strategies (CLES) and The Democracy Collaborative (TDC), which included a review of evidence on the role and impact of anchor institutions, as well as three case studies: University Hospitals Birmingham NHS Foundation Trust, Leeds Teaching Hospitals NHS Trust and East Lancashire Hospitals NHS Trust.
- Interviews about existing practice from a range of perspectives, including the acute sector, community and mental health trusts, primary care, clinical commissioning groups (CCGs), research, policy and local government. Interviewees included leads for transformation, sustainability, purchasing, public health, partnerships, estates and workforce.
- Workshops with an expert advisory group to identify the greatest opportunities for progress. Participants included representatives from acute trusts, local government, national bodies, academia, primary care, commissioners and the voluntary sector.
For each of the five areas (employment, procurement, capital and estates, environmental sustainability and partnerships), we explain why it matters, provide examples of what anchor practices look like in the NHS and briefly explore the policy context. We conclude with a summary of implications for practice and policy moving forward.
Chapter 2: Setting out the case for change – the role of the NHS in a local place
There is increasing concern about inequalities in different parts of the UK where the conditions for living life in good health are poor and deteriorating. Across England, wages, living standards and productivity are stagnating and more than one in five people (22%) now live in poverty. Poverty represents a profound economic and social loss to the UK: the British economy spends an estimated £78bn pounds dealing with the effects of poverty. People living in poverty are more likely to have poor health, and this is reflected in persistent inequalities in health outcomes.
People born in the most deprived 10% of local areas in England are expected to die nearly a decade earlier and have 18 fewer years in good health. While these inequalities are primarily driven by broader factors that sit outside the health system, there are several reasons why the NHS should and can play a stronger role in supporting their reduction.
The protection of health care spending relative to other parts of the public sector since 2011 creates a moral case for maximising the value and reach of NHS funding to improve population health and wellbeing. Health care accounted for 30% of public service spending in 2016/17 compared to 26% in 2009/10 and 23% in 1999/2000, and budget reductions to local government have put both public health and social care services under severe pressure.
There is also an instrumental argument: even if the root causes of poor health and health inequalities are primarily driven by factors outside the control of the health sector, it is the NHS that deals with many of the consequences. It faces increased demand from preventable behavioural and socioeconomic causes, and it is therefore logical to extract the most value from the NHS in its wider role within local communities.
Thinking of the NHS in this wider role goes with the grain of policy both in England and across the UK. The 2014 NHS Five Year Forward View demanded a ‘radical upgrade in prevention’, with the 2019 NHS Long Term Plan expanding on this to set out a strategy to strengthen the NHS’s contribution to tackling health inequalities and improving population health. The government’s Green Paper on prevention set out proposals to make progress on their ambition to extend healthy life expectancy in the UK by five years by 2035, (though the proposals have been criticised for not going far enough to narrow the inequalities between the richest and poorest needed to achieve this aim). Wales and Scotland have already adopted cross-government approaches to improving health and wellbeing, placing duties on public bodies to take action to tackle the socioeconomic conditions that widen inequalities.,
Since 2016, health policy in England has also encouraged the NHS to plan and deliver services in collaboration with other bodies locally. Sustainability and transformation partnerships (STPs) and the emerging integrated care systems (ICSs) bring the NHS and local government together to design and deliver services to meet local population needs from a common pool of resources. Though still very much under development, the promise of these partnerships is that the NHS may have more scope to establish and work towards common goals with sectors like housing, education and employment. In Scotland and Wales, health and social care are further integrated and NHS bodies have greater flexibility to work together to develop new approaches to improve population health.
Supporting inclusive economies
There is a growing synergy between the place-based lens of the NHS and broader policy that emphasises localism in shaping the socioeconomic environments in which we live.
The idea of inclusive economies – enabling all communities to benefit and contribute to economic success – has garnered significant attention nationally and internationally over the past decade. This is partly due to a recognition that economic growth has often failed to ‘trickle down’ and alleviate poverty or increase living standards across all communities as expected. In England, growth has been concentrated in London and the South, with other parts of the country falling significantly behind.
Inequalities and deprivation threaten long-term economic stability as many people become trapped in low-productivity work or are excluded from the benefits of growth altogether., Local leaders have therefore increasingly turned to anchor institutions to create the conditions needed to support a healthy population, and help tackle inequalities while boosting economic growth. Devolution and the subsequent creation of local enterprise partnerships (LEPs) and local industrial strategies have been promoted as ways of giving more power to local communities. Though an emergent area of policy, these agendas are seen as an opportunity to bring economic players together across a place to drive productivity and distribute growth more fairly across the country – although whether these policies will lead to a narrowing of inequalities remains to be seen., There is an inherent risk that increased localism could even widen socioeconomic divides if already advantaged places are better positioned to leverage local resources and capacities for the benefit of residents. This makes it ever more important to consider the distinct role that health sector organisations play as anchors in local communities, given that the NHS exists everywhere and carries with it significant assets that can be channelled for public good.
The NHS is a key part of the social and economic fabric in all communities, and as an anchor is well placed to work with other sectors to support place-based approaches that promote prosperity and create the foundation for healthy communities. There is growing recognition that health systems have an important and positive impact on economies, and can improve health and wellbeing (directly and indirectly) through the size and nature of their role., However, the complexities of the NHS have often meant that health care organisations have acted as institutional siloes, often looking upwards to regulatory bodies more than outwards to their community for direction and to drive change. But given the economic challenges the UK is facing and the recent focus on localism, there is now a key opportunity for the NHS to work with other local leaders to develop a common agenda and support economic strategies that improve the socioeconomic conditions of local communities. This goal is important not only for building more inclusive economies, but for the NHS itself; by more consciously leveraging its resources and actions, the health sector can have even greater strategic influence across a place and be part of broader conversations that improve the context in which it works.
Learning from anchor practices
In the chapters that follow, we set out examples of anchor practices in a health care context to show how the NHS can leverage its assets to maximise its influence. These examples come from the grey literature and interviews, highlighting existing anchor practices in the NHS and what it might take to broaden their impact.
There are many ways of considering how the NHS functions as an anchor institution. We restrict our focus to examples related to five key areas: employment, procurement and commissioning, capital and estates, environmental sustainability and working in partnership across a place. Many of the examples involve provider trusts, because of their relatively large size. This should not be taken to imply that other parts of the NHS cannot function as anchor institutions, or have less scope or responsibility to intervene in the social determinants of health. Indeed, the formulation of primary care networks (PCNs) in England may create new opportunities to work at scale and implement anchor strategies in primary care. While most actions will take place at the level of the organisation, the report discusses how local system and regional/national NHS leaders can help create an environment in which NHS organisations more fully embrace their anchor mission and maximise their contribution to local economies. We focus primarily on England, given its different context and recent opportunities, and given that the other countries of the UK are making more progress in some areas.
Based on our findings, we conclude by suggesting actions at each level of the health and care system, including by national and regional policymakers, by local system leaders (that is, STPs and ICSs) and by local NHS providers or networks.
* Announced in 2010, LEPs are private-sector-led partnerships between local businesses and local public sector bodies. Their aim is to help set local economic priorities and undertake activities to drive local economic development and job creation. LEP boards are led by a chairperson from local businesses, with board members drawn from local industry, educational institutions and the public sector.
Chapter 3: The NHS as an employer
Why this matters
The NHS employs more than 1.6 million people in the UK and, with more than 350 career options, is a critical source of economic opportunity for local people. Figure 2 shows the percentage of jobs the health sector contributes locally by level of STP. The figure demonstrates how the NHS, which accounts for most of these jobs, is a major driver of employment in each regional economy, though some areas (the North and parts of London) are more reliant on the NHS for employment relative to other sectors.
There is a strong link between work and health; for work to have a positive impact on health, it must be ‘good work’ – providing stable employment, paying a living wage, and offering fair working conditions, work-life balance and career progression. By helping more residents – particularly those furthest from the labour market – into quality work, the health system can improve the welfare of its local communities and begin to narrow inequalities. Building a workforce that is more representative of the local area can also better respond to patients’ needs. Furthermore, employing local people can contribute to reducing the carbon impact of the health sector by reducing the number of staff reliant on transportation to get to work.
Anchor workforce strategies involve thinking not only about how the NHS can grow local workforce supply and widen access to employment for local communities, but also how it can be a better employer and place to build a career for more people. It acts as an anchor not only in the number of jobs it creates, but in how it can support the health and wellbeing of its staff through good employment conditions and the working environment – a timely undertaking, given the enormous workforce pressures confronting the NHS.
Figure 2: Health employment as a percentage of total employment by STP level
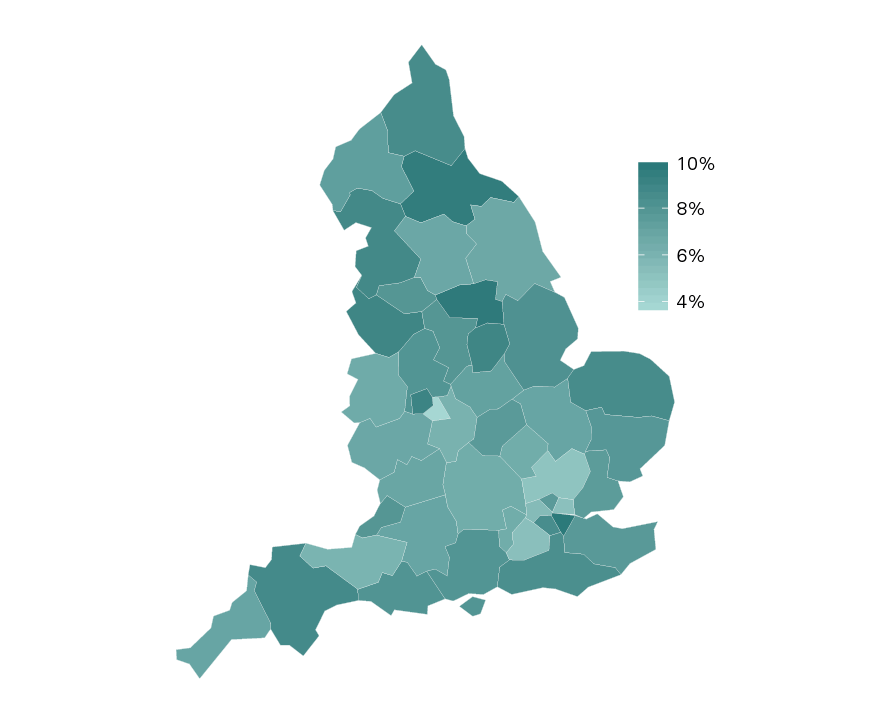
Office for National Statistics, Business Register and Employment Survey (2017)
Notes: data are for all people employed in hospital activities, medical and dental practice activities and other human health activities (eg, medical nursing homes, rehabilitation centres, psychiatric hospitals, etc.). Data will include people working in the private sector as well as part-time.
What do anchor workforce strategies look like in practice?
Widening workforce participation
- Targeting positions for local people
- Understanding local demographics and opportunities
- Creating pre-employment programmes, work placements and volunteer work experience
Building the future workforce
- Engaging young people and supporting career development
- Increasing the number and types of apprenticeships
Being a good employer
- Supporting health and wellbeing of staff
- Supporting fair pay and conditions of employment
- Supporting professional development and career progression
Policy context
Workforce shortages are the biggest threat facing the health and care system, with significant implications for the quality of care. Hospitals and mental health and community providers in England alone are reporting vacancies of more than 100,000 full-time equivalent (FTE) staff. Based on current trends, the NHS will continue to fall substantially short of the workforce it needs unless there are significant actions to increase staff supply.
There are multiple strategies that the NHS, as an anchor institution, can adopt to address workforce shortages, including better attention to career progression and training for NHS employees, with numerous efforts targeting support roles, including health care assistants. This includes the Health Education England Talent for Care Strategic Framework, which aims to create more opportunities for people to start and build a career in the NHS. Alongside this, the Widening Workforce Participation Strategy established a programme to expand access to education, employment and development opportunities for under represented communities. The Interim NHS People Plan also explicitly recognises the NHS’s responsibility, as an anchor, to support employment opportunities for local communities by creating new job pathways and making the NHS a more inclusive work environment and better employer for more people. The government’s Industrial Strategy also creates further scope for the NHS to work with local partners to improve local skills development.
Apprenticeships are another mechanism for widening access to employment. A new apprenticeship levy came into effect in 2017, and as the largest employer in the UK, the NHS has led the public sector in its use. In health and social care, around 420,000 people have started apprenticeships since 2011. The levy covers the costs of training, but not the apprentices’ wages. Smaller employers, like GP practices, can also access the levy to pay 90% of their apprenticeship training costs. There are plans to create 100,000 more apprenticeships in England by 2020, including nursing and health care assistants, and in IT, estates and facilities, domestic and housekeeping services, and business administration.,
Workforce shortages are compounded by poor experiences for some groups of staff. The 2018 NHS Workforce Race Equality Standard survey found that 15% of black and minority ethnic (BME) staff reported experiencing discrimination in the past 12 months, and that 28% did not believe that their organisation provided equal opportunities for career progression (this compares to 7% and 13% of white staff, respectively). These inequalities need urgent attention. The Interim NHS People Plan promises to deliver a more compassionate and inclusive culture that promotes equality of opportunity for all staff.
Learning from practice
Widening workforce participation
- Targeting positions for local people
NHS organisations have worked with community partners to target certain positions for local residents, who might otherwise face barriers to work. Partners include local councils and other community organisations that often have deeper reach and insight into local populations, which helps identify potential candidates and promote work opportunities.
For example, Barts Health NHS Trust has a proportion of roles available to locally unemployed applicants. In the same way that some roles are ring-fenced for internal hires, the trust prioritises local hires for a certain number of entry-level positions and works with local authorities to identify and match potential candidates (see case study on page 19).
To monitor progress, some organisations are using targets to increase the percentage of local hires – a practice adopted by some hospitals in the United States. In 2015, Johns Hopkins Health System and Johns Hopkins University launched HopkinsLocal, which stipulated that 40% of new hires for entry-level positions should come from Baltimore neighbourhoods with high poverty and unemployment. Hopkins met this target within the first year and by 2018, 47% of targeted positions (381 new hires) were filled by residents from these areas. The hospital worked with local organisations to identify unemployed and underemployed individuals for specific jobs, and provided tailored training, skills development and assistance with the application process. Residents who apply through the programme are guaranteed a first look by recruiting managers.
These recruitment methods need to reach as wide a pool of applicants as possible. This means writing job descriptions accessibly, advertising NHS roles in a broad range of outlets and using selection techniques that support inclusivity and diversity. NHS Employers and Health Education England (HEE) have created a range of tools, resources and guidance to support NHS organisations to engage local communities throughout the recruitment process, offering a helpful starting point when developing or expanding anchor strategies.
- Understanding local demographics and opportunities
Where possible, NHS organisations should aim to employ a staff mix that is drawn from, and broadly representative of, the local population it serves. This requires baseline data to know where employees come from to ensure that areas with the highest levels of deprivation are represented in the workforce, and that people from these areas have equal opportunity to advance their careers.
The Leeds Teaching Hospitals NHS Trust has been thinking critically about how to build career opportunities for local people from deprived or excluded communities, and is working with Leeds City Council through a new programme called Priority Neighbourhoods. This initiative uses local data to develop ‘neighbourhood profiles’ to help target local investments and create more opportunities in areas that fall within the 1% of the most deprived areas nationally.
‘Some little things have been easy to do. For example, some of the most disadvantaged neighbourhoods in Leeds are on our doorstep, like Lincoln Green, which has a high percentage of people who’ve recently emigrated to the UK. Feedback from those working in the priority neighbourhood highlighted that many people felt helpless as to how to get on a career pathway. In-work poverty was and is a key challenge. Working with the council we have run a series of recruitment events locally to promote routes into careers, alongside an employability programme and language courses. This has seen us make around 30 hires from within the neighbourhood and surrounding area. We’re currently planning our next cohort.’
Director of Policy and Partnerships
Leeds Teaching Hospitals NHS Trust
- Creating pre-employment programmes, work placements and volunteer work experience
A growing number of NHS organisations (supported by strategies such as Widening Participation and Talent for Care) are developing employability programmes that provide training and support to help local people acquire the skills needed to work in health and care, often linked to direct work experience, training or volunteer roles.,
One example is the University Hospitals Birmingham NHS Foundation Trust, which has worked with local partners like The Prince’s Trust to establish a Learning Hub (set up in 2008). This is a purpose-built centre fully staffed to offer pre-employment advice, training, guidance and direct links to jobs in the NHS to unemployed local people and those furthest from the labour market. In a 12-week programme, participants complete 3-week volunteer work placements in roles across the NHS and receive mentoring from trust employees. To ensure that the recruitment opportunities are widely accessible, the organisation has agreed to accept references from social workers instead of traditional employment references, for refugee populations. The Learning Hub has so far supported nearly 2,500 local people into employment within the trust and partner organisations since it opened.
East Lancashire Hospitals NHS Trust has launched a programme that offers more residents a chance to gain a qualification and volunteer work experience within the trust. Partnering with the Department for Work and Pensions and Blackburn College, the trust provides pre-employment training for the long-term unemployed, homeless people, people with learning disabilities and people struggling with drugs and alcohol. Participants complete a 3-week course at Blackburn College on employability skills in adult and child care, then do a 2-week volunteer work placement within the trust in roles including catering, laundry services or business administration. Twenty-five people completed the training as part of the first cohort in 2018, four of whom have secured permanent employment within the trust.
Survey data from HEE show that in 2015/16, there were nearly 800 employability programmes of this nature across the NHS, with 1,219 participants, many of which targeted local people or underrepresented populations. The roles targeted have tended to be lower-banded operational and administrative roles that are critical to the running of the NHS. However, there may be further scope to expand opportunities and connect more local people to clinical roles in nursing and allied health professions that have clear progression routes and where more staff are needed.
It will be important to evaluate these programmes robustly. At the sites where we conducted interviews, there has been limited attention to measuring effectiveness of pre-employment support and other efforts to widen workforce participation. Indeed, a HEE survey found that fewer than half (48%) of NHS organisations with an employability programme had evaluated it. Yet the limited evidence available suggests these programmes can work: an evaluation commissioned by HEE of programmes offered in three trusts (Manchester University NHS Foundation Trust, South Tees Hospitals NHS Foundation Trust and North Bristol NHS Trust) found that of 732 people participating in a programme at one of the sites, 52% went on to work at the trust as an apprentice or in a permanent job.,
So far, pre-employment programmes have been created in large hospital trusts with limited offers in general practice or commissioning. This suggests that more support is needed to encourage other NHS organisations to follow suit. This could be an important part of STP/ICS planning – to develop a wider health employment programme that links local people to opportunities across the sector. The introduction of PCNs may also create more scope to pool resources and develop pre-employment programmes or work placements for general practice across a locality.
There are examples of health and care organisations working together to develop opportunities across a local system. As part of the North West London Health and Care Partnership, the NHS is working with local councils and unions to develop a formal skills partnership to help more local people from disadvantaged backgrounds access good-quality work. Since forming the partnership, the NHS in west and north west London has become the largest provider of supported employment opportunities for young people with special education and development needs. By working more closely with the council, NHS organisations have made new relationships with other large employers locally (such as Heathrow Airport) and are developing further joint programmes to benefit local people. The Interim NHS People Plan promises a shift to devolving more responsibility to STPs/ICSs for workforce planning, creating further opportunities to develop collaborative approaches for improving the economic prospects of more people.
Building the future workforce
1. Engaging young people and supporting career development
Helping young people to gain the skills and qualifications they need to pursue careers of their choice is key to supporting a healthy transition into adulthood. In the UK, over 10% of young people aged 16–24 are not in education, employment or training (NEET), which can have serious long-term effects on their economic prospects and employability. As an anchor in local communities, the NHS can work with local partners to help break down barriers to future employment for young people.
A growing number of NHS organisations are collaborating with local schools and community organisations to expose more young people to careers in the NHS, raise the profile of different types of NHS jobs and help support skills development locally. This has also been a part of HEE’s Widening Participation strategy, which has introduced a framework to support the NHS to partner with schools to create new training opportunities and mentoring for students.
Through our research, we have identified several examples of trusts implementing initiatives to support young people to understand potential NHS career options and to gain the experience and skills needed to work within the sector and broader local economy. Many of these examples focus on young people from disadvantaged communities.
For example, Birmingham has one of the highest rates of youth unemployment in the country, and the local trust has developed programmes that target young people at risk of homelessness and unemployment. In addition to its programmes with The Prince’s Trust through its Learning Hub (see page 15), the University Hospitals Birmingham NHS Foundation Trust is also working with Birmingham City Council to deliver Youth Promise Plus – a city-wide initiative providing training, support and work opportunities to at least 16,000 young people (aged 15–29) classed as NEET. Together with Birmingham and Solihull NHS trusts, the local hospitals have committed to supporting 850 participants through this programme.
The Leeds Teaching Hospitals NHS Trust is also promoting careers to young people in the local area. It has appointed a cohort of staff to act as health career ambassadors to promote NHS opportunities in local schools. It has also established a work experience programme that enables young people to directly observe the trust’s work in both clinical and non-clinical areas. After finding that the initial uptake of work experience placements came from younger people in more affluent areas, the trust has started to target schools in more deprived postcodes to redress the balance.
2. Increasing the number and types of apprenticeships
NHS apprenticeships can offer paid employment, protected learning time and clear career progression from support worker through to a degree or postgraduate-level qualification. They can be used to support new trainees as well as internal staff looking to advance in their careers.
Some NHS organisations have used the funds they contribute to the apprenticeship levy to scale their approach. The Leeds Teaching Hospitals NHS Trust is one of a few organisations piloting a nurse apprenticeship programme, to give more people from different backgrounds an opportunity to access NHS careers. The pathway involves a 6-week traineeship with a guaranteed interview on completion for a Level 1 apprentice clinical support role. Building on the initial success, the trust has expanded the programme to include roles in administration, facilities, medical engineering and other clinical support areas. In 2018, apprentices accounted for 3% of the trust’s workforce; since 2015, it has increased its apprenticeships by 51% each year.
Stakeholders we interviewed welcomed the concept of a compulsory employer funded and led training programme like the apprenticeship levy, but felt that some changes are needed for it to provide greater local benefit. For example, it would be better in some cases if unused funds could be retained within the sector or within localities, rather than redistributed elsewhere. There is also a lack of data on where people move on to after completing their apprenticeship, which hampers understanding of how the programme supports career prospects, and for whom.
Some felt that the levy should have explicit aims to boost social mobility, so that the funds could support economic prospects for people from disadvantaged backgrounds or who have not benefited from apprenticeships so far. This could mean prioritising a certain number of placements for local people living in more deprived areas and who are underrepresented in the NHS clinical workforce. The Interim NHS People Plan committed to explore how the apprenticeship levy could evolve to support more inclusive pathways into NHS careers, which may provide an impetus to implement some of these changes. In either case, given the challenges NHS organisations already face in using the levy, any changes must be balanced and not overly burdensome to administer.
Case study 1: Barts Health NHS Trust
Based in east London, Barts Health NHS Trust is the largest NHS trust in England, with an annual total workforce spend of £869m and around 16,500 staff. It has high vacancy and staff turnover rates, exceeding 10% and 13% respectively. The trust’s response to this provides a good example of how an NHS organisation can combine a range of programmes and initiatives in one of the key anchor areas to focus on improving local health, wellbeing and social mobility, while also addressing workforce pressures.
Targeting positions to help local unemployed people
To employ more local people, particularly from disadvantaged backgrounds, the trust ring-fences a proportion of entry-level roles for local applicants. These vacancies are shared with local authorities who help identify and match potential candidates based on their skills, interests and other requirements. The most common positions targeted are clinical and corporate roles that do not require advanced degrees, ensuring that they are accessible to residents who may not have high educational attainment.
The public health team advocating for this change needed buy-in from recruitment managers, who worried that prioritising local applicants would limit choice of candidates. The team argued that even if fewer applicants were shortlisted for each role, this process was more efficient as candidates were pre-screened and pre-matched by the local authority according to their skills and interests.
Supporting career opportunities for younger people in the area
The trust has also been working with schools and community partners on programmes designed to generate qualified and prepared local applicants from socially disadvantaged communities.
Project Search East London, run in partnership with local schools and employment services, aims to increase career opportunities within the trust for young people with learning difficulties and/or disabilities. Adapted from an initiative at Cincinnati Children’s Hospital in the United States, it provides employability skills training and job placements for young people at Barts. In the five years since it launched, 54% of participants (46 interns) have moved into paid employment in roles including ward clerk and ward host, and in catering and portering. The project has a designated job coach who works with managers to provide inductions, define work placement duties and support interns with any specific learning or workplace issues. Project Search is also being adapted by some other NHS organisations across the UK.
Barts Health NHS Trust has also recently launched a Health Horizons programme, a multi-pronged strategy to help more young people locally build their careers in the NHS. Run by the trust in partnership with Barts Charity and supported by the JP Morgan Chase Foundation, the programme works with schools across local boroughs to increase awareness of NHS careers and promote the NHS as a local employer. The trust has appointed sector career champions and mentors working with secondary schools and local councils to offer career advice, run career awareness events and recruit for volunteer work experience placements.
For students aged 16–18, the programme works with Jobcentre Plus and local authorities to identify career opportunities in target boroughs and deliver coaching and interview training. The programme is building local supply in roles where recruitment has been especially challenging, including allied health professions, nursing and nursing associates, health care assistants and health care navigators. As of summer 2019, it is yet to be fully implemented, but aims to recruit 400 students to work experience placements or apprenticeships and support 100 participants through pre-recruitment programmes (with a target of 50% ultimately going on to employment in health or social care).
Being a good employer
- Supporting health and wellbeing of staff
The NHS has an opportunity to improve the health and wellbeing of local people in the way it treats and supports its own large body of staff. Supporting a happy and healthy NHS workforce can also have a knock-on impact on the health and wellbeing of the wider community, given the number of connections NHS staff have through their families and social networks. The latest NHS staff survey results reveal that the NHS could do much more to promote a healthier working environment. While there have been improvements in some areas, less than a third of staff reported that their trust takes positive action on health and wellbeing.
Many NHS employers have prioritised improving staff health and wellbeing, offering workplace wellness schemes to reduce stress and promote healthy lifestyles. Though important, these strategies need to be carefully designed to be accessible to all and to not inadvertently widen inequalities within the workforce. Studies have shown that employees who participate in workplace wellness programmes often have higher incomes and are in better health than those who do not.
This was a case in point at the Royal Free London NHS Foundation Trust, where an internal review of its workplace programmes revealed that, of the 1,700 participants, only 10% were from bands 1 and 2 – despite these staff having some of the highest rates of referrals to occupational health and missing the most work days due to musculoskeletal issues. These staff also reported feeling extremely stressed at work and often ignored or unvalued. The trust therefore co-designed a workplace wellness programme with staff in the facilities team (including porters, domestic and security staff), which led to a range of activities including cooking classes, family and social events, a financial advice workshop and group walks. An independent (unpublished) evaluation indicates that the programme brought benefits, including more staff reporting that they felt valued, physically active and less stressed at work. The evaluation also suggests a reduction in sickness absences of 1.6 days for porters and domestic care staff compared to a control arm of other band 2 staff during the 12 months of the project. The trust now needs to find a way to sustain the programme beyond its initial national grant funding.
- Supporting fair pay and conditions of employment
An important determinant of staff wellbeing is the terms and conditions of their employment, including receiving a fair wage and having a good work–life balance. Low pay can lead to financial hardship, trapping people in in-work poverty, with important implications for health and wellbeing. Being an anchor means ensuring that the NHS provides secure employment and fair compensation so that all its staff can live with financial security, not least because in some areas the NHS is the largest employer.
The Health Foundation’s Closing the Gap report with The King’s Fund and Nuffield Trust shed light on the current challenges in staff pay and how they impact on different employee groups. The 2018 pay deal marked an important change in how NHS staff are paid, lifting the 1% cap and resulting in almost all staff receiving real-term pay increases. Staff in lower bands received the biggest increases, and from 2019/20, every worker employed directly through the NHS is now paid at least the real living wage.
Lifting the pay cap is a crucial step for many NHS staff experiencing hardship. For example, the Royal College of Nursing (RCN) reported that the number of nurses and health care assistants receiving a grant from the RCN Foundation to alleviate severe financial hardship had doubled between 2010 and 2016. And a Unison survey of 12,000 NHS employees in lower-paid roles showed that 21% had to take on another paid job to make ends meet. As the Closing the Gap report makes clear, it is critical that pay for NHS staff keeps up with the cost of living beyond 2021/22 (when the pay deal expires) if the NHS is to support the financial security of all who work for it.
The NHS also needs to remunerate staff fairly, addressing the persistent ethnic and gender pay gaps, if NHS organisations are going to maximise their potential as anchor institutions and provide a model for other employers. The NHS also has an opportunity to go further and influence the wellbeing of many more workers by extending living wage and fair working condition standards to all its contracted employees.
- Supporting professional development and career progression
Supporting staff to meet their full potential and advance in their roles is a key feature of any good human resources (HR) policy, but is particularly important for anchor institutions. Given the size, scale and varied nature of its workforce, the NHS has a key opportunity to ensure that no one gets trapped at the low end of the labour market. It can do much to help staff progress into higher-wage positions – for example, by mapping out clear potential career pathways for all roles and offering continuing professional development and training for staff at all levels, not just those in the highest-paid bands.
While the NHS has focused at both the national and local level to improve staff development, there is significant scope to ensure that these opportunities are accessed equally across staff groups. For example, people from BME backgrounds are underrepresented in leadership positions, with the 2018 NHS Workforce Race Equality Standard report revealing that over half of trusts (52%) have no BME representation in the 'very senior manager' pay band. The percentage of chairs and non-executives of NHS trusts from a BME background has nearly halved, from a peak of 15% in 2010 to 8% today. As with pay, it is important that the NHS seeks to understand what is driving inequality and develop strategies to redress this.
Equality of opportunity is also important in the context of broader technological advances that will change the nature of health care work. The Topol Review noted that clinical staff will need new training and development to acquire the skills that digital transformation requires. These changes offer an opportunity to improve the quality and efficiency of health care, but the workforce implications must be closely considered. For example, where new technology brings automation of care or tasks, the risks to lower-banded support roles (an important entry point to NHS careers for many people) should be monitored. As an anchor institution supporting inclusive employment, the NHS must use technology to upskill and advance all roles, not just those in the highest-paid positions. The Care City case study below provides an example of an inclusive professional development strategy that has used digital enhancement to improve the career prospects for more junior members of staff.
Case study 2: Care City
First established by North East London Foundation Trust and the London Borough of Barking and Dagenham, Care City is a centre for healthy ageing and social regeneration that works across northeast London. The area has 10% unemployment and the lowest life expectancy in London. Care City brings investment and opportunity to help regenerate the boroughs. One way it does this is by testing new ways of using digital technology to improve the skills of people working in support roles, such as health care assistants. Funded through the Test Beds programme run by NHS England and the Office for Life Sciences, the programme involves three components:
- Building the skills and confidence of domiciliary carers to use new technology that helps spot deterioration among patients with long-term conditions early, and supports better medication management.
- Training health care assistants working in primary care to support patients who have been prescribed a digital application by a GP to make use of the technology and help prevent deterioration of long-term conditions.
- Teaching skills to administrators in acute care to provide support for people with heart failure and administer digital programmes that support education and exercise between appointments.
Care City leadership saw an opportunity with this programme to develop people in support roles – who often have the least access to technology – to improve the way they deliver care. An evaluation is underway; the team hopes that the digital training will not only improve care delivery and the patient experience but also support future career prospects and professional advancement for more junior members of the health and social care workforce.
Summary and implications for practice and policy
Growing a local workforce and making the NHS a better place to build a career are areas where the NHS has the largest scope to maximise its role as an anchor. These goals also align with the policies and programmes the NHS is pursuing to address recruitment and retention challenges.
At the national level, delivering the NHS Interim People Plan can support NHS organisations to widen workforce participation and create more diverse and accessible pathways into NHS careers. This includes ensuring adequate funding and resources for training and development so that all staff can progress in their roles, and that opportunities are inclusive and help break down the barriers to advancement that exist for many staff groups. Where policy levers (such as the apprenticeship levy) already exist, they should be reviewed and, if necessary, reformed to ensure that they create opportunities for communities who could benefit the most.
At the local system level, STPs and ICSs should enable NHS organisations to advance anchor strategies as part of local workforce plans, and develop joint approaches with local partners that improve employment prospects for local people. The NHS’s regional teams can also help share learning and evidence between systems.
There is also scope for individual organisations to do more to widen participation, increase the numbers of local people they employ and ensure good work for current and prospective employees. NHS providers could make inclusion, diversity and local hiring explicit organisational goals, and work with partners to deliver more volunteering, work experience, apprenticeships, skills training and coaching to build a pipeline of future employees and prepare more people for work in the NHS. This requires both local demographic data and baseline data about existing staff to identify the greatest areas of need and to target interventions. Once staff are in post, every opportunity should be taken to support staff health and wellbeing and create equal opportunities for career development and progression.
If approached correctly, anchor strategies can respond to workforce pressures at the same time as improving health and addressing inequalities within local communities. These strategies need to be accompanied by clear targets and metrics to help assess progress and the wider impact of these strategies over time.
|
Practical resources to support implementation |
|
Economic and Social Impacts and Benefits of Health Systems (World Health Organization Regional Office for Europe) NHS Workforce Health and Wellbeing Framework (NHS Employers) Recruiting from your community (NHS Employers) The Talent for Care. A National Strategic Framework to Develop the Healthcare Support Workforce (Health Education England) Think Future – tools, resources and learning (NHS Employers) What Comes Next? National Strategic Framework for Engagement with Schools and Communities to Build a Diverse Healthcare Workforce (Health Education England) Widening Participation. It Matters! Our Strategy and Initial Action Plan (Health Education England) |
† Volunteering takes many forms and can give a range of benefits to the recipient, the organisation and the individual who is giving time. For the purposes of this report, we focus specifically on the benefits of volunteer opportunities in terms of providing work experience opportunities and supporting skills development and routes into employment for different populations.
‡ ‘In-work poverty’ refers to individuals living in households where income is below the poverty threshold despite one member of the household working either full-time or part-time. The poverty threshold is defined as under 60% of the average household income (before housing costs).
Chapter 4: The NHS as a purchaser and commissioner for social value
Why this matters
The NHS has significant purchasing power, spending £27bn each year on goods and services in England alone. Decisions about what the NHS decides to buy, and how, have ramifications on local population health and wellbeing. Procuring and commissioning more goods and services from local small and medium-sized enterprises (SMEs) and voluntary and community sector organisations can have an important economic impact, as resources spent locally have a multiplier effect and are reinvested in the local community at a faster rate than resources spent with national corporations., There is limited conclusive evidence on the size of local multipliers and the extent to which local procurement stimulates local economic growth. This will depend in large part on the nature of local economies, but some studies have shown an effect ranging between 1.7 and 2.1 (for example, investing £1 in a local economy generates between £1.70 and £2.10 worth of growth).,,,
An analysis of procurement data of 10 anchor organisations in Leeds (four local authorities, two colleges, a university, a hospital, a CCG and a housing association) found that they collectively spend £1.4bn a year on goods and services, nearly half of which (£665m) left the local economy. The analysis concluded that by shifting 5%–10% of their spend locally, these anchors could generate between £168m and £196m a year of additional economic activity in the local economy when multipliers are factored in. By spending more resources within the community, anchor organisations may help local businesses to grow, employ more people and pay higher wages, thereby stimulating local economic development.
The NHS could also derive greater social benefit from the money it spends by introducing principles of social value into its contracts and procurement processes. There is no standard definition of ‘social value’, but it broadly refers to the wider societal benefits that can be gained from purchasing decisions (over and above those to the contracting organisation) – for example, by specifying that jobs are created locally with living wages and fair working conditions. By choosing to work with suppliers that advance social, environmental and economic outcomes in their local populations, the NHS can secure even greater value from its investments and support broader community health and wellbeing. By changing its procurement and commissioning processes, the NHS can also lead by example and influence other organisations in its supply chain, thereby having a wider community impact.
What do anchor procurement strategies look like in practice?
Shifting more spend locally
- Building local capacity and supporting local supply chains
Embedding social value into purchasing decisions
- Prioritising and monitoring social value
- Building organisational capability and capacity for social value
Policy context
Applying anchor strategies to NHS procurement is not without challenge, as this is an area where NHS organisations have less local flexibility, particularly in England. This is especially true following the introduction of the Future Operating Model (FOM), which aims to improve efficiency and effectiveness of NHS purchasing by introducing greater standardisation and price transparency.
It is expected that once the FOM is fully implemented, 80% of the NHS’s spend in England on everyday hospital goods, consumables and capital equipment will be purchased through centralised procedures. The FOM was developed in response to recommendations in Lord Carter’s review into operational productivity in English hospitals, which determined that the NHS could do more to leverage its collective buying power to reduce unwarranted variation in prices and procurement approaches and help release savings. The FOM covers 11 ‘category towers’ or areas of spend, including medical consumables, capital equipment and common goods, but there are still areas where the NHS has more flexibility to procure locally, including catering and hotel services.
Even with these changes, procurement and commissioning can still be used to improve health outcomes for local communities. In England and Wales, the 2012 Social Value Act requires public sector commissioners to consider how the services they buy support wider social, environmental and economic wellbeing when they procure services above OJEU (Official Journal of the European Union) thresholds., Scotland has a similar policy, where the government requires contracting authorities to consider how procurement can help reduce inequalities and shift more spend towards SMEs in contracts of £4m or above. In Wales, the government also requires public sector organisations to apply a community benefits policy to all procurement, regardless of the value of the contract (though outcomes need only be reported on contracts worth over £2m). The UK government also committed to spending £1 in every £3 with SMEs by 2020, and there are separate requirements in England that food and catering services procured by central government or the NHS must meet specified social and environmental aims.
The legislation should, in theory, promote anchor practices, but there are significant differences in how NHS organisations have applied its principles. In England, a 2017 analysis of CCG Freedom of Information Act requests revealed that only 13% of clinical commissioners actively considered social value as part of decision making, and 43% had no policy in place.
Although this variation suggests room for improvement, some NHS organisations are already using social value and purchasing decisions to benefit the local community.
Learning from practice
Shifting more spend locally
- Building local capacity and supporting local supply chains
An important first step in shifting more spend locally is to understand current purchasing practices. NHS organisations can conduct internal audits of procurement spend to identify the percentage of purchasing that stays within the local region, and then work out how to reallocate more of the purchasing budget towards local organisations. The Centre for Local Economic Strategies (CLES) benchmarked spend at two NHS provider trusts by examining procurement data on goods and services from their top 300 suppliers for 2017/18 (see Table 2).
Table 2: Procurement spend of East Lancashire Hospitals NHS Trust and Leeds Teaching Hospitals NHS Trust, 2017/18
|
Procurement spend |
Percentage spend in local authority |
Percentage spend in wider region |
||
|
Leeds Teaching Hospitals NHS Trust |
£482m |
28% (Leeds City) |
31% (West Yorkshire including Leeds) |
69% |
|
East Lancashire Hospitals NHS Trust |
£117m |
19% (Burnley and Blackburn-with-Darwin) |
23% (Lancashire) |
77% |
This shows that significant spend at each trust is ‘leaking’ out of the local economy, and there is potential to work with local suppliers and get more value from procurement. How local economic boundaries are defined will vary by area, but benchmark analysis can help organisations set reasonable targets for retaining more spend within communities.
Once an organisation understands its purchasing practices, it needs to find ways to prioritise local suppliers. Stakeholders reported pushback from staff who fear that requiring suppliers to be local is anti-competitive and violates existing regulations. While regulatory frameworks do prevent NHS organisations from requiring suppliers to be only local or use only local labour, procurement experts we spoke to said that it can be specified that potential suppliers must help advance local community development. More can be done to provide training and clarity to purchasing teams on what is legally possible and how to enforce social value.
Some efforts by anchors to procure more goods and services locally have been criticised as protectionist or inefficient., It is important to fully evaluate and understand the impact of these strategies; anchor strategies should aim to boost the competitiveness of local suppliers, not shield them from competition. Any effort to shift more spend locally must be in line with existing regulations that require services to be competitively procured. Audit functions can be bolstered to help ensure these potential risks are mitigated and that local suppliers compete credibly on costs and quality.
Shifting more spend locally will also depend on the capacity and capability of the local supplier market, and may not be possible in all areas of spend. Anchor organisations have a role in supporting local supply chains and ensuring that local businesses, social enterprises and SMEs can compete for and secure NHS contracts. Existing tools and guidance make clear that building local capacity starts in the pre-procurement phase, identifying which resources and services can be secured by organisations working in and with people from the community., This may involve conducting audits and outreach with the local economy to identify opportunities and build new relationships, particularly with SMEs and voluntary sector organisations. Local NHS charities are often well placed to know voluntary sector organisations or SMEs in the area with whom to engage.
Interviewees noted how this engagement can help build awareness and encourage smaller organisations to bid for and win contracts. Engagement also helped contracting organisations understand the barriers that local organisations face in working with the NHS. Experts we spoke to thought that STP and ICS leadership could be helpful in coordinating this engagement across a larger area, but that individual organisations still need to conduct their own engagement and outreach, particularly in the lead-up to large projects and contracts being advertised. Procurement leads described how it can be difficult to reach smaller organisations that may not always have the capacity or staff to engage in outreach. This is why NHS organisations should also consider taking other measures alongside engagement, like ensuring prompt payment terms or unbundling contracts into smaller parts so that SMEs are more able to compete, and are not required to deliver all aspects of a service to be successful. Interviewees warned, however, that enacting these strategies can be administratively time-consuming, and not all NHS teams have capacity and expertise to do this.
Some anchor organisations have also developed toolkits and guidance for suppliers to help organisations understand the required criteria and improve the quality of applications. For example, the Greater Manchester Combined Authority developed a toolkit for suppliers that lists clear examples of what provider organisations can offer as part of their bids against core social value criteria, alongside a list of resources to help organisations implement these practices. And in Wales, the Co-operative Centre (a community development agency that supports social enterprises and co-operatives) has developed modules and guidance for suppliers demonstrating ways they can contribute to broader social value, as well as tools and techniques for reporting against criteria.
More can be done at the national and regional level to help NHS organisations spend more locally. For example, in England, stakeholders noted how the FOM towers (see page 25) could incorporate at least one regional provider (where possible) in categories to give NHS organisations an opportunity to retain resources within the health economy where appropriate.
Case study 3: North Bristol local food procurement
North Bristol NHS Trust changed its approach to procurement of catering services to purchase more food locally. In 2018, 54% of its food spend went towards local produce. It has been awarded Food for Life certification by the Soil Association, recognising excellence in catering that provides environmentally sustainable and ethical food.
To make this change, the catering team conducted a large audit to identify what produce was available locally and the financial implications of switching suppliers. They removed certain menu options (lamb) that could not be sourced within a 50-mile radius. This increased costs slightly: for example, beef cost 1p more per meal when sourcing from a local and organic provider. The director of facilities, who was supportive of the change from the start, looked for savings from elsewhere to offset the increase. Existing regulations helped gain senior backing for the approach, as trusts are already required by the Department of Health and Social Care to have a food and drink strategy that supports procuring more food from local, sustainable sources.
Embedding social value into purchasing decisions
- Prioritising and monitoring social value
There are promising examples of NHS organisations that have embedded social value into procurement processes, either by introducing explicit weightings or designing core contract specifications so that suppliers must meet specific conditions – for example, creating local jobs and training opportunities, paying a living wage and adopting environmentally sustainable practices.
To aid this process, some NHS organisations have established frameworks and action plans with specified outcomes and definitions for social value to assess bids and help measure performance against social objectives. Doing so often requires sophisticated cross-department working to write contract specifications and agree common aims and procedures. Stakeholders we interviewed noted that senior leaders play an important role in developing a clear vision and strategy for social value to underpin these efforts and ensure they are consistently applied.
STPs/ICSs also have an important role in strengthening the application of social value across a health economy. At present, very few STP plans (13%) refer explicitly to social value, though some do include related objectives around narrowing inequalities, improving access to housing and reducing poverty. STP and ICS leads could work with partners across a place to agree shared objectives and define common metrics for social value, which in turn could help reduce local variation in how the concept of social value is adopted in a local health economy and could help mainstream it in practice.
Even where frameworks exist, the NHS could take a broader approach to have an even greater impact on community health and wellbeing. For example, when NHS organisations consider social value it tends to be primarily as part of competitive tender processes, which are limited to large contracts. Applying these principles more systematically across areas where the NHS has greater flexibility (such as hotel and catering services), even though they may be of lower value, can help maximise spend for community benefit. Stakeholders noted that the overall weighting NHS organisations give to social value when scoring contracts tends to be low (between 5% and 10%), with most value placed on cost and quality. This is lower than local government, where social value weightings can be as high as 30%.
Applying more weighting to social value increases the likelihood of selecting suppliers who provide greater community benefit, but even so, there are trade-offs. For example, requiring that all suppliers pay their staff a living wage can make a service more expensive to deliver:
‘Often we have no flexibility to increase the cost of running a service, so requiring suppliers to pay a living wage means we can’t deliver the whole service to the same level. This is made harder by the fact that we face pressure to achieve cost savings on contracts year on year… This is why we’ve started with a weighting of 10%, with the goal of increasing it slowly over time. This felt more manageable to our purchasing team.’
Head of partnership
Clinical commissioning group
There are still limited accountability mechanisms for enforcing the use of social value, which interviewees believed may contribute to inconsistencies in how it is applied. To be compliant with the Social Value Act, public sector commissioners are only required ‘to consider’ social value in purchasing decisions, yet they are rarely scrutinised to show what ‘consideration’ means. Even with the incorporation of social value into the NHS Standard Contract in England, CCGs and trusts reported not being required to provide evidence for how they meet the requirements.
Strengthening the legislation so that public bodies are required to formally incorporate social value into purchasing decisions could help mainstream it in practice. In 2018, the government announced plans to do just that – making social value an explicit requirement of central government contracts. Legislative proposals intended to ease the implementation of the NHS Long Term Plan also aim to introduce a ‘best value test’. Although more detail is needed on how the test will operate, this has the potential to support system leaders to incorporate wider considerations of public and social value when commissioning services. But legislative changes notwithstanding, there is more that can be done to build greater accountability for social value across the sector. Interviewees said that NHS England and NHS Improvement could help introduce stronger incentives for social value, either by encouraging use of weightings or helping to define minimum key performance indicators (KPIs) through existing levers, including CCG assurance frameworks and STP/ICS guidance. They could also set minimum social value standards for the NHS nationally, establish common metrics and showcase promising practices that can be adapted locally. The Scottish government, for instance, has issued guidance for contracting authorities on how to define community benefit requirements as part of procurement, with suggestions for how public sector organisations can develop metrics to monitor performance against national and local outcomes.
However, even where national standards and resources exist to support more progressive procurement, they have not always become embedded in practice. For example, the Government Buying Standards for Food and Catering Services (GBSF) requires all central government departments and the NHS in England to meet basic minimum standards for sustainability and socioeconomic value, and to use a balanced score-card when evaluating bids to ensure that more complex criteria, like how companies source from SMEs, are factored into procurement. A 2017 government review found that while significant progress had been made to adopt GBSF standards, almost half of NHS trusts were not fully compliant. According to stakeholders we interviewed, the scorecard has been difficult to mandate centrally, given that these services are procured so differently across organisations and often involve sub-contractors that can be harder to monitor.
Many NHS organisations also lack the means to ensure that their suppliers follow through on social value commitments. Establishing monitoring frameworks so that NHS organisations can systematically collect evidence and track progress against social value indicators could help build accountability and increase the benefit of anchor procurement strategies. However, stakeholders noted that contract management can be time-consuming, and should be proportionate to the size of the contract to avoid being overly burdensome.
Case study 4: Wales community benefits measurement tool
Wales provides an example of how to monitor and build accountability for social value at national and local levels. The government requires public sector organisations to report on the broader community benefit of contracts over £1m (though organisations are encouraged to consider social value as part of all procurement decisions, irrespective of value).
To aid this, the Welsh government has established a community benefits measurement tool to help organisations capture the full range of outcomes, including worksheets and guidance for purchasing managers to report on a number of defined measures. These include whether procurement budgets have: supported businesses based in Wales and SMEs; helped local unemployed people to find work; diverted waste from landfills; and created new apprenticeships and training opportunities. Organisations report to the government, which can then track the broader social value and multiplier effect of public spend.
While designed primarily as a reporting tool, this resource has also provided a consistent way for organisations to measure outcomes. It is used locally by organisations as part of their ongoing contract management process to ensure that suppliers meet agreed standards for social value.
Case study 5: Social value in Salford
Salford provides one of the more advanced examples of what a collective approach to social value and progressive procurement can look like. In 2016, organisations across the public, private, voluntary and community sectors formed the Salford Social Value Alliance, which supports all partner organisations to deliver services and contracts with social value in mind. In 2017, it launched a campaign to make a 10% improvement across 11 social and environmental outcomes by 2021. This included increasing the number of residents from vulnerable groups accessing jobs and training; supporting more people to cycle when commuting; and directing more spend towards local organisations.
The alliance includes local NHS organisations, which took part in early engagement activities to help establish shared principles for how to embed social value priorities in health and care commissioning and procurement. Salford CCG has since developed an action plan for social value, which acknowledges its role as an anchor and builds on the metrics set in the 10% campaign. It is also expected that this strategy will help underpin developments through the ICS and joint working with the local council as part of integrated commissioning arrangements.
The alliance has also created toolkits and resources to help partner organisations embed community benefit into commissioning and procurement decisions, and to measure impact. The city council has taken the lead in producing annual reports on social impact. In 2018, 59% of local government’s direct procurement spend was with Salford-based suppliers, nearly half of their wage bill goes towards residents and 18 council suppliers are accredited Living Wage Foundation employers (up threefold on the previous year).
- Building organisational capability and capacity for social value
It is essential that any effort by system leaders to embed social value comes with capability building for those in charge of procurement. Interviews revealed how purchasing managers – even those who understand the importance and concept of social value – often have limited capacity and capability to incorporate principles in their daily work:
‘The expertise of our patient meals contract manager, for example, is to make sure that our patients are satisfied with the quality of their meal, and that they get what they need to support their recovery. It’s not usually in their skill set to write contracts to drive social value and provide evidence for how they are increasing local employment and reducing gender pay gaps across employees… Even when they understand why the principles of social value are a priority, it is not something they have been trained to do.’
Sustainability lead
Acute trust
Purchasing teams must also be given the time and space to build skills and knowledge on social value and explicit permission to integrate these outcomes into contracting decisions. System and organisational leaders can help signal more clearly that social value is a priority, and take steps to ensure that local teams see it as part of their role. They also have a role in facilitating sharing of learning evidence and good practice. Numerous tools and resources exist to help support staff training on social value and progressive purchasing practices. For example, the NHS Sustainable Development Unit (SDU) has developed a range of resources, including a learning module, case studies and social value calculator, to help NHS organisations apply the Social Value Act. Social Enterprise UK has developed a Social Value Guide to help procurement managers and commissioners apply social value in practice. Some of our interviewees from CCGs also mentioned developing training packages on social value for use by procurement teams across their health economy. (Further resources to support staff capability and knowledge on social value are available in the box on page 35.)
The experience of NHS trusts also shows the value of having a designated sustainability or social value lead who can oversee local purchasing initiatives and link up efforts across departments. Interviewees said that the person in this role can also train purchasing managers across the organisation and ensure that strategies are applied systematically (also freeing up capacity among purchasing managers, who are often pressured to meet other efficiency targets).
‘It can be helpful to have someone who sees supporting social value across the organisation as their primary role and has the knowledge to think of the same problem through different lenses. Workforce teams don’t always work with procurement teams, or with estates – it can be really helpful to have someone who can link efforts and help bring these functions together as part of one strategy.’
Sustainability lead
Acute trust
Stakeholders also emphasised the value of designating a board member to lead on social value and sustainability to help join up efforts as part of a more centralised organisational approach.
Summary and implications for practice and policy
Directing more of the NHS’s spend towards community benefit is not without challenge, given that many purchasing decisions are made centrally. However, there are still areas of procurement (particularly within services) where purchasing can be a lever to stimulate local economic development and support broader socioeconomic aims. There is legislation in each country of the UK to support this, but more must be done nationally to help clarify definitions, metrics and opportunities to fully embed social value principles. This means defining minimum standards nationally and putting in place accountability for delivering social value across the system.
While implementation will look different based on local and organisational contexts, there are opportunities nationally to develop templates, standard contract language and measurement tools that can be adapted by local systems to avoid unnecessary duplication of efforts.
Underlying all these efforts will be a need to build greater organisational capability. For NHS organisations, this means giving purchasing managers the time, training and resources they need to develop new expertise and progressive procurement approaches. Local system and organisational leaders should signal promoting social value as a priority and ensure that teams are given the permission to adopt new approaches. NHS organisations should also be encouraged to learn from other local partners (such as councils) with experience in implementing progressive procurement policies. Driving change will require baseline data on current practices so that each organisation can set informed and realistic targets for directing more spend towards community benefit. It also requires organisations to understand their local markets and address barriers that local suppliers face when trying to work with the NHS. And, as with all anchor practices, progressive procurement approaches will have greater impact if included as an explicit organisational aim, with someone leading on coordination and monitoring across the organisation.
|
Practical resources to support implementation |
|
Creating Social Value – module (Sustainable Development Unit) Economic and Social Impacts and Benefits of Health Systems (World Health Organization Regional Office for Europe) Social Value Calculator (Sustainable Development Unit) Social Value Toolkit. Guidance for Suppliers (Greater Manchester Combined Authority) Social Values Forums Toolkit (Wales Co-operative Centre) The Public Services (Social Value) Act 2012. An Introductory Guide for Commissioners and Policy Makers (Department for Digital Culture, Media and Sport) The Social Value Guide. Implementing the Social Services (Public Value) Act (Social Enterprise UK) Using the Social Value Act to Reduce Health Inequalities in England Through Action on the Social Determinants of Health (Public Health England and UCL Institute of Health Equity) |
§ Procurement and commissioning are both used in reference to social value and mean slightly different things. In this paper, we use the following definitions:
• Commissioning is the process that public sector organisations go through to assess and determine what services are needed for a local area and choose what and how to allocate resources to provide services that meet those needs. Commissioning is a cyclical process involving many steps to meet strategic objectives, including identifying need, scoping the market for potential providers, drawing in expertise, establishing service specifications, deciding how to resource the service, selecting a suitable supplier, and evaluating and monitoring performance against service specifications. Commissioned services can be funded in many ways, including providing the service in-house, grant funding or procurement from external providers.
• Procurement refers to the method of purchasing goods and services by public sector organisations from other external or third-party organisations, resulting in a contract. Source: www.gmcvo.org.uk/system/files/issues%2019.pdf
¶ Local multipliers are used to estimate the knock-on effects (for example, new employment opportunities or increased incomes locally) of stimulus spending on local economic growth. A multiplier greater than 1 corresponds to a positive growth stimulus (returning more than £1 for each pound invested locally), whereas a multiplier less than 1 indicates a net loss from spending.
** To provide context to these figures, CLES has created an average of the spend of the 26 analyses it has carried out covering procurement in a range of anchor organisations (including local authorities and higher education institutions). It finds that on average, anchors spent 36% of total spend inside the local authority boundary and 63% within a wider regional area.
Chapter 5: The NHS as a land and capital asset holder
Why this matters
NHS organisations often have significant physical assets that can be leveraged for community benefit. Though data are limited on the exact size of the NHS’s entire estate portfolio, it includes 8,253 trust and primary care sites across 6,500 hectares of land in England alone.
Anchor strategies involve thinking about how the NHS can manage and develop its land and estates to support broader social, economic and environmental aims – for example, by working with partners to support more high-quality, affordable housing and widening access to community spaces. This is especially important for lower-income groups, which tend to have poorer-quality housing and less access to green and community spaces.
Housing is an important driver of health; physical and mental health is affected by quality of housing, where it is located and how connected it is with the wider community. Estimates from 2011 suggest that poor quality housing costs the NHS around £2.5bn per year. Affordable housing close to workplaces can benefit staff, while helping to improve retention and offering environmental benefits.
Communities are also more resilient when people are connected through social networks, and opening NHS buildings and land for community use or supporting the development of green spaces can provide vital opportunities for social interaction. The NHS also influences the local economy through who it lets operate and conduct business in its facilities (such as stores and food outlets). By providing more opportunities for SMEs and working with organisations that promote social good, the NHS can further support community wealth development.
What do anchor capital strategies look like in practice?
Expanding community access to NHS property
- Enabling local groups and businesses to use NHS estates
Converting and selling estate for community benefit
- Supporting access to affordable housing or housing for key workers using NHS estate
- Working in partnership across a place to maximise the wider value of NHS estates
- Developing accessible community green spaces
Policy context
In many parts of the country, NHS estates are in poor condition, lacking sufficient buildings and infrastructure to meet clinical demands. The capital budget for investments in buildings and maintenance has declined in real terms between 2010/11 and 2017/18, leading to chronic maintenance backlogs and many NHS sites needing significant upgrades. The government did recently announce a £1.8bn short-term capital funding increase for the NHS in England, but this level of investment falls well short of what is required to bring NHS infrastructure to modern standards., These immediate pressures can make it difficult for the NHS to consider the wider value of its estate for local communities.
This context has put pressure on the NHS to raise capital through sales of land and assets, which have more than doubled since 2010/11. In 2017 the government published the Naylor Review to help develop a new strategy for NHS estates, which reinforced the need for the NHS to dispose of surplus land to free up more funding for capital. Financial pressures have meant that NHS organisations are sometimes incentivised to sell land and assets to the highest bidder as an opportunity to plug funding gaps.
At the same time, there is now greater emphasis on how unused or surplus NHS land can be used to widen access to affordable housing. The Naylor Review recommended that any NHS land that is sold should be developed into housing for NHS staff as a priority, and that 30,000 homes could be built on land belonging to acute estates. This would support broader government aims to accelerate the development of new housing across the UK and help achieve the Department of Health and Social Care’s aims of releasing NHS land to build 26,000 more homes by 2020. According to 2019 figures, NHS trusts have nearly 890 hectares of surplus land that could be sold or converted. Lack of affordable housing has compounded the recruitment and retention challenges currently facing the NHS, providing further impetus to use surplus estate to develop housing for staff, particularly clinicians.
However, ownership and control of NHS estates is complex, with important implications for how property can be sold and repurposed for community benefit. NHS trusts own most of the land they occupy, though this is not the case with general practices, which typically lease land from NHS Property Services (which owns and manages over 10% of all NHS estate), community health partnerships or owners outside of the NHS. This means that the opportunities to implement anchor strategies will look different across the sector, as accountability sits with different NHS organisations.
Moreover, since the 1990s, NHS organisations have used private finance initiatives (PFIs) to fund building development. PFIs allow the NHS to use private finance to fund capital projects, and usually mean that NHS organisations only obtain full ownership of the asset once payments have been completed (typically 30 years). This places further constraints on the ability of some NHS organisations to use their estate for broader community benefit.
Given the context, it is not surprising that we see fewer examples of NHS organisations adopting anchor practices on the use of land and estates compared with areas like employment. However, there are opportunities to think differently about how the NHS leverages its assets for social benefit.
Learning from practice
Expanding community access to NHS property
- Enabling local groups and businesses to use NHS estates
The NHS often has facilities that are not used at certain times (such as weekends), which means it can offer the space to community groups at little or no cost. This could make a big difference to small local charities and organisations that otherwise would have no access to space, and help enhance social networks locally.
For example, University Hospitals Birmingham NHS Foundation Trust regularly gives community groups free use of its buildings and facilities, allowing charities to host their annual conferences there. It is also looking into hosting free film screenings for the community in unused lecture theatres. Some trusts are also allowing local schools to use their space in the evenings and at weekends for arts programming.
Another way the NHS can support staff and the wider community is by offering childcare facilities on site, increasing the provision of childcare available in the local community. Sussex Community NHS Foundation Trust, for example, offers nursery places on three sites for NHS and emergency services staff, also reserving some places for local families.
As an anchor, the NHS can also support community development by leasing its retail space to local community businesses, thereby encouraging patients, staff and visitors to spend local. Some hospitals host farmers’ markets on trust estates that are open to the broader community. Cambridgeshire Community Services NHS Trust, after consulting with the community advisory group, is opting to work with a locally owned cafe rather than a large national chain while rebuilding a community hospital.
Some NHS organisations have reported that PFI contracts can restrict their ability to allow local businesses to sell on-site due to exclusivity clauses (although some NHS organisations have been able to negotiate access for local businesses on PFI-owned sites). For example, Southmead Hospital in North Bristol worked with PFI contractors to negotiate a weekly local farmers’ market on-site for patients and visitors using locally sourced produce. The trust had to demonstrate how the farmers’ market would not be in direct competition to existing shops within the hospital. To help make the produce more affordable for residents, the farmers’ market agreed to reduce profit margins to help expand access to healthy food within the trust and community. In exchange, the trust provides volunteers to help run the stall.
Converting and selling estate for community benefit
- Supporting access to affordable housing or housing for key workers using NHS estate
Given the links between housing and health, there is a case for NHS organisations to ensure that their decisions around land use support the needs of their staff, the local community and, over time, contribute to reducing health problems from poor housing. Our interviews with stakeholders revealed that where such efforts are taking place, they are often motivated by more immediate issues of improving recruitment and retention, rather than part of an anchor mission to tackle inequalities:
‘We are absolutely struggling to recruit nurses because no nurses can afford to live and work in some areas, so it is in our interest to somehow build affordable housing, so you can subsidise nursing staff to live in the community, which means they’re not going to be struggling to recruit those staff.’
Deputy director of strategy
NHS England
There are opportunities to align the NHS’s strategic priorities around workforce with broader social objectives, and some NHS organisations are explicitly prioritising social value as part of decisions to sell land. For example, when NHS Property Services sold the former St George’s hospital site in Hornchurch for £40m (the largest reinvestment in the NHS through sale of surplus land), 15% was allocated for social housing and 1.6 hectares of land retained to host a new community health centre.
When selling surplus land, or redeveloping its own land, the NHS could more actively consider social value and the impact on the wider community – though doing so is not always straightforward. Stakeholders we interviewed expressed concern that most NHS land sold by trusts does not include affordable housing provision. A New Economics Foundation analysis of NHS surplus land sales in 2017/18 found that of the sites with planned homes, two-thirds will be unaffordable for nurses on an average salary. Even when there are provisions for affordable housing embedded in the sale agreement, it is not always achieved. For example, in West Yorkshire, a large housing developer committed at the point of sale to building 30% affordable housing on the site of Pontefract General Infirmary – a figure later reduced to 6% after declaring ‘financial unviability’. Strong accountability mechanisms are necessary to ensure that the full social value of NHS estates can be realised after sales are completed. NHS organisations will not always have full control over decisions on the use of their surplus estate for affordable housing, as local authorities often have the primary role. This makes developing partnerships ever more important in delivering these aims.
Converting NHS land and facilities for community use can also require significant upfront investment that many NHS organisations cannot afford in the current financial climate. Stakeholders emphasised the overriding pressures in the NHS from system leaders and trust boards to sell any surplus land on the open market to the highest bidder, even if gains are short-term:
‘We’ve engaged with housing associations, we’ve engaged with primary care associations, all are very keen for us to promote and take forward plans to develop affordable housing. We find ourselves slightly thwarted by the centre… They are completely focused on today’s agenda as opposed to a more broad, long-term view.’
Deputy director of planning
Acute trust
Housing associations, local councils and other community organisations often miss out on development opportunities as they have fewer resources than private developers to make competitive bids. However, interviewees said there is scope for the NHS to pursue alternatives to open market sale and enter into joint ventures with housing associations or councils, who may be able to help attract upfront investment for the development of housing and community spaces. This could help ensure that more of the NHS’s land benefits the community; for example, the NHS could sell land to or enter a leasing arrangement with housing associations, who then develop the land themselves and give the NHS a share of the rental income. However, the need to offset current deficits may severely limit these options. Interviews and learning from the grey literature suggest that, where this is possible, partnerships tend to be more successful if the housing association and the NHS have long-standing relationships and the housing association can make a clear financial case which directly benefits the individual NHS provider.
- Working in partnership across a place to maximise the wider value of NHS estates
Beyond the sale of surplus assets, NHS organisations in some areas are working proactively with other anchors to help improve the local built environment to support community health and wellbeing.
At the national level, NHS England’s Healthy New Towns programme is bringing together NHS providers, commissioners, local government and other partners to test how new housing developments can advance population health through 10 demonstrator sites. The NHS Long Term Plan committed to publishing guidance based on learning from the programme to help other local areas work together to develop healthier built environments. There will also be a new quality standard to incentivise future developments that support prevention.
Cambridgeshire Community Services NHS Trust is negotiating with the Ministry of Defence and the local council, which own adjacent land, to manage the whole site as one plot on which to rebuild a smaller hospital and develop affordable housing. While the circumstances in Cambridgeshire are specific, with strong historical relationships, they highlight the potential for the NHS to partner across a place and to think differently around land use when opportunities arise. STPs and ICSs may provide further scope for the NHS to build these relationships and work more collaboratively to improve local planning and the built environment for health.
If NHS organisations are to make the most of opportunities to use their estate for public good, then meaningful public engagement during the planning process is essential. This has been an important lesson from Healthy New Towns, which highlighted the importance of developing a shared vision with local people on how space can be used, and actively involving communities and residents in decision making on new developments. Partnerships and local stewardship can unlock this, particularly with marginalised and underrepresented communities, as local councils and housing authorities may have different relationships with the community and can be instrumental in forging new links.
- Developing accessible community green space
Given the positive associations between quality green space and health and wellbeing outcomes, some NHS organisations are exploring how they can create more accessible community parks. These green spaces provide a habitat for wildlife and space for physical activity, and contribute to improved health and wellbeing, particularly for people who otherwise would not have access.
Some NHS sites have existing green space that they have opened to the local community, and others are working to develop green space on unused land. For example, Bromley-by-Bow Centre – a GP practice and community charity based in a socially deprived area in east London – owns 3 acres of land that it has converted into green space, with a children’s play area, an allotment and garden. And at a primary care centre near Sunderland, staff worked with NHS Property Services and a local charity, Groundwork, to convert derelict space into a community garden and allotment. The space is now used to run a gardening course as part of a community mental health recovery programme.
Summary and implications for practice and policy
Taking a broader view of the socioeconomic value of NHS capital and estate can be difficult. The demands placed on NHS capital and lack of capital funding puts pressure on the system to immediately dispose of surplus land, typically to the highest bidder. While these pressures will continue, there are examples of good anchor practices where NHS organisations are supporting the development of affordable housing and other community assets and doing more to open their doors to community organisations. However, there is more that can be done.
Nationally, NHS policymakers can support local action by providing clear guidance and clarity to NHS organisations on how to embed provisions for social value into sales and monitor their implementation, and signal this as a priority.
At the local system level, NHS organisations can work with other public sector partners to develop joint strategies that optimise the use of public estate for broader social objectives, such as affordable housing and green spaces. This can also help with immediate organisational pressures around staff recruitment or retention.
For individual organisations, knowing how best to leverage land and estates for social value starts with a detailed understanding of existing estate portfolios to see what can be opened for community use or converted from surplus land. NHS organisations should build relationships with housing associations and local councils to pursue alternatives to open market sale. They should also engage in discussions with local residents to explore community needs for space, and how NHS land and estates can be used to meet those needs.
|
Practical resources to support implementation |
|
Housing Associations and the NHS: New Thinking, New Partnerships (The Smith Institute) Putting Health into Place. Introducing NHS England’s Healthy New Towns programme (TCPA, The King’s Fund, The Young Foundation, Public Health England, NHS England) Supporting the Healthy New Towns programme (The King’s Fund) |
Chapter 6: The NHS as a leader for environmental sustainability
Why this matters
NHS organisations have a significant impact on the environment and are some of the largest contributors to climate change and air pollution. The NHS alone is responsible for 40% of public sector emissions in England.
Delivering high-quality health and care places numerous demands on natural resources and the environment, such as:
- use of energy, water and consumables, including plastics
- waste production and waste management
- travel, which requires fossil fuels and contributes to air pollution.
In 2017, the health and social care system used 27.1 million tonnes of CO2e and 2.23 billion m3 of water. This includes 589,000 tonnes of waste and 9.5 billion travel miles generated by NHS providers. Indeed, health and care-related travel constitutes around 5% of all road travel in England. Given its large carbon footprint, any action the NHS takes to support responsible consumption and reduce waste can have a significant impact on the environment. This is important not only to reduce the carbon impact, but to support more sustainable utilisation of finite resources overall.
The climate crisis has serious direct and indirect consequences for health. Toxic air pollution is associated with acute and chronic health conditions that cost health and social care £157m in 2017. Exposure to air pollution is estimated to cause the equivalent of 40,000 premature deaths in the UK each year, and more than 2,000 GP practices and 200 hospitals are in areas affected by toxic air., Climate change and air pollution also disproportionately affect disadvantaged and vulnerable populations., These communities are more exposed to climate hazards, more vulnerable to the harms they cause and have relatively fewer resources to cope or recover from their effects, thereby further entrenching inequalities.,, And while improving environmental sustainability will have benefits beyond local populations, it is one of the main ways the NHS has influence as an anchor institution, and can improve the wider determinants of health and support community development. It has the power and responsibility to influence action on a broader scale to reduce its contribution to climate change and protect resources for the health of future generations.
What do anchor environmental sustainability strategies look like in practice?
Adopting sustainable practices within the NHS
- Developing leadership and staff buy-in for environmental sustainability
Influencing sustainable practices in the community
- Helping shape community environments and behaviours and influencing local suppliers
Policy context
Public sector organisations are legally required to deliver environmental sustainability as outlined in the Climate Change Act 2008, which commits the UK to reducing its carbon emissions by 80% by 2050. The legislation has since been amended to introduce a target to bring all greenhouse gas emissions to net zero by 2050. NHS leaders have enacted several changes to help deliver on these aims. NHS England and Public Health England jointly fund the SDU, which helps NHS organisations with expert advice and guidance on how to support environmental and social sustainability. NHS organisations in England are also required by the NHS Standard Contract to produce an annual Sustainable Development Management Plan that sets out how they will reduce carbon emissions. And as previously discussed, Wales, Scotland and England each have legislation in place to promote the social value of public purchasing, including considerations for broader environmental sustainability.
The NHS Long Term Plan re-emphasised the importance of reducing greenhouse gas emissions and air pollution associated with delivering health care, and acknowledged the need for collective action from all NHS organisations to reach these targets. The NHS has made progress over the past decade by reducing its carbon output by 18.5%, though as one of the world’s biggest organisations with one of the largest carbon footprints in the UK public sector, these improvements could go much further if the NHS embraced and developed its role as an anchor institution.
Learning from practice
Adopting sustainable practices within the NHS
- Developing leadership and staff buy-in for environmental sustainability
Reducing the health and care system’s carbon footprint involves taking action in several areas, including improving energy efficiency, supporting more sustainable travel for patients and staff, and reducing waste and water consumption.
As with all complex improvements, changing organisational behaviour to support environmental sustainability needs leadership and commitment from senior leaders., Interviewees told us that responsibility for implementation has often been left to sustainability officers without more senior or board-level support. This has often meant that interventions lack coordination and visibility, and could have a greater impact if they were part of an organisation-wide strategy.
Stakeholders who have managed to get senior leaders on board emphasised the importance of creating a vision that appeals to corporate strategic aims. Clearly linking environmental sustainability to goals around improving health has been helpful for some:
‘I just kept banging my drum (about) the whole 40,000 excess deaths a year in the UK due to air quality. So, that stat always hits home.’
Sustainability lead
Acute trust
There is also a lack of accountability on sustainable development within the system. Despite a strong legal context for action, there are no sanctions or incentives beyond national targets for action on sustainable development, which are insufficient on their own to motivate and drive change. One promising development is that the SDU is developing a dashboard to help organisations understand their baseline, assess their readiness and set individual targets in line with their own goals. This data will amalgamate to STP and ICS level to support greater system accountability and regional planning.
Adopting more sustainable operational practices also relies on staff engagement at all levels, requiring a shift in culture, attitudes and knowledge. Research suggests that staff resistance often comes from feelings of having insufficient knowledge or skills to implement change and not knowing the impact of interventions., Giving teams the tools and resources they need to feel empowered to implement solutions and measure impact is key to supporting the NHS to support environmental sustainability for local communities.
During interviews, senior leaders commented that NHS organisations have often been able to make the greatest progress on reducing local air pollution, partly because this is an area with clearly defined metrics that can more easily demonstrate impact.
There are numerous tools and resources to support teams to reduce pollution. These include the Clean Air Hospital Framework, which offers best practice and guidance on how hospitals can improve outdoor and indoor air quality in key areas like procurement, travel, construction and energy generation. The SDU’s Health Outcomes of Travel Tool supports NHS organisations in measuring the impact of travel and transport, helping to quantify the impact of pollution from different sources and how to reduce them. The SDU is also developing frameworks to support progress in other areas where the NHS can have an impact, including recycling schemes, biodiversity, responsible chemical disposal, responsible construction and conservation.
A number of interviewees felt that action on sustainability has become easier as more staff are aware of the climate crisis and its impact. Organisational champions and communication campaigns have helped build a sense of shared motivation, responsibility and ownership over solutions. The NHS has an important role to play in educating staff about what they can do, both at work and outside of work.
‘When I started here, it was just me and nobody really taking sustainability on… Slowly, got more people on board … After a couple of minutes, you can tell them what it’s about and a lot of people, the light bulb just clicks that it’s just good business; like being efficient and using all your resources whether it be staff, the patients we’re dealing with or the environmental impacts of your actions … The tide turned quite a few years ago.’
Sustainability lead
Acute trust
Examples of action by NHS organisations include promoting use of public transport or walking and cycling to work, monitoring waste generation and recycling rates, and installing more energy efficient heat and power sources. But NHS organisations and local systems could do more to coordinate their efforts. There is also an opportunity for regional and national policymakers and the SDU to share good practice and innovations – something NHS England and NHS Improvement have committed to as part of the NHS Long Term Plan.
Case study 6: University Hospitals of North Midlands NHS Trust and Beat the Cold
University Hospitals of North Midlands NHS Trust has launched an initiative to establish more sustainable and affordable energy sources and reinvest savings in the community. Recognising the links between hospital readmissions during winter and poor heating and living conditions, it worked with residents and the local council to crowdfund for 1,100 solar panels, installed on NHS hospital buildings. By switching to renewable energy, the trust saved nearly £300,000 that was invested into a local charity, Beat the Cold, which tackles cold-related sickness and fuel poverty. This initiative has helped strengthen relationships between the trust and residents. Early evaluation suggests the project has helped achieve savings by reducing the rate of readmissions, particularly among elderly people and other vulnerable groups. Having the support of the chair of the board was essential:
‘It was so important that we had the support of the hospital chairman. On the day we were putting the solar panels up a member of the board tried to stop us… The hospital chairman had to overrule him.’
Business development manager
Beat the Cold
Influencing sustainable practices in the community
- Helping shape community environments and behaviours and influencing local suppliers
As an anchor, the NHS can use its voice to push for broader developments that support the environmental health of local communities. For example, some NHS organisations have advocated for more public transport routes and cycling lanes to NHS hospitals, which benefits individuals’ health as well as the environment. This has knock-on benefits for local public transportation, which research has shown can help improve social inclusion and stimulate economic regeneration in deprived areas.
For example, Epsom and St Helier University Hospitals NHS Trust has been working with local councils to improve public transport links to the hospital for staff and the local community. After receiving repeated complaints about the difficulty of getting to the hospital via public transport, the sustainability officer at the trust negotiated with local councils to pilot a new ‘on-demand’ bus service for residents in Surrey, with a designated bus stop on the hospital site. The staff shuttle bus has become a public bus service, and the trust has negotiated with Transport for London to further extend bus services to the hospital.
Purchasing and commissioning can also be harnessed to influence sustainability practices in the community. The supply chain is one of the biggest components of the health and social care system’s carbon footprint, accounting for 57% of its carbon emissions in 2017, with the largest hotspots being medical instruments and equipment, followed by pharmaceuticals., As discussed in the procurement section, the NHS can reduce some of this by working with local suppliers to reduce its carbon output.
For example, as part of its Care without Carbon strategy, Sussex Community NHS Foundation Trust is working with suppliers to reduce carbon emissions, which make up 60%–70% of the trust’s overall carbon footprint. The sustainability team has embedded sustainability criteria and metrics into the tendering process by setting targets for suppliers to reduce their vehicle emissions over the lifetime of the contract.
Improving environmental sustainability in the wider community requires strong partnership working, and much can be achieved by anchors working together – something we explore in the next chapter.
Summary and implications for practice and policy
As one of the largest public sector resource users and polluters, the NHS must take action to reduce its environmental impact. Beyond changing its own organisational practices, the NHS can drive progress within local communities by using its influence at all levels of the system to advocate for broader changes that promote sustainability and improve the wellbeing of communities, particularly for disadvantaged populations who face the highest levels of environmental risk.
For national bodies, this means moving beyond simply setting national targets on narrowly defined areas such as air pollution to supporting the development of metrics, tools and resources across all domains of environmental sustainability and supporting capability at the front line.
At the local system level, organisations can work together to develop shared goals and strategies to improve environmental sustainability and track their impact. The NHS is also well placed to work with other anchors to influence supplier behaviour and make local transport or infrastructure more environmentally sustainable.
NHS organisations need strong leadership to give visibility to strategies, align efforts with other organisational priorities and maximise the influence of the NHS on environmental sustainability within their local area. Understanding which of their practices and activities have an adverse environmental impact is an important first step; securing engagement and buy-in from staff is also essential to finding solutions. Organisations should educate their staff and offer skills, resources and tools so they can take action.
|
Practical resources to support implementation |
|
Care Without Carbon – our strategy (Sussex Community NHS Foundation Trust) Clean Air Hospital Framework (Global Action Plan) Health Outcomes of Travel Tool (Sustainable Development Unit) |
†† This includes carbon emissions associated with the extraction, processing, assembly, packaging, transport, storage and handling of products and materials that are directly and indirectly consumed by service providers.
Chapter 7: The NHS as a partner across a place
Why this matters
Across each dimension of anchor activity, the NHS can accelerate progress by working with others across a place – both within the NHS and with anchors from other sectors – to scale impact and develop shared approaches. The combined assets of anchor institutions (in terms of local jobs, spending and land) can be significant; working collaboratively can give anchors more reach into the community than they would have individually, and allows sharing of best practice. And by working together locally, anchors can use their collective influence to encourage other organisations in their local economies to adopt similar practices.
Establishing anchor partnerships and collaboratives can be key to developing greater intentionality and shared purpose around an anchor mission. There are, however, some contextual and wider issues around place-based anchor collaboration that must be carefully considered.
What do anchor partnerships look like in practice?
Partnering with other anchor institutions across a place
- Developing anchor collaboratives and networks to support shared approaches locally
Partnering with other NHS anchors
- Developing networks to support shared learning and spread good practice
Policy context
The growing focus on place-based approaches to improve health and economic outcomes, both within and across local areas, has changed the dynamics of how anchor institutions may function and work together across a place.
In some areas, devolution has brought sectors together to think collectively about how to channel assets to improve the wellbeing of local populations. For example, the Greater Manchester devolution deal, which gave the combined authority control over £6bn spend on health and social care in the 10 boroughs, has supported anchors to develop a joint strategy for improving population health and economic prosperity across the city region. But even when health and social care have been incorporated into plans, the NHS has not always actively contributed to broader economic strategy development and discussions.
Likewise, the delivery of the government’s Industrial Strategy relies on place-based approaches and calls on combined authorities and LEPs to come together to develop ways to spur growth across local communities. The extent to which NHS organisations have engaged with LEPs has been mostly limited: very few LEPs have NHS representation on their boards, though there are some exceptions – like in Dorset, where the chief system integration officer for the local CCG is a member., Stakeholders have noted that there is an opportunity for the NHS to take a more active role in supporting the delivery of these place-based strategies, given the significant economic assets they bring, and their powers to improve skills development, innovation, employment and infrastructure to support productivity. Moreover, working in partnership on these strategies can open up opportunities to access new funding streams.
‘We are very much trying to take an approach looking at how the local NHS organisations begin to play their part in shifting conversation. I don’t think what we’ve ever done particularly well in the NHS is to say, “What is the role of our organisation in contributing to the economic success of that area?” I don’t think we’ve made that connection powerfully enough, yet.’
Strategy lead
Combined authority
Within health and care, we have identified a number of opportunities for STPs and ICSs to develop anchor approaches around common aims. These are relatively new forums for partnership working and it is too early to tell whether they will realise their promise of supporting more collaboration around prevention. None of the 2016 STP plans referred explicitly to an anchor mission, and few described initiatives to work on anchor-like strategies to intervene in the wider determinants of health. However, as ICSs are a key part of the delivery mechanism for the NHS Long Term Plan, they may create the incentive for NHS organisations to develop their anchor role and collaborate with local partners for the benefit of local communities.
The emphasis on place, both within the NHS and in broader government policy, creates fertile ground for NHS organisations to think differently about their role in a place. If harnessed effectively, it could provide the conditions needed to support greater collaboration to develop communities and take collective action to tackle inequalities and improve the socioeconomic environments needed for good health.
Learning from practice
Partnering with other anchor institutions across a place
- Developing anchor collaboratives and networks to support shared approaches locally
Anchor institutions in several UK cities have started to work more closely to combine their influence and scale impact in local communities. This has often taken a range of forms including collaboratives, networks and economic coalitions, with shared objectives around a common anchor mission.
For example, in Sheffield the NHS has joined with local universities, housing associations, colleges, the city council, chamber of commerce and voluntary sector organisations to drive a collective commitment to building a more inclusive local economy. Led by the city council, the Sheffield City Partnership has developed a framework with a vision, commitments and shared objectives for implementing a city-wide approach to: education, skills and work; environmental sustainability and inequality; procurement; and homelessness and violent crime. The framework provides focus for working together around an anchor mission. It is also being underpinned by extensive engagement with local people to help identify what an inclusive economy would mean for them, and help define common standards and indicators to help track progress and ensure that resources are invested in the areas that could bring the greatest community benefit.
While the potential benefits of greater collaboration between anchors are clear, a range of structural and contextual factors conspire to make partnering around an anchor mission difficult. For one, each anchor has different accountability and governance mechanisms that affect their ability to develop and implement anchor strategies. Across each category of anchor activity, organisations will be accountable to different stakeholders, require different administrative processes and have different financial constraints, affecting their ability to work together across a place.
Having a clearly defined geographical area can help focus efforts, but the geographical footprint and population that each anchor works to, even when in the same locality, can vary.
‘We are all trying to get the best spend of our local pound, really, but there are challenges with that. We have different footprints – at the trust we are part of the ICS footprint, which is a different footprint from the city region. So, we have this constant footprint debate, which plays out when you’re trying to articulate the governance framework, the accountability, the permissions, and who has the authority to make decisions.’
Deputy chief executive
Acute provider trust
This is why stakeholders have emphasised that when developing collaborative approaches, it can be helpful to be flexible, by establishing common objectives and minimum standards for advancing anchor goals but allowing each organisation to determine the most appropriate path to implementation.
Without pre-existing relationships, collaboration at any level is even harder, and so a first step for anchor institutions is to find the time and space to foster working relationships. The exact method will vary, but it is often less about setting up new forums or mechanisms for collaboration and more about identifying those places where different anchor institutions already come together and using those as building blocks to build alignment around an anchor mission. In the current context, this may include health and wellbeing boards, local partnership boards, LEPs, or STP and ICS boards. Regardless of the forum, stakeholders emphasised the need to have the space and time to co-develop a shared vision to drive successful collaboration.
‘There are a lot of potential benefits to STPs and ICSs for developing anchor partnerships and approaches, but I don’t think we’ve realised them yet… But we probably just haven’t had enough space and time to think all that through well.’
Non-executive director
Acute trust
Building these relationships undoubtedly takes significant time, and it can be difficult to establish trust, respect and mutual understanding in the short term. Evaluations of the Greater Manchester devolution deal found that Manchester’s strong sense of place and 30-year history of partners working together was pivotal to delivering the plan and linking up policies to improve population health and wellbeing.
Given the different structures and focus of anchor organisations, it can also be difficult to know the best level at which to engage within each organisation around place-based strategies. Interviewees from outside the NHS said it is not immediately clear who holds responsibility or the most relevant expertise. Having a designated anchor or sustainability lead within NHS organisations can help, as it makes it obvious who to start conversations with, in cases where the NHS has not always taken part (for example, as part of LEPs).
Relationships have also been helped by working with third-party organisations who can act as a convener and facilitator and provide much-needed additional capacity to support partnership working. For example, the Joseph Rowntree Foundation has worked with Leeds (see case study 7) and CLES with places like Birmingham and Preston to bring different anchors together to provide forums for discussion and develop a common approach.
Local government has also frequently been an important driver of cross-sector collaboration, as in Sheffield, where councils have linked anchor partnerships to broader strategies around supporting more inclusive community development. NHS stakeholders we interviewed noted that when working in partnership, it is essential to recognise the value and expertise that other sectors bring, and be willing to work as equal partners alongside other sectors:
‘You know, (NHS organisations) should be partners, and we are partners with our local community. We shouldn’t be putting ourselves up on a pedestal, and then there’s a risk of that sometimes … we have a lot to contribute to the local growth agenda and the sustainability agenda, but we should do that in partnership.’
Deputy chief executive
Acute trust
Collaborative anchor approaches have been developed in procurement, where NHS organisations are working with other anchors to maximise the social value of public spend. Adopting joint progressive procurement strategies can help retain more money locally while also sending a collective market signal that social objectives are a priority, which can influence supplier behaviour. For example, in Birmingham, partners across the STP have agreed to apply a 10% social value weighting in their contracts and use procurement to meet shared social aims, including increasing the number of apprenticeships, recruiting more people from vulnerable populations and lowering carbon emissions.
By working collaboratively, anchor organisations can help build a common language for social value and reduce variation in how the concept is understood and applied in practice across a health economy. Interviews with stakeholders revealed that commissioners and providers often use a mix of approaches that contribute to a lack of clarity in how to interpret social value while also unnecessarily duplicating efforts. For instance, in one local area, a trust had to respond to two local authorities with different requirements for social value to deliver the same sexual health service:
‘The service specification looked exactly the same, but we had to report different types of evidence to show how we would meet standards for social value. This required a degree of expertise in how to respond to contracts, that thankfully we had, but not all providers do. It also created inefficiencies without changing anything fundamental about our approach to social value or increasing the community benefit we would bring in the way we delivered the service.’
Head of sustainability
Acute trust
STP and ICS leadership can help establish common standards while reducing duplication by coming up with contracting templates that can be adapted by anchors across the partnership.
Case study 7: Leeds City Region anchor framework
In Leeds, anchor organisations from across the city have formed an anchors collaborative and agreed common goals for supporting inclusive development. Working with the Joseph Rowntree Foundation, the collaborative developed a tool for partners to self-assess how they perform on five anchor dimensions (employment, procurement, capital, service delivery and corporate responsibility), visualise where they want to be and identify what actions they can take to get there. The framework has also helped anchors establish common goals and have a broader impact by sending a powerful collective signal to the local economy that narrowing inequalities and supporting inclusive economic development are priorities. To support this effort, Leeds City Council has also created a data dashboard so that areas with the greatest needs and inequalities can be targeted.
Though the framework establishes clear goals and specific actions for all partners, flexibility in how the tool is adapted and applied within each organisation is key.
Case study 8: Birmingham anchor network
A new network has formed in Birmingham to explore how six anchors can work together, including Queen Elizabeth Hospital, Birmingham City Council, the police, University of Birmingham, local colleges and the local housing association. This network builds on work these organisations have done with the Centre for Local Economic Strategies (CLES) funded by the Barrow Cadbury Trust to map their collective assets and understand their baseline contribution to the Birmingham and West Midlands economy. With combined annual budgets of £6bn and more than 50,000 employees, the network will support anchors to develop individual strategies and advocate for an anchor approach on workforce, procurement and management of land and assets. One collective priority is around construction, as a significant proportion of money leaks from the local economy from new building projects, and the upcoming Commonwealth 2022 games in Birmingham present an opportunity to shift practice. The network is also developing ways to measure the impact of different approaches to better understand how anchor practices can benefit communities.
Partnering with other NHS anchors
1. Developing networks to support shared learning and spread good practice
In addition to coming together across a place, there is an opportunity for NHS organisations to work together to develop their collective identity as anchor institutions to tackle common issues. Peer networks can be a powerful tool in generating knowledge and supporting a culture of learning. However, there is currently no formal network of health care anchors in the UK. The NHS Confederation and the SDU have been convening NHS organisations to facilitate shared learning, provide expertise and develop skills around local economic development and environmental and social sustainability, but our interviewees felt there could be more collaborative networks and communities of practice to help make an anchor mission an institutional priority across the NHS.
In the United States, The Democracy Collaborative (TDC, which supports a network of more than 40 health care systems) could serve as a model for the NHS. These health systems together employ 1.5 million people and purchase over $50bn worth of goods and services annually. The network allows health care organisations to share knowledge, work through common challenges, identify areas for joint working and co-develop tools that can be adapted by each organisation to accelerate progress. A key aim is to help members drive culture change within their respective organisations and adopt more intentional and conscious anchor strategies within their health system’s overarching strategy. Since its inception, members have implemented changes in their local areas, including investing in affordable housing, committing to living wages for all staff and creating new career pathways for non-clinical entry-level roles.
In the UK, there are also examples of anchor collaboration within other sectors. For instance, 37 vice-chancellors recently signed a Civic Universities Statement Agreement pledging to prioritise the social, economic, environmental and cultural life of their local communities. This includes specific commitments to collaborate with each other and other anchor institutions to support their aims. There are also dedicated programmes and networks in local government, housing, and the arts and culture sectors.
Summary and implications for practice and policy
NHS organisations can work with each other, and with other anchor organisations across a place, to share learning and establish common goals so that the anchor mission more directly informs how the NHS functions within a place. As many of the examples have demonstrated, where individual institutions have come together to collaborate on a shared vision and work together to hold each other to account, the benefits can be significant.
There is a real opportunity to capitalise on STPs and ICSs to help the NHS forge new partnerships across a place and develop shared approaches and anchor strategies as part of broader system plans. Anchor strategies may also provide a gateway for the NHS to take part in other place-based strategic discussions, including with LEP, to help align approaches with broader economic proposals that improve the health and wellbeing of communities. National leaders should work with partners to create space for NHS organisations to come together to share and spread ideas through action learning and to work through challenges unique to the NHS context.
|
Practical resources to support implementation |
|
A Partnership Framework for an Inclusive and Sustainable Economy (Sheffield City Partnership) Anchor Collaboratives: Building Bridges with Place-Based Partnerships and Anchor Institutions (The Democracy Collaborative) Community Wealth Building Through Anchor Institutions (Centre for Local Economic Strategies) Health In All Local Industrial Strategies? (NHS Confederation) Healthcare Anchor Network (The Democracy Collaborative) Leeds City Region Anchor Institution Progression Framework (Leeds City Council) Local Growth Academy (NHS Confederation) Learning from other sectors Civic University Agreements – List of Signatories (Civic University Commission) Great Places Commission Interim Report (National Housing Federation) Inquiry into the Civic Role of Arts Organisations. Phase 2. What Happens Next? (Calouste Gulbenkian Foundation) Leading Places programme (Local Government Association) Local Access (Big Society Capital and Access) |
‡‡ The NHS Confederation’s Health in all local industrial strategies? briefing offers examples of how health intersects with local industrial strategies and ways the NHS can engage with LEPs to shape their development around mutual aims. Source: www.nhsconfed.org/-/media/Confederation/Files/Publications/Documents/Health-in-all-local-industrial-strategies.pdf
Conclusion: actions and opportunities for change
Consciously adopting an anchor mission
In this report we have explored a range of opportunities for the NHS to harness its considerable influence to have an even greater impact on the health and wellbeing of communities. There are many anchor activities already taking place across the sector that provide an important foundation on which the NHS can build. NHS organisations are all at different stages in embracing their role as anchors, but where strategies are being adopted, they tend to be discrete and narrow in scope, rather than joined up and embedded as part of central, local system or organisational strategies. Anchor approaches are often being applied in one area only (for example, workforce). While NHS organisations will have to start somewhere, the greatest impact will come from pursuing changes in each domain of anchor influence and with other anchors and partners across a place. It is also the case that anchor practices are not yet being evaluated systematically to understand what actions have the strongest impact on population outcomes. More needs to be done to help NHS organisations cultivate an anchor mission and know where to prioritise efforts, both within their organisations and in their local communities.
This report has also identified cross-cutting opportunities – regardless of the area of anchor activity being pursued – to make anchor practices more embedded in the NHS, and these are summarised below. While most actions will be delivered at the level of NHS organisations and networks, national, regional and local system leaders have a strong role in signalling the anchor mission as a priority and supporting an environment where these changes can happen. These opportunities are set out in Table 4.
Adopting new ways of working for an anchor mission requires time, resources and upfront investment that can be hard for NHS organisations to come by. The report has highlighted tensions the NHS may have to work through to balance priorities and direct its anchor efforts (described in Table 3). These tensions play out at different levels of the system and are not always inevitable, but when they do arise can often be mitigated or managed with careful implementation and planning. For instance, the NHS can boost international recruitment to address shortages in certain jobs and geographies while also taking steps to increase local workforce supply over the long term. The examples given throughout the report show how the NHS can shift practice by taking a pragmatic approach and aligning anchor practices with other system goals.
Table 3: Potential tensions between anchor practices and the current policy/practice context
|
Anchor practices |
Tensions to balance |
|
A desire to develop the local labour market and create pipelines into NHS jobs and careers. |
The need to fill vacancies quickly to address severe workforce shortages requires a focus on external labour sources, including international recruitment. |
|
An aspiration to increase social value by taking a wider range of factors into account when making decisions on purchasing and procurement. |
A push to reduce costs and increase efficiency, given the wider economic climate and financial pressures on the health service. |
|
A desire to increase capability in the local supply chain, leading to more local purchasing and procurement. |
A need to avoid potentially anti-competitive behaviour. |
|
A focus on developing strong and resilient local places in specific geographical areas. |
The risk of widening inequalities (as those places with the largest or best-resourced anchors will benefit most and may draw resources away from neighbouring areas). |
|
A desire to allow flexibility for NHS anchors to adapt activity to meet local context and local needs. |
A national drive for greater standardisation of activities to reduce variation. |
What can the NHS do now to develop its role as an anchor?
- Build a baseline understanding of current practice to know where to prioritise action and establish informed goals.
Data are key to helping organisations understand their baseline levels of activity and assess their readiness to change. Baseline audits can generate information on purchasing behaviour, use of estates, employment practices and environmental impact. This can then inform goal-setting and targets for shifting behaviours based on current levels of practice.
Baseline data can also help signal where there may be more immediate opportunities and where change will have to happen over the longer term. NHS organisations may find it easier to start in domains such as employment, where there is clear data on vacancies and local unemployment to show where to target efforts, and where anchor actions align with broader organisational strategies. Within procurement, NHS organisations can use data to establish achievable targets of how much spend can be shifted locally, identifying which contracts are up for renewal that may lend themselves to working with local suppliers. People with improvement skills are well placed to support the development of aims and measures to inform goals, and the ability to facilitate change.
- Develop metrics and evaluate the impact of interventions
Data are also vital for measuring the impact of interventions and building the business case for future investment. National leaders can help establish metrics in each area of anchor activity for local NHS organisations and STP/ICS leads to use to assess progress, and fund evaluations of the wider impact and return on investment. This could build on existing work such as the framework developed in Leeds (see page 55) that defines metrics across different anchor dimensions to help organisations measure progress around shared goals. Within procurement, some local system leaders have already defined metrics to help guide purchasing decisions and build an understanding of the broader social impact of public spend (see Chapter 4). STPs and ICSs can help track progress across a place by creating dashboards that pool data from partner organisations and help guide future strategy. Evaluation requires significant resources and time, so it is important that teams are funded and supported with the skills and capacity necessary to use data effectively to inform decision making.
- Establish clear and visible leadership to embed anchor practices within organisational and system strategies
Leadership is needed at each level of the system to make anchor practices visible and an integrated part of organisational and system strategies. Unless leaders see an anchor mission as a core part of the NHS’s role and responsibility to local communities, little will be achieved. At the organisational level, gaining board support will be an essential early step to ensure that efforts are adequately resourced and prioritised over the long term. Nominating a board-level lead for anchor strategy can help cement that support, while raising the profile of anchor practices across the organisation and connecting them up. Beyond board support, having a designated manager – for example, an anchor or sustainability lead – to oversee and coordinate anchor practices across an organisation can be a key driver in getting efforts off the ground and integrating anchor strategies into operating models.
Linking anchor practices to existing organisational priorities and goals can be useful in gaining senior buy-in. For example, showcasing how anchor practices that build local workforce supply or provide more affordable housing for staff can address staff recruitment and retention challenges at the same time as helping to reduce inequalities, can gain traction for these ideas. And when there are tensions between short-term performance pressures and longer-term improvements to population health, having board-level support can give staff the permission and air-cover needed to prioritise practices in support of an anchor mission.
At the local system level, STP and ICS leads have an opportunity to work with system partners to create a shared view around an anchor mission and embed strategies as part of delivery plans. This requires building consensus around common aims and identifying which anchor strategies are best done in partnership to achieve more ambitious and long-term goals. Local system leaders have a role in articulating a clear vision for inclusive development while permitting flexibility for organisations, to account for different contexts.
While most anchor practices will be delivered at the organisational and local system levels, national leaders can be instrumental in helping to shape the collective vision of how the NHS acts as an anchor and setting expectations about its broader role in the local community. The explicit references to anchor institutions in the NHS Long Term Plan and Interim NHS People Plan are positive developments that help signal the anchor mission as a priority. There may be more opportunities to incorporate an anchor approach into other national frameworks and guidance – for example, through the CCG improvement and assessment framework, or STP/ICS guidance. These frameworks should be backed by proactive support to ensure that teams have the resources and capability needed to support effective implementation. There is also a role for national leaders to help clarify definitions and provide guidance and templates to ensure consistency in anchor practices and how they can be integrated into NHS practice.
- Enable staff to act on a collective vision for enhancing community health and wellbeing
Change will not happen unless staff are engaged in the anchor mission and have the time, skills and capability needed to embed anchor practices within daily roles. The anchor mission may offer an opportunity to tap into employees’ intrinsic motivation, by connecting operational functions like HR, procurement and facilities management to the aims for front-line delivery – that is, improving the health and wellbeing of local communities. One way to do this is to co-produce and design potential solutions directly with staff so that they feel ownership over the challenges and feel part of the collective vision for supporting wider community health and wellbeing.
It is also the case that anchor practices may be new territory for staff, who may need support to incorporate considerations for population health and social value effectively into their daily roles. We have cited numerous resources and tools throughout this report to help staff put these ideas into practice. NHS organisations should use these tools as a starting point, and national and system leaders should ensure that local teams have the skills and capabilities needed to carry out these practice changes and develop methods that support a consistent approach.
Where there are gaps in skills and expertise, working in partnership can also help the NHS build greater capacity. Working with partners can bring different perspectives and skills from outside health care that are invaluable and give NHS organisations greater reach into local communities. Many of the examples of anchor activity we have highlighted involve NHS organisations collaborating with local community, public sector or commercial partners on a specific initiative. Whether this is working with housing associations to ensure that NHS land is developed for affordable housing, or engaging local government around improving public transport for staff and patients, effective partnership is often a core component of success.
- Support the sharing and spread of ideas through networks
Sharing knowledge and ideas can help the NHS more intentionally adopt and apply anchor strategies in practice. Networks could add value and support the NHS to maximise its anchor role at different levels: locally, by convening anchors across a place to support community cohesion, align practices around a shared vision and maximise combined impact; and nationally, to facilitate peer learning and help health care organisations carry out anchor activities more effectively and efficiently.
STPs/ICSs can play a key role in convening and establishing these relationships across anchors in a locality. The introduction of PCNs may also create an opportunity to align operational practices and strategy in general practice around an anchor mission, and feed into broader goals of improving population health at the STP/ICS level. Regional and national leaders are well situated to encourage and support NHS organisations from different localities to convene and share learning and expertise across NHS peers. Whether national or local, networks may benefit from working with an independent third-party facilitator to build consensus and sustain engagement over the long term.
- Engage proactively with communities to ensure that anchor strategies meet the needs of local people and to maximise impact on narrowing inequalities
Maximising the NHS’s contribution to community health and wellbeing requires a deep understanding of local priorities and needs. This means engaging with residents in new ways to explore their needs and developing a shared vision and strategy for how the NHS can be a better partner for and leader in change. For example, being a better and more inclusive employer requires an understanding of the needs of residents who face the greatest barriers to employment. It means getting residents’ views on how NHS estate and land can add most value, and creating access to community spaces for those who need them most. This type of engagement requires connecting with people who are seldom heard and poorly served – something that many NHS organisations may not currently be equipped to do, which makes partnership working and local collaboration essential. Local organisations should prioritise this engagement as part of the design and delivery of different interventions, and local system leaders may also be well placed to coordinate engagement strategies across a place.
Table 4: Opportunities for action by different stakeholders
|
Opportunity |
Action |
For action by |
|
Build a baseline understanding of current practice to know where to prioritise action and establish informed goals |
Conduct internal audits to set targets and goals for shifting practice. |
|
|
Develop metrics and evaluate practices to understand the impact of different interventions |
Continuously monitor and collect data to track impact of anchor strategies, ensuring teams have the resources and capacity needed to make effective use of data and make evaluation a priority. |
NHS provider organisations and networks |
|
Establish dashboards that pool data and track progress across a place. |
||
|
Help define metrics for tracking and measuring impact at the local system and organisational levels. |
||
|
Establish clear and visible leadership to embed anchor practices within organisational and system strategies |
Designate a board-level lead for anchor strategy and operational lead to help coordinate and align efforts across an organisation. |
NHS provider organisations and networks |
|
Embed anchor strategies as part of local system plans to help deliver broader aims on population health and prevention. |
Local system leaders |
|
|
Establish clarity around common definitions to build system understanding of what anchor practices look like, and how they support broader social value and community benefit. |
National policy makers |
|
|
Send clear signals through national policy, guidance and frameworks that the anchor mission is a priority for the NHS. |
National policy makers |
|
|
Enable staff to act on a collective vision for enhancing community health and wellbeing |
Co-design solutions directly with teams, appealing to intrinsic motivation among staff. |
NHS provider organisations and networks |
|
Use existing tools, resources and guidance to build capability, awareness and knowledge around anchor practices. |
NHS provider organisations and networks |
|
|
Work in partnership with other organisations that may have greater community reach or skills and expertise to support implementation of anchor practices. |
NHS provider organisations and networks Local system leaders |
|
|
Deliver support programmes that equip teams with the resources, skills and expertise needed to operationalise anchor practices and strategies. |
National policy makers Local system leaders |
|
|
Support the sharing and spread of ideas through networks |
Establish place-based networks that convene anchors across a locality to develop a shared vision and objectives for improving community health and wellbeing. |
Local system leaders |
|
Encourage and support NHS organisations to convene through networks to learn and share practice for applying anchor strategies in the NHS context. |
National policy makers |
|
|
Engage proactively with communities to ensure that anchor strategies meet local needs and to maximise impact on narrowing inequalities |
Work in partnership to engage with communities, particularly seldom heard groups, to ensure that all residents have a voice in shaping anchor approaches and strategies. |
Local NHS providers and networks Local system leaders |
References
- Department for Work and Pensions. Households Below Average Income: An Analysis of the UK Income Distribution: 1994/95-2017/18. GOV.UK; 2019 (www.gov.uk/government/statistics/households-below-average-income-199495-to-201718).
- Office for National Statistics. Health State Life Expectancies by National Deprivation Deciles, England and Wales: 2015 to 2017. ONS; 2019.
- Local Government Association. Leading Places programme [webpage]. Local Government Association (www.local.gov.uk/topics/devolution/leading-places).
- Civic University Commission. UPP Foundation Civic University Commission [webpage]. Civic University Commission (www.upp-foundation.org/civic-university-commission).
- Marmot M. Fair Society, Healthy Lives: The Marmot Review. Strategic Review of Health Inequalities in England Post-2010. The Marmot Review; 2010 (www.gov.uk/dfid-research-outputs/fair-society-healthy-lives-the-marmot-review-strategic-review-of-health-inequalities-in-england-post-2010).
- Acheson D. Independent Inquiry into Inequalities in Health. The Stationery Office; 1998 (www.gov.uk/government/publications/independent-inquiry-into-inequalities-in-health-report).
- Black D. Inequalities in Health. Department of Health and Social Security; 1980.
- Office for National Statistics. Socioeconomic Inequalities in Avoidable Mortality, England and Wales: 2001 to 2016. ONS; 2018 (www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/causesofdeath/articles/measuringsocioeconomicinequalitiesinavoidablemortalityinenglandandwales/2001to2016).
- Canadian Institute of Advanced Research, Health Canada, Population and Public Health Branch. AB/NWT 2002. In: Kuznetsova D. Healthy Places: Councils Leading on Public Health. New Local Government Network; 2012.
- Kindig DA, Booske BC, Remington PL. Mobilizing action toward community health (MATCH): Metrics, incentives, and partnerships for population health. Preventing Chronic Disease. 2010; 7(4): A68.
- McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Affairs. 2002; 21(2): 78–93.
- Bunker JP, Frazier HS, Mosteller F. The role of medical care in determining health: Creating an inventory of benefits. In: Amick BC, Levine S, Tarlov AR, Walsh DC (eds.) Society and Health. Oxford University Press; 1995.
- NHS England. Long Term Plan Implementation Framework [webpage]. NHS England; 2019 (www.longtermplan.nhs.uk/implementation-framework/).
- Bramley G, Hirsch D, Littlewood M, Watkins D. Counting the Cost of UK Poverty. Joseph Rowntree Foundation; 2016 (www.jrf.org.uk/report/counting-cost-uk-poverty).
- The Health Foundation. Infographic: Poverty and Health: How do our Money and Resources Influence our Health? The Health Foundation; 2018 (www.health.org.uk/infographic/poverty-and-health).
- Office for National Statistics. Health State Life Expectancies by National Deprivation Deciles, England and Wales: 2015 to 2017. ONS; 2019.
- Charlesworth A, Firth Z, Gershlick B, Watt T, Johnson P, Kelly E, et al. Securing the Future: Funding Health and Social Care to the 2030s. The Health Foundation/Institute for Fiscal Studies; 2018 (www.health.org.uk/publications/reports/securing-the-future-funding-health-and-social-care-to-the-2030s).
- GOV.UK. Prevention Is Better Than Cure: Our Vision to Help You Live Well for Longer. Department of Health and Social Care; 2018 (www.gov.uk/government/publications/prevention-is-better-than-cure-our-vision-to-help-you-live-well-for-longer).
- NHS England, Care Quality Commission, Health Education England, Monitor, NHS Trust Development Authority, Public Health England. NHS Five Year Forward View. NHS England; 2014 (www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf).
- NHS England. NHS Long Term Plan. NHS England; 2019 (www.longtermplan.nhs.uk).
- Department for Business, Energy and Industrial Strategy. Industrial Strategy: The grand challenges. GOV.UK; 2019 (www.gov.uk/government/publications/industrial-strategy-the-grand-challenges/missions#ageing-society).
- Cabinet Office and Department of Health and Social Care. Advancing our health: prevention in the 2020s – consultation document. GOV.UK; 2019 (www.gov.uk/government/consultations/advancing-our-health-prevention-in-the-2020s/advancing-our-health-prevention-in-the-2020s-consultation-document#fn:26).
- The Health Foundation. A healthy economy needs a healthy population to power it. Health Foundation responds to government's prevention green paper. The Health Foundation; 23 July 2019 (www.health.org.uk/news-and-comment/news/a-healthy-economy-needs-a-healthy-population-to-power-it).
- Commissioner for Wales. Deddf Llesiant Cenedlaethau’r Dyfodol. Well-being of Future Generations (Wales) Act 2015 (https://futuregenerations.wales/about-us/future-generations-act).
- Scottish Government. Fairer Scotland Duty: Interim Guidance for Public Bodies [webpage]. Scottish Government; 2018 (www.gov.scot/publications/fairer-scotland-duty-interim-guidance-public-bodies/pages/1).
- Briggs ADM, Alderwick H, Fisher ES. Overcoming challenges to US payment reform: Could a place-based approach help? Journal of the American Medical Association. 2018; 319(15): 1545–1546. doi:10.1001/jama.2018.1542.
- Samans R, Blanke J, Corrigan G. The Inclusive Growth and Development Report. World Economic Forum; 2015 (www3.weforum.org/docs/WEF_Forum_IncGrwth_2017.pdf).
- UK 2070 Commission. Fairer and Stronger: Rebalancing the UK Economy. UK 2070 Commission; 2019 (http://uk2070.org.uk/2019/05/30/first-report-of-the-uk2070-commission-to-be-published-on-thursday-30th-may-2019).
- United Nations Department of Economic and Social Affairs. Leaving No One Behind: The Imperative of Inclusive Development. Report on the World Social Situation 2016. UNDESA; 2016 (https://doi.org/10.18356/d2c06f02-en).
- Royal Society for the Encouragement of Arts, Manufactures and Commerce. Inclusive Growth Commission: Making our Economy Work for Everyone. RSA; 2017 (www.thersa.org/discover/publications-and-articles/reports/final-report-of-the-inclusive-growth-commission).
- Jackson M. Creating a Good Local Economy: The Role of Anchor Institutions. Centre for Local Economic Strategies; 2015 (www.cles.org.uk/publications/creating-a-good-local-economy-the-role-of-anchor-institutions).
- Ministry of Housing, Communities and Local Government. Strengthened Local Enterprise Partnerships. GOV.UK; 2018 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/728058/Strengthened_Local_Enterprise_Partnerships.pdf).
- Lupton R, Hughes C, Peake-Jones S, Cooper K. City-Region Devolution in England. SPDO Research Paper 2. The London School of Economics and Political Science; 2018 (http://sticerd.lse.ac.uk/dps/case/spdo/spdorp02.pdf).
- Cylus J, Permanand G, Smith PC. Making the Economic Case for Investing in Health Systems. What is the Evidence that Health Systems Advance Economic and Fiscal Objectives? Policy Brief. Health Systems for Prosperity and Solidarity. WHO Regional Office for Europe; 2018 (www.euro.who.int/__data/assets/pdf_file/0010/380728/pb-tallinn-01-eng.pdf?ua=1).
- Vaughan M, Hilsenrath P, Ludke RL. The contribution of hospitals to a local economy: a case study in Iowa and Illinois. Health Care Management Review. 1994; 19(3): 34–40 (www.ncbi.nlm.nih.gov/pubmed/7822189). Rotarius T, Liberman A. The financial impact of hospitals on the local economy – 2 new factors. Healthcare Manager. 2014; 33(4): 304–309 (www.ncbi.nlm.nih.gov/pubmed/25350018).
- Office for National Statistics. Public sector employment, UK: June 2018, statistical bulletin. ONS; 2018 (https://bit.ly/2zO1hn9).
- The Health Foundation. Infographic: How Is Work Good For Our Health? The Health Foundation; 2018 (www.health.org.uk/infographic/how-is-work-good-for-our-health).
- The Health Foundation, The King’s Fund, Nuffield Trust. The Health Care Workforce in England. Make or Break? The King’s Fund; 2018 (www.kingsfund.org.uk/publications/health-care-workforce-england).
- Health Education England. The Talent for Care. A National Strategic Framework to Develop the Healthcare Support Workforce. HEE; 2014 (www.hee.nhs.uk/our-work/talent-care-widening-participation).
- Health Education England. Widening Participation. It Matters! Our Strategy and Initial Action Plan. HEE; 2014 (www.hee.nhs.uk/our-work/talent-care-widening-participation).
- NHS England. Interim NHS People Plan. NHS England; 2019 (www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_June2019.pdf).
- Health Education England. Facing the Facts, Shaping the Future: A Draft Health and Care Workforce Strategy for England to 2027. HEE; 2017 (www.hee.nhs.uk/our-work/workforce-strategy).
- Hird P. NHS Pay Review Body. Thirty-First Report 2018. Her Majesty’s Stationery Office. Cm 9641; 2018 (www.gov.uk/government/publications/national-health-service-pay-review-body-31st-report-2018).
- NHS Equality and Diversity Council. Data Analysis Report for NHS Trusts. NHS Equality and Diversity Council; 2018 (www.england.nhs.uk/wp-content/uploads/2018/12/wres-2018-report-v1.pdf).
- Johns Hopkins University and Health System. HopkinsLocal Progress Report: Year Three. HopkinsLocal; 2018 (https://hopkinslocal.jhu.edu/progress-report).
- NHS Employers. Engaging With and Recruiting From Your Local Community. NHS Employers; 2018 (www.nhsemployers.org/your-workforce/plan/recruiting-from-your-community/engaging-with-and-recruiting-from-across-your-local-community).
- Health Education England. Preparation for Work Programmes Analysis, Findings and Recommendations. HEE; 2018 (www.hee.nhs.uk/our-work/work-experience-pre-employment-activity).
- University Hospitals Birmingham NHS Foundation Trust. The Learning Hub [website]. (www.learninghub-uhb.co.uk).
- University Hospitals Birmingham NHS Foundation Trust. Annual Report and Accounts 2017/18. University Hospitals Birmingham NHS Foundation Trust; 2018 (www.uhb.nhs.uk/Downloads/pdf/AnnualReport17-18.pdf).
- East Lancashire Hospitals NHS Trust. Hospital Employment Opportunities for Local Unemployed. East Lancashire Hospitals NHS Trust; 2019 (www.elht.nhs.uk/news-and-media/news/hospital-employment-opportunities-local-unemployed).
- Accenture, The business case for employability programmes in the NHS. Health Education England; 2018 (www.hee.nhs.uk/our-work/work-experience-pre-employment-activity).
- NHS Confederation. Defining the Role of Integrated Care Systems in Workforce Development: A Consultation. NHS Confederation; 2019 (www.nhsconfed.org/-/media/Confederation/Files/Publications/Documents/Defining-the-role-of-integrated-care-systems-in-workforce-development-A-draft-manifesto.pdf).
- Kane M, Bibby J. Listening to our Future: Early Findings from the Health Foundation’s Young People’s Future Health Inquiry. Health Foundation; 2018 (www.health.org.uk/publications/listening-to-our-future).
- Francis-Devine B. Youth Unemployment Statistics. Briefing Paper Number 5871. House of Commons; 2019 (https://researchbriefings.parliament.uk/ResearchBriefing/Summary/SN05871#fullreport).
- The Prince’s Trust. Success Stories – Queen Elizabeth Hospital, Birmingham [webpage]. The Prince’s Trust (www.princes-trust.org.uk/about-the-trust/success-stories/queen-elizabeth-hospital-birmingham).
- NHS Employers. Infographic: Your Future Nurses. NHS Employers (www.nhsemployers.org/-/media/Employers/Publications/Nursing-Supply-Route-Infographic.pdf).
- Andalo D. The NHS apprenticeships offering a new route to health and social care. The Guardian; 5 March 2019 (www.theguardian.com/careers/2019/mar/05/the-nhs-apprenticeships-offering-a-new-route-to-health-and-social-care).
- Beech J, Bottery S, Charlesworth A, Evans H, Gershlick B, Hemmings N, Imison C, Kahtan P, McKenna H, Murray R, Palmer B. Closing the Gap: Key Areas for Action on the Health and Care Workforce. Overview. The Health Foundation, The King’s Fund, Nuffield Trust; 2019 (www.health.org.uk/sites/default/files/upload/publications/2019/Closing-the-gap-key-areas-for-action-overview.pdf).
- NHS Employers. Barts Health NHS Trust: Engaging with Project Search. NHS Employers; 2018 (www.nhsemployers.org/-/media/Employers/Publications/Widening-participation/Barts-Project-Search-case-study-final.pdf).
- C3 Collaborating for Health. Health Professionals [webpage] C3 Collaborating for Health (www.c3health.org/our-programmes/health-professionals).
- The Health Foundation. NHS staff survey shows workforce under pressure. Health Foundation; 2019 (www.health.org.uk/news-and-comment/news/health-foundation-response-to-nhs-staff-survey-2018).
- Jones D, Molitor D, Reif J. What Do Workplace Wellness Programs Do? Evidence From the Illinois Workplace Wellness Study. National Bureau of Economic Research; 2018 (www.nber.org/workplacewellness/s/IL_Wellness_Study_1.pdf).
- NHS Employers. NHS Terms and Conditions (AfC) pay scales – Hourly. NHS Employers; 2019 (www.nhsemployers.org/your-workforce/pay-and-reward/agenda-for-change/pay-scales/hourly).
- Royal College of Nursing Foundation. No Longer Suffering in Silence: A Review of the Lamplight Support Service. RCN Foundation; 2017 (www.rcnfoundation.org.uk/__data/assets/pdf_file/0004/659227/Lamplight-Report_V4_web.pdf).
- Unison. Living on a knife-edge – survey reveals what a pay rise would mean to NHS employees. Unison; 2017 (www.unison.org.uk/news/2017/12/living-knife-edge-survey-reveals-pay-rise-mean-nhs-employees/).
- NHS Equality and Diversity Council. NHS Workforce Race Equality Standard – 2018 Data Analysis Report for NHS Trusts. NHS Equality and Diversity Council; 2019 (www.england.nhs.uk/wp-content/uploads/2018/12/wres-2018-report-v1.pdf).
- NHS Confederation. Chairs and Non-executives in the NHS: The Need for Diverse Leadership. NHS Confederation; 2019 (www.nhsconfed.org/-/media/Confederation/Files/Publications/Chairs-and-non-executives-in-the-NHS.pdf).
- Health Education England. The Topol Review. Preparing the Healthcare Workforce to Deliver the Digital Future. HEE; 2019 (https://topol.hee.nhs.uk/wp-content/uploads/HEE-Topol-Review-2019.pdf).
- NHS England. NHS Test Beds programme. Successful Wave 2 Test Beds [webpage]. NHS England (www.england.nhs.uk/ourwork/innovation/test-beds).
- Care City. Innovation Test Bed Wave 2 [webpage]. Care City (www.carecity.london/what-we-do/live-projects/innovation-test-bed-wave-2).
- NHS England. Partnering with the NHS to sell goods and services. NHS England; 2018 (www.gov.uk/guidance/partnering-with-the-nhs-to-sell-goods-and-services#nhs-procurement-in-england-background).
- Moretti E. Local multipliers. American Economic Review. 2010; 100(2): 373–7. (https://eml.berkeley.edu/~moretti/multipliers.pdf).
- Stuckler D, Reeves A, Mckee M. Social and economic multipliers: What they are and why they are important for health policy in Europe. Scandinavian Journal of Public Health. 2017; 45(18suppl): 17–21.
- Suárez Serrato JC, Wingender P. Estimating Local Fiscal Multipliers. Working Paper. National Bureau of Economic Research; 2016 (www.nber.org/papers/w22425.pdf).
- Morgan K, Munday M, Roberts A. Local economic development opportunities from NHS spending: Evidence from Wales. Urban Studies. 2016; 54(13): 3138–56.
- Sacks J. The Money Trail: Measuring Your Impact on the Local Economy Using LM3. New Economics Foundation; 2002 (http://nefconsulting.com/wp-content/uploads/2017/05/TheMoneyTrail.pdf).
- Livingood WC, Coughlin S, Bowman W, Bryant T, Goldhagen J. Application of economic impact analysis to a local public health agency and its “academic health department”. Public Health Reports. 2007; 122(1): 27–36 (www.ncbi.nlm.nih.gov/pmc/articles/PMC1802120/).
- Devins D, Gold J, Boak G, Garvey R, Willis P. Maximising the Local Impact of Anchor Institutions: A Case Study of Leeds City Region. Joseph Rowntree Foundation; 2017 (www.jrf.org.uk/report/maximising-local-impact-anchor-institutions-case-study-leeds-city-region).
- NHS Business Services Authority. The Future Operating Model for NHS procurement: Transforming the landscape of NHS procurement. Department of Health; 2017 (www.nhsbsa.nhs.uk/sites/default/files/2017-06/FOM_general_guide_0.pdf).
- Department of Health. Operational Productivity and Performance in English NHS Acute Hospitals: Unwarranted Variations. Department of Health; 2016 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/499229/Operational_productivity_A.pdf).
- HM Government. Public Services (Social Value) Act 2012, Chapter 3. The Stationery Office; 2012 (www.legislation.gov.uk/ukpga/2012/3/pdfs/ukpga_20120003_en.pdf).
- Official Journal of the European Community. EU Procurement Thresholds [webpage]. Official Journal of the European Community (www.ojec.com/thresholds.aspx).
- HM Government. Procurement Reform (Scotland) Act 2014. The Stationery Office; 2014 (www.legislation.gov.uk/asp/2014/12/section/9).
- Welsh Government. Community Benefits: Delivering Maximum Value for the Welsh Pound – 2014. Welsh Government; 2014 ( https://gweddill.gov.wales/docs/dpsp/publications/valuewales/140904-community-benefit-report-en.pdf).
- GOV.UK. Big opportunities for small firms: government set to spend £1 in every £3 with small businesses. Cabinet Office; 2015 (www.gov.uk/government/news/big-opportunities-for-small-firms-government-set-to-spend-1-in-every-3-with-small-businesses).
- GOV.UK. The government buying standard for food and catering services. Department for Environment, Food and Rural Affairs; 2015 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/418072/gbs-food-catering-march2015.pdf).
- Cabinet Office. Social Value Act Review. Cabinet Office; 2015 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/403748/Social_Value_Act_review_report_150212.pdf).
- Redding D, Butler J. Healthy Commissioning – How the Social Value Act is being used by Clinical Commissioning Groups. National Voices; 2017 (www.nationalvoices.org.uk/sites/default/files/public/publications/healthy_commissioning_-_how_the_social_value_act_is_being_used_by_clinical_commissioning_groups.pdf).
- Stubbington T. Buy local, hire local: Preston blossoms on Corbynomics. The Sunday Times; 29 October 2017 (www.thetimes.co.uk/article/buy-local-hire-local-preston-blossoms-on-corbynomics-xkbtq0t90).
- What Works Centre for Local Economic Growth. Local Procurement [webpage]. What Works Centre for Local Economic Growth (https://whatworksgrowth.org/resources/local-procurement-1).
- Zuckerman D, Parker K. Hospitals Aligned for Healthy Communities: Inclusive, Local Sourcing. Democracy Collaborative; 2016 (https://democracycollaborative.org/content/hospitals-aligned-healthy-communities-inclusive-local-sourcing).
- Local Government Association. A Councillor’s Guide to Procurement. Local Government Association, Local Partnerships; 2013 (www.local.gov.uk/sites/default/files/documents/councillors-guide-procure-4b2.pdf).
- Manchester City Council. Social Value Toolkit for Suppliers. Manchester City Council; 2017 (https://secure.manchester.gov.uk/downloads/download/6648/social_value_toolkit).
- Social Value Wales. The Model [webpage]. Social Value Wales (http://socialvaluewales.co.uk/the-model).
- Department of Health. A Toolkit to Support the Development of a Hospital Food and Drink Strategy. Department of Health; 2016 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/499745/Toolkit_Feb_16.pdf).
- Department of Health. The Hospital Food Standards Panel’s Report on Standards for Food and Drink in NHS Hospitals. Department of Health; 2014 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/523049/Hospital_Food_Panel_May_2016.pdf).
- NHS England. NHS Standard Contract 2019/2020. Service Conditions (Full Length) version 2. NHS England (www.england.nhs.uk/wp-content/uploads/2019/03/3-FL-SCs-1920-sepsis.pdf).
- GOV.UK. New ‘Social Value’ contracts to revolutionise government procurement. Cabinet Office; 19 November 2018 (www.gov.uk/government/news/new-social-value-contracts-to-revolutionise-government-procurement).
- Health Select Committee. NHS Long-term Plan: legislative proposals. Chapter 2: Competition. HM Government; 2019 (https://publications.parliament.uk/pa/cm201719/cmselect/cmhealth/2000/200006.htm#_idTextAnchor020).
- The Scottish Government. Guidance under the Procurement Reform Act (Scotland) 2014. The Scottish Government; 2016 (www.gov.scot/binaries/content/documents/govscot/publications/advice-and-guidance/2016/03/guidance-under-procurement-reform-scotland-act-2014/documents/00496919-pdf/00496919-pdf/govscot:document/00496919.pdf).
- Department of Health. Compliance with Hospital Food Standards in the NHS. Two Years On: A Review of Progress since the Hospital Food Standards Panel Report in 2014. Department of Health; 2017 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/586490/HFSP_Report.pdf).
- Allcock C, Dormon F, Taunt R, Dixon J. Constructive Comfort: Accelerating Change in the NHS. The Health Foundation; 2015 (www.health.org.uk/sites/default/files/ConstructiveComfortAcceleratingChangeInTheNHS.pdf).
- Community Housing Cymru. A guide to the Community Benefits Measurement Tool Version 6.6 July 2014. Community Housing Cymru; 2014 (https://chcymru.org.uk/uploads/general/Value_Wales_guidance.pdf).
- NHS Salford Clinical Commissioning Group. Social Value Strategy 2019-2021. NHS Salford Clinical Commissioning Group; 2019 (https://extranet.salfordccg.nhs.uk/application/files/4815/5618/2744/Social_Value_Strategy.pdf).
- Salford Social Value Alliance. Social Value Toolkit. Useful Resources. Social Value in Salford (www.salfordsocialvalue.org.uk/social-value-toolkit/useful-resources).
- Salford City Council. Social Impact Report 2018: One year on. Salford City Council; 2018 (www.salford.gov.uk/media/393544/social-impact-report-2018.pdf).
- Jones B, Horton T, Warburton W. The Improvement Journey. Why Organisation-Wide Improvement in Health Care Matters, and How to Get Started. The Health Foundation; 2019 (www.health.org.uk/sites/default/files/upload/publications/2019/The%20improvement%20journey.pdf).
- Sustainable Development Unit. Creating social value. SDU (www.sduhealth.org.uk/areas-of-focus/social-value.aspx).
- Social Enterprise UK. The Social Value Guide. Implementing the Public Service (Social Value) Act. Social Enterprise UK; 2012 (www.socialenterprise.org.uk/Handlers/Download.ashx?IDMF=2e2c2f33-30d6-4ad5-a08c-e5221821c8d5).
- NHS Digital. Estates returns information collection, England, 2017–18. NHS Digital; 2018 (https://digital.nhs.uk/data-and-information/publications/statistical/estates-returns-information-collection/summary-page-and-dataset-for-eric-2017-18).
- Hoffimann E, Barros H, Ribeiro AI. Socioeconomic inequalities in green space quality and accessibility: Evidence from a southern European city. International Journal of Environmental Research and Public Health. 2017; 14(8): 916.
- The Health Foundation. Infographic: How Does Housing Influence our Health? The Health Foundation; 2017 (www.health.org.uk/infographic/how-does-housing-influence-our-health).
- Nocol S, Roys M, Garrett H. The Cost of Poor Housing to the NHS. Building Research Establishment; 2011 (www.bre.co.uk/filelibrary/pdf/87741-Cost-of-Poor-Housing-Briefing-Paper-v3.pdf).
- Communities Connected Consultancy Ltd and Social Care Wales. Approaches to Community Resilience. Social Care Wales; 2018 (https://socialcare.wales/resources/approaches-to-community-resilience-communities-connected-consultancy-ltd).
- Houses of Parliament Parliamentary Office of Science and Technology. Green Space and Health. Houses of Parliament; 2016 (http://researchbriefings.files.parliament.uk/documents/POST-PN-0538/POST-PN-0538.pdf).
- The Health Foundation. New short-term capital funding boost for NHS in England will only scratch the surface. The Health Foundation; 2019 (www.health.org.uk/news-and-comment/news/New-short-term-capital-funding-boost-for-NHS-will-only-scratch-surface).
- Kraindler J, Gershlick B, Charlesworth A. Failing to Capitalise: Capital Spending in the NHS. Briefing. The Health Foundation; 2019 (www.health.org.uk/sites/default/files/upload/publications/2019/Failing-to-capitalise.pdf).
- Naylor R. NHS Property and Estates: Why the Estate Matters for Patients. Department of Health; 2017 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/607725/Naylor_review.pdf).
- National Housing Federation. Surplus NHS Land: A Best Value Alternative. Connecting Housing and Health Briefing. National Housing Federation; 2015 (http://s3-eu-west-1.amazonaws.com/pub.housing.org.uk/Surplus_NHS_land_-_a_best_value_alternative_briefing.pdf).
- Ministry of Housing, Communities and Local Government. Public Land for Housing Programme 2015 –2020. Programme Handbook for Departments and Arm’s Length Bodies. August 2018: Update. Ministry of Housing, Communities and Local Government; 2018 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/734654/Public_Land_for_Housing_Programme_2015-20.pdf).
- NHS Digital. NHS Surplus Land 2018/19 England [PAS]. NHS Digital; 2019 (https://digital.nhs.uk/data-and-information/publications/statistical/nhs-surplus-land/2018-19-england-pas).
- NHS Providers. There For Us: A Better Future for the NHS Workforce. NHS Providers; 2017 (https://nhsproviders.org/media/3901/there-for-us-a-better-future-for-the-nhs-workforce.pdf).
- Appleby, J. Making Sense of PFI. Nuffield Trust Explainer. Nuffield Trust; 2017 (www.nuffieldtrust.org.uk/resource/making-sense-of-pfi).
- NHS Property Services. Sale of surplus London hospital site yields new homes and funds for reinvestment in the NHS. NHS Property Services (www.property.nhs.uk/news-insight/news/sale-of-surplus-london-hospital-site-yields-new-homes-and-funds-for-reinvestment-in-the-nhs).
- Wheatley H. Still No Homes for Nurses: How NHS Land Is Being Sold Off To Build Unaffordable Homes. New Economics Foundation; 2019 (https://neweconomics.org/uploads/files/StillNoHomes_May2019.pdf).
- New Economics Foundation. Four out of five homes built on NHS land are unaffordable to nurses. New Economics Foundation; 2018 (https://neweconomics.org/2018/01/four-five-homes-built-nhs-land-unaffordable-nurses).
- National Housing Federation. Releasing NHS Estates For Community Benefit. Connecting Housing and Health Briefing. National Housing Federation (www.housinglin.org.uk/_assets/Resources/Housing/OtherOrganisation/NHF_Releasing_NHS_Estates_Briefing_v3_002.pdf).
- Chevin D. Housing Associations and the NHS: New Thinking, New Partnerships. The Smith Institute; 2015 (www.smith-institute.org.uk/wp-content/uploads/2015/09/Housing-associations-and-the-NHS.pdf).
- NHS England. Healthy By Design: The Healthy New Towns Network Prospectus. NHS England; 2018 (www.england.nhs.uk/wp-content/uploads/2018/01/healthy-by-design-healthy-new-towns-network-prospectus.pdf).
- The King’s Fund. Putting Health into Place: Introducing NHS England’s Healthy New Towns Programme. The King’s Fund; 2019 (www.kingsfund.org.uk/sites/default/files/2018-09/putting-health-into-place-nhs-england.pdf).
- Sustainable Development Unit. Health and care system (HCS) carbon footprint [webpage]. SDU (www.sduhealth.org.uk/policy-strategy/reporting/hcs-carbon-footprint.aspx).
- Sustainable Development Unit. Reducing the Use of Natural Resources in Health and Social Care. SDU; 2018 (www.sduhealth.org.uk/documents/Policy%20and%20strategy/20180912_Health_and_Social_Care_NRF_web.pdf).
- Watts N Amann M, Arnell N, Ayeb-Karlsson S, Belesova K, Berry H, et al. The 2018 report of the Lancet Countdown on health and climate change: shaping the health of nations for centuries to come. The Lancet. 2018; 392(10163): 2479–2514 (www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)32594-7/fulltext).
- Public Health England. Estimation of Costs to the NHS and Social Care Due to the Health Impacts of Air Pollution. Public Health England; 2018 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/708854/Estimation_of_costs_to_the_NHS_and_social_care_due_to_the_health_impacts_of_air_pollution.pdf).
- Royal College of Physicians. Every breath we take: the lifelong impact of air pollution. Royal College of Physicians; 2016 (www.rcplondon.ac.uk/projects/outputs/every-breath-we-take-lifelong-impact-air-pollution).
- The British Lung Foundation. Toxic Air at the door of the NHS. The British Lung Foundation; 2018 (www.blf.org.uk/take-action/campaign/nhs-toxic-air-report).
- Ebi K, Campbell-Lendrum D, Wyns A. The 1.5 Health Report – Synthesis on Health and Climate Science in the IPCC SR1.5. World Health Organization; 2018 (www.who.int/globalchange/181008_the_1_5_healthreport.pdf).
- World Health Organization. Environmental Health Inequalities in Europe. Second Assessment Report. WHO Regional Office for Europe; 2019 (www.euro.who.int/en/publications/abstracts/environmental-health-inequalities-in-europe.-second-assessment-report-2019).
- Clougherty JE, Kubzansky LD. A framework for examining social stress and susceptibility to air pollution in respiratory health. Environmental Health Perspectives. 2009; 117(9): 1351–8.
- Paavola J. Health impacts of climate change and health and social inequalities in the UK. Environmental Health. 2017; 16(Suppl 1): 113.
- Islam S, Winkle J. Climate Change and Social Inequality. UNDESA Working Paper No. 152. United Nations Department of Economic and Social Affairs; 2017 (www.un.org/esa/desa/papers/2017/wp152_2017.pdf).
- HM Government. Climate Change Act 2008. The Stationery Office; 2008 (www.legislation.gov.uk/ukpga/2008/27/part/1/crossheading/the-target-for-2050).
- HM Government. The Climate Change Act 2008 (2050 Target Amendment) Order 2019. The Stationary Office; 2019 (www.legislation.gov.uk/uksi/2019/1056/contents/made).
- NHS England. 2019/20 NHS Standard Contract. NHS England; 2019 (www.england.nhs.uk/nhs-standard-contract/19-20).
- Birch E, Perry DC, Taylor Jr HL. Universities as anchor institutions. Journal of Higher Education Outreach and Engagement. 2013; 17(3): 9 (http://openjournals.libs.uga.edu/index.php/jheoe/article/viewFile/1035/680).
- Sustainable Development Unit. Sustainable Healthcare Dashboard to support key Long Term Plan targets. SDU; 2019 (www.sduhealth.org.uk/news/670/sustainable-healthcare-dashboard-to-support-key-long-term-plan-targets).
- Naylor C, Appleby J. Sustainable Health and Social Care: Connecting Environmental and Financial Performance. The King’s Fund; 2012 (www.kingsfund.org.uk/sites/default/files/field/field_publication_file/sustainable-health-social-care-appleby-naylor-mar2012.pdf).
- Global Action Plan. Clean Air Hospital Framework. Global Action Plan; 2019 (https://globalactionplan.org.uk/files/clean_air_hospital_framework.pdf).
- Sustainable Development Unit. Health Outcomes of Travel Tool - V 3.0. SDU; 2019 (www.sduhealth.org.uk/delivery/measure/health-outcomes-travel-tool.aspx).
- Southern Staffordshire Community Energy, University Hospitals of North Midlands. Beat the Cold. Share Offer Document July 2016: Saving Lives with Solar. Southern Staffordshire Community Energy; 2016 (www.ethex.org.uk/medialibrary/2016/07/21/3e7e443a/SSCEUHNMShareOfferDocumentFinal.pdf).
- Lucas K, Tyler S, Christodoulou G. The Benefits of Providing New Public Transport in Deprived Areas. Joseph Rowntree Foundation; 2008 (www.jrf.org.uk/report/benefits-providing-new-public-transport-deprived-areas).
- Sustainable Development Unit. Reducing the use of natural resources in health and social care: 2018 report (Natural Resource Footprint). Sustainable Development Unit; 2018 (www.sduhealth.org.uk/policy-strategy/reporting/natural-resource-footprint-2018.aspx).
- Greater Manchester Health and Social Care Partnership. The Greater Manchester Population Health Plan 2017–2021. Greater Manchester Health and Social Care Partnership; 2017 (www.gmhsc.org.uk/wp-content/uploads/2018/05/Population-Health-Plan-2017-2021.pdf).
- Campbell F. Nobody Left Behind: Maximising the Health Benefits of an Inclusive Local Economy. Local Government Association; 2018 (www.local.gov.uk/sites/default/files/documents/22.15%20inclusive%20growth_04.1.pdf).
- GOV.UK. The UK’s Industrial Strategy [webpage]. GOV.UK (www.gov.uk/government/topical-events/the-uks-industrial-strategy).
- Marlow D. Getting to know your local economic leadership is a valuable health investment [webpage]. NHS Confederation; 2015 (www.nhsconfed.org/blog/2015/03/getting-to-know-local-economic-leadership-valuable-investment).
- NHS Confederation. Health In All Local Industrial Strategies? NHS Confederation; 2019 (www.nhsconfed.org/-/media/Confederation/Files/Publications/Documents/Health-in-all-local-industrial-strategies.pdf).
- Sheffield City Partnership. Working Together to Build a Sheffield that Works for Everyone: A Partnership Framework For An Inclusive and Sustainable Economy. Sheffield City Partnership; 2018 (www.sheffieldcitypartnership.org/s/Partnership-Framework.pdf).
- Harrison D, Edwards P. Making Procurement Work for All: Procurement Practices as a Route to Fulfilling Work in North East England. Institute for Local Governance; 2018 (https://d1ssu070pg2v9i.cloudfront.net/pex/carnegie_uk_trust/2018/11/07120730/Making-Procurement-Work-for-All.pdf).
- Porter J, Fisher-Burns D, Ha Pham B. Anchor Collaboratives: Building Bridges With Place-Based Partnerships and Anchor Institutions. The Democracy Collaborative; 2019 (https://democracycollaborative.org/content/anchor-collaboratives-building-bridges-place-based-partnerships-and-anchor-institutions).
- Kershaw M, McKenna H, Charles A, Ewbank L, Ham C. Sustainability and Transformation Partnerships in London: An Independent Review. The King’s Fund; 2018 (www.kingsfund.org.uk/publications/sustainability-transformation-partnerships-london).
- Walshe K, Lorne C, Coleman A, McDonald R, Turner A. Devolving Health and Social Care: Learning from Greater Manchester. The University of Manchester; 2018 (www.mbs.ac.uk/media/ambs/content-assets/documents/news/devolving-health-and-social-care-learning-from-greater-manchester.pdf).
- Leeds City Council, West Yorkshire Combined Authority, Joseph Rowntree Foundation. Harnessing the Power of Anchor Institutions – A Progressive Framework. Joseph Rowntree Foundation (https://democracy.leeds.gov.uk/documents/s181576/4%20Anchor%20Institution%20Progression%20Framework%20Toolkit.pdf).
- Centre for Local Economic Strategies and Preston City Council. How we built community wealth in Preston. CLES; 2019 (https://cles.org.uk/publications/how-we-built-community-wealth-in-preston-achievements-and-lessons/).
- Live healthy Live happy Partnership Birmingham and Solihull. Live Healthy, Live Happy Birmingham and Solihull Draft STP (Sustainability and Transformation) Strategy. Birmingham and Solihull STP; 2018 (https://governance.wmca.org.uk/documents/s1785/04.%20Wellbeing%20Board%20PROOF_v7_BSol_STP_Strategy_May_2018.pdf).
- Intelligence and Policy Service, Leeds City Council. Leeds Observatory [website]. Leeds City Council (https://observatory.leeds.gov.uk).
- Centre for Local Economic Strategies. Local Wealth Building in Birmingham and Beyond: A New Economic Mainstream. CLES; 2018 (https://cles.org.uk/wp-content/uploads/2018/07/Local-Wealth-Building-in-Birmingham-and-Beyond_report_2018.pdf).
- Centre for Local Economic Strategies. Birmingham anchor network gets underway. CLES; 2019 (https://cles.org.uk/news/birmingham-anchor-network/).
- Randall S. Leading Networks in Healthcare: Learning About What Works – The Theory and the Practice. The Health Foundation; 2013 (www.health.org.uk/sites/default/files/LeadingNetworksInHealthcare.pdf).
- NHS Confederation. Local Growth Academy [webpage]. NHS Confederation; 2017 (www.nhsconfed.org/localgrowthacademy).
- Healthcare Anchor Network. About the Healthcare Anchor Network [webpage]. Healthcare Anchor Network; 2019 (www.healthcareanchor.network/about.html).
- Brabner R. Leading universities pledge commitment to local communities. Civic University Commission; 2019 (https://upp-foundation.org/leading-universities-pledge-commitment-to-local-communities).
- National Housing Federation. Great Places Commission Interim Report. National Housing Federation (https://greatplaces.housing.org.uk/take-part/interim-report).
- Inquiry into the Civic Role of Arts Organisations. Principles of an arts organisation playing a civic role [webpage]. Inquiry into the Civic Role of Arts Organisations (http://civicroleartsinquiry.gulbenkian.org.uk/principles).