Foreword
To those interested in policy who aren’t long in the tooth, the word ‘Wanless’ may not mean much. But it should. Named after its chair, Derek Wanless, it was a landmark review of NHS funding, published nearly two decades ago in 2002.
Why is such an old review so important to revisit? Wanless was the first serious attempt to assess objectively the long-term funding needs of the NHS. It unlocked not only unique levels of growth in funding for the NHS, but also helped justify the tax rises to pay for it. And since policymaking is mostly about human behaviour, Nick Timmins exposes how politics ‘acutely intersects’ with the issue of NHS funding to wrestle progress out of conflict (although Nick uses more vivid language). As we exit from the pandemic, these issues are even more important to understand than they were in 2002.
Three surprises
If you think of the UK NHS as one ‘industry’, it is the largest in Europe. Now in its seventies, it is also one of Europe’s oldest. Polls consistently show the NHS is a national treasure in the public’s mind, top of the list of reasons they are proud to be British, and tops priorities for extra public funding. Not surprising then that the NHS successfully extracts extra funds from the Treasury each year, to a greater extent than most other areas of the public sector. But three things are surprising.
First, for such a national treasure, the year-on-year funding growth over the years has varied wildly – from 11% to -1% – making anything other than short-term planning a challenge. This matters in a service where demand for care only grows and can’t be suddenly turned off: more staff are constantly needed who take many years to train, the public expects new technologies it sees elsewhere in life, and clinical staff know that new technologies are being used to good effect in other countries, all of which need investment.
Second, other European countries have managed to invest more in health care over time – the Wanless review calculated even between 1972 and 1988 this totalled £220bn–£277bn relative to the EU average. Whatever the public and political importance of the NHS over time, paradoxically this has translated into chronic underinvestment. By 2002, this showed in a raft of unflattering international comparisons on performance, most visible in long waiting times for planned care, and winter crises in A&E.
Third, until the Wanless review in 2002, there had not been a full, objective, and published analysis of the demand pressures on the NHS under various scenarios for the long term, costed out, for the government or by the NHS itself. Wanless was a serious attempt to do that, in part made technically possible because data were increasingly available to analyse. Data, and modelling techniques, are much more sophisticated now, and yet even today there is no regular Wanless exercise for the NHS akin to the long-range projections for the economy by the Office for Budget Responsibility.
Clues as to why can be gleaned from Nick’s rollicking account of the politics surrounding the conception, delivery, and outcome of the Wanless review. For sure, by 2000, recognition was overripe that the NHS needed a major slug of investment, and not only over the short term. This wasn’t just politically needed in New Labour’s first term, off the back of a decade of the NHS being ‘under attack’ by market-based ideology following introduction of the 1991 NHS reforms, and inadequate funding growth. But also because cracks in the NHS were showing, not least with ‘never never’ waiting lists, winter crises and, of course, heart-rending individual cases of lapses in care in the late1990s as Nick documents – all translated into damning headlines.
Contested origins
Absent any substantive projections as to the funding needs, in January 2000 the PM announced the European Union average (health spending as a percentage of GDP) as the target for NHS spending by 2005. The Wanless review was then commissioned by the Treasury, examining resourcing the NHS and social care, and published as Securing our future health in 2002.
Whether or not the Wanless review came about to give retrospective credibility to the PM’s target, or to give advantage in a feud between Number 10 and the Treasury, its objectivity based on evidence made the case for a substantial increase in funding, further reform and justified increased taxes to pay for it. For 5 years following Wanless, the NHS was awarded well over twice the long-run average in real-terms growth in funding. Social care received a significant boost in funding for 3 years. National insurance was raised by 1%, and this tax rise was tolerable electorally. And a day after Wanless reported, Alan Milburn (then secretary of state for health), announced not only increases in staffing and equipment, but a significant set of reforms, in part centred on reducing waiting times.
As Nick Macpherson notes, the Wanless review, ‘… led to the only serious, non-forced, discretionary tax rise since at least 1979 – and one that proved electorally appealing’. And in Ed Balls’s words, ‘When I think back on reviews I have been involved in, and I have been involved in some really good ones over the years, the Wanless review is by far the most politically significant with the longest lasting effects.’
‘Doing a Wanless’
Which still leaves the surprise that ‘doing a Wanless’ is not a regular feature of planning today. To help, in 2020 the Health Foundation launched the REAL Centre (Research and Economic Analysis for the Long Term) to provide objective projections of supply and demand, and funds needed for the NHS under different scenarios. Unlike Wanless, REAL gives full consideration of social care funding as well. And neatly, the Director of the REAL Centre, Anita Charlesworth, was the senior official at the Treasury who led the secretariat supporting Derek Wanless two decades ago.
As the UK exits the pandemic, it faces not only the backlog of unmet demand for NHS care, unreformed social care, and investment sorely needed elsewhere in the public sector. For long waiting times and winter crises not to be the norm, the political pressure for more investment in the NHS will be intense. The large debt overhang from the pandemic, and justifiable demands for investment elsewhere, will mean competition for resources will be acute as will the pressure to raise taxes.
Perhaps time then to consider another Wanless? Waiting times for elective care had steadily increased before the pandemic, and the NHS faced 100,000 in staff shortages. The pandemic has further exposed the NHS’s Achilles heel – a fundamental lack of capacity. This was also on full view with respect to shortages in staff and equipment in social care. Any review should examine not just the capacity the NHS needs to address the backlog of care, but also unmet need and inequality in access for the NHS and social care. Both are needed to build care that is more resilient to future health shocks, as COVID-19 is sadly unlikely to be the last. Such a review might give more objective credibility to assessments of how much funding is needed for care over the next 5 years; and justify that to the public, to politicians and the Treasury, especially if tax rises are on the cards.
For the NHS this time round though there is already a clear reform agenda, in the form of the NHS Long Term Plan, which commands widespread support. It will be more difficult to justify the case for further significant reform. It is the pandemic that has caused the backlog, public perceptions of how the NHS has managed the crisis and vaccine rollout, and the obvious staff commitment to duty, are favourable. And the last round of reform was costly, distracting, and of questionable impact. Instead extra resource may be better targeted directly at more basic issues that will limit progress on waiting and wider performance – such as staff shortages, insufficient technology and other equipment
For social care, the task is larger as there is currently no reform strategy, there is an urgent need for investment, and outside of a pandemic there are few screaming headlines to prompt action. It is here that political leadership, deal-making and creativity, of the sort Nick notes in this study, is sorely needed most to ‘fix social care once and for all’.
Dr Jennifer Dixon CBE
Chief Executive,
The Health Foundation
Introduction and origins
Introduction
It is almost 20 years since the Wanless report on the future funding of the NHS. As its 20th anniversary approaches, this study revisits the original – Securing our future health. It examines the origins of the Wanless review and takes something of an outline look at its methodology. It also attempts an assessment of its impact, in both the short and the long term.
The review is, however, a contested event, both in terms of its origins and its impact.
To some it is one of the most important documents in the history of the NHS, providing the massive boost in funding that hugely improved both the quality of services and access to them across the 2000s. Indeed, in some people’s eyes, it fundamentally changed the political argument over the NHS.
To others it was merely a ‘His Master’s Voice’ report, commissioned by Gordon Brown, then Chancellor, to deliver a predetermined outcome. A report to help justify what Tony Blair, the Prime Minister, had already made inevitable – a big increase in expenditure, and the associated tax rise to pay for that.
Some believe the report’s impact has been lasting. Others that rereading it is a somewhat depressing exercise. It is almost as if nothing has changed in the sense that some of its big themes – much improved health IT, far better workforce planning, better integrated care, a proper social care settlement – are still current and immensely pressing matters.
This study examines these and other issues, taking in the subsequent Wanless review of public health, while asking whether, if a government were to repeat such an exercise, there might be a way to amplify its impact.
It is important to note, however, that the government papers for this period are not yet available. So while there are plenty of references to published material, some of what is related here relies on memory, including that of the author. And honestly held memories can play tricks.
It is also worth underlining that this study does not seek to tell a full story of the management of the NHS, either at the time of Wanless or afterwards. The author has attempted that elsewhere. Some of the key events are, however, outlined because they are part of the context and helped shape the impact of the review (see also Box 1). But they are not a full account. The focus here is on the review itself.
We start with its origins … where there is more than one view of precisely how it came about.
Box 1: Timeline of the Wanless reviews and selected linked events
- May 1997: Labour landslide. Tony Blair declares at the end of the campaign, ‘We have 24 hours to save the NHS.’
- Late 1999: Gordon Brown, then Chancellor, and two key advisers, Ed Balls and Ed Miliband, devise a strategy for a long-term settlement for the NHS and the tax rise needed to deliver that. This strategy appears, however, either not to have been communicated to, or not understood by, Number 10.
- January 2000: After a winter crisis in the NHS, the Prime Minister, Tony Blair, announces on the BBC’s Breakfast with Frost that all things being equal, Labour will increase NHS spending up to the European Union average.
- March 2000: The Budget provides significant real-terms increases in NHS and social care spending, as Brown also announces he is commissioning ‘a long-term assessment of the technological, demographic and medical trends over the next two decades that will affect the health service… ’ This will become the Wanless review.
- July 2000: Following the spending rise, the NHS Plan is published, producing the first waiting time targets and the promise of more staff, more buildings and a more responsive service.
- January 2001: Anita Charlesworth appointed as the Treasury lead, with Derek Wanless subsequently recruited to head the review.
- March 2001: Wanless’s appointment is announced in the Budget.
- November 2001: Interim Wanless report.
- April 2002: Final Wanless report – Securing our future health: Taking a long-term view. Spending commitment made and national insurance increase announced. The day after, Delivering the NHS Plan announces the introduction of more market-like mechanisms into the NHS.
- April 2003: Wanless asked to conduct a follow-up review on public health.
- February 2004: Securing good health for the whole population – the public health report – published.
A more detailed timeline of NHS policies can be found at The Health Foundation’s Policy Navigator (http://navigator.health.org.uk) and at the Nuffield Trust’s NHS Reform Timeline (www.nuffieldtrust.org.uk/health-and-social-care-explained/nhs-reform-timeline).
Origins version one: ‘The most expensive breakfast in history’
On Sunday 16 January 2000, in what rapidly became dubbed ‘the most expensive breakfast in history’, the Prime Minister, Tony Blair, went on to the BBC’s flagship weekend political programme Breakfast with Frost. Pretty much out of the blue, Blair declared that all things being equal, the UK would increase its health spending up to the European Union average by 2005.
The commitment was enormous. Roughly 2 percentage points of GDP. And next to no one knew it was coming. Not his Chancellor, Gordon Brown, who reportedly exploded at Blair, ‘You’ve stolen my fucking budget.’ Not, in any detail, his health secretary Alan Milburn. Nor Alan Langlands, then chief executive of the NHS. Simon Stevens, Milburn’s health adviser and a future chief executive of the NHS, learned about it via a pager message while visiting a Homebase store.
Journalists like me were stunned, scrabbling to work out just what this huge commitment would cost – not least because the EU average was likely to increase over the next 5 years. It was not that different in Number 10. Robert Hill, Blair’s health adviser, put in an urgent call from his home to that of Clive Smee, the health department’s chief economist, asking him to set out precisely how much this would cost and whether it even looked achievable given reasonable assumptions around economic growth.
On a Sunday morning, outside the Treasury, Smee was the only one likely to have to hand the most up-to-date EU expenditure data on which to do the numbers. In typically self-deprecating style, in his memoir Smee recalled that most of the more complicated calculations were done by his daughter’s boyfriend because he was the only one who knew how to use the compound interest function on his calculator. The results of these calculations, which concluded that on reasonable assumptions it was in fact doable, were put out late in the day in a press release.
Over the next couple of days, Gordon Brown sought to water down Blair’s declaration from what was plainly a commitment to ‘an aspiration’. But the Prime Minister, who went on to reinforce his message at Prime Minister’s Questions, had spoken. The die had been cast. And in the March Budget, the Chancellor duly delivered the first steps on that road. He pre-empted the longer term Spending Review planned for July by announcing spending increases averaging 6.1% a year in real terms over the following 3 financial years – easily the largest ever sustained rise in NHS expenditure. The average since 1948 had been 3.3%.
These increases were historically large. But they were not on their own sufficient to raise health spending to the EU average by 2005. In the same Budget, however, Brown also announced that he was ‘commissioning a long-term assessment of the technological, demographic and medical trends over the next two decades that will affect the health service’. The review was to report to him ‘in time for the start of the next Spending Review in 2002’.
This review did not yet have a chair, nor a title. But Securing our future health, as it would become, proved to be the first serious attempt by any government in the history of the NHS to have an independent assessment made of the service’s likely future needs, and likely cost, over the next 20 years.
That account is not just the received wisdom of how the Wanless review emerged. It is the view of many of the key players involved in health financing and policy at the time, who were interviewed for this study. There is, however, another – though not incompatible – version of its origin. One that sets it in a somewhat wider context, and to which we will come (see Origins version two).
The road to Breakfast with Frost
This account opened with the statement that Blair’s announcement came ‘pretty much out of the blue’. But that is not entirely so. In fact, it had a lengthy back story. At the end of the 1990s, the NHS was in a pretty parlous state. And it is easy to forget now the extent to which the NHS model – of a tax-funded, largely free-at-the-point-of-use, and pretty comprehensive service – was itself under fire from the mid-1990s into the 2000s.
The policy and politics of the 1990s
In 1991, amid immense controversy, the Conservatives had introduced the so-called and somewhat misnamed ‘internal market’ – otherwise known as the purchaser/provider split. The ‘providers’ were NHS hospitals. These were turned into less directly managed, and somewhat more businesslike, NHS trusts. The trusts competed for patients through contracts from NHS ‘purchasers’. The ‘purchasers’ were the then health authorities and so-called GP fundholders – those GPs who volunteered to take budgets with which to buy care on their patients’ behalf. The private sector was also free to compete for these contracts, although initially that happened on a very small scale.
Many, not just on the far left, suspected that this more market-like approach, and in particular the somewhat more businesslike way of running NHS hospitals, was merely the first step towards privatising them. Furthermore, after a huge injection of cash in 1991 to make sure the new ‘internal market’ did not crash and burn on day one, money for the NHS had become increasingly tight over the 1990s. To the point that in 1996/97, the year running up to the 1997 general election, NHS spending had actually been cut in real terms for the first time since the early 1950s.
For all the diminishing amounts of growth, John Major, the Prime Minister of the day, and his successive health secretaries Virginia Bottomley and Stephen Dorrell, all supported the NHS model. As did Ken Clarke, Chancellor for most of this period, and himself the former health secretary whose white paper Working for patients had introduced the purchaser/provider split. Indeed Clarke, when asked whether he had private medical insurance, had once produced the disarming declension, ‘I don’t have it. You don’t need it. We have the National Health Service.’ But Major’s government was beleaguered throughout by the ‘No Turning Back’ group of Conservative MPs, the guardians of what they saw as the Thatcherite flame. Both they and right-wing think tanks such as the Institute for Economic Affairs and the Adam Smith Institute were, over this period, propounding various models of health care that would have diminished or removed the tax-funded, free-at-the-point-of-use nature of the NHS.
The mix of a more market-like way of managing the service through the purchaser/provider split, suspicion of where the government was taking the NHS, and ever-tightening resources saw not just the usual suspects but mainstream figures in the world of health care start to wonder whether the NHS model was, in fact, sustainable.
In September 1995, Rodney Walker, the retiring chairman of the NHS Trust Federation which at the time represented most NHS trusts, argued that rising demand, medical advances and an ageing population meant the NHS would have to be reduced to ‘a safety net’ for the old and vulnerable. Walker was a highly enthusiastic advocate for the government’s more market-like approach to running the service. Even so, his stance came as a bit of a shock.
But later the same month, a study funded by the pharmaceutical industry to the tune of £100,000 concluded that the gap between demand and resources could not be closed by taxation alone, and that user charges and ‘a clearer definition of what services will be provided free at the point of use’ were likely to be needed. It painted several not very appealing scenarios of what that might involve.
Given its funding source, that conclusion was perhaps not surprising. What was surprising was that the review was chaired by Sir Duncan Nichol, the chief executive of the NHS at the time of the 1991 reforms, and who in 1994 had shocked some by joining the board of Bupa, Britain’s biggest private health insurer, as soon as the civil service rules allowed him to do so. Leading figures on the review included Chris Ham, a Professor of Health Services Management at the University of Birmingham and a future chief executive of The King’s Fund health think tank, while its deputy chair was Patricia Hewitt, formerly press spokesperson for the Labour leader Neil Kinnock in the 1980s and who, a decade after the report, would herself be health secretary. These mainstream figures were seriously questioning whether the NHS could go on as it was – and they were not alone.
Then, in 1996, less than a year before the 1997 general election, a group of influential figures formed the Rationing Agenda Group, partly funded by The King’s Fund, and whose members included distinguished health economists, GPs, consultants and other health care luminaries, none of whom would normally be regarded as being anywhere near the far right of politics. Its conclusion was that ‘rationing in health care is inevitable’ and that the public needed to be involved in the debate about how that was to be done. Public satisfaction with the NHS had been on a downward trend in the years after 1993, to the point where according to the British Social Attitudes Survey, almost 50% were dissatisfied with it and only just over 30% were satisfied.
At one point in the midst of this Alan Langlands, the chief executive of the NHS, felt the need to go on the record to attack these ‘doom and gloom’ merchants, declaring that he wanted to distance himself from the ‘ration and privatise brigade’. The climate was such that A service with ambitions, a white paper produced by the then Conservative health secretary Stephen Dorrell, equally felt the need to open with a lengthy defence of the tax-funded nature of the NHS, arguing that the model was in fact sustainable.
In summary, during the middle of the 1990s and beyond, the NHS model was not just under attack from those who had never believed in it, but was being questioned by some who would otherwise have been seen as its natural supporters. The argument became less heated after Labour won the 1997 general election. But for reasons we shall see, Labour’s first 2 and a half years in power had not laid it to rest.
Conservative policy in early 2000
At the time of Breakfast with Frost, Conservative health policy under William Hague as leader, and Dr Liam Fox as health spokesperson, was both to promise the NHS real-terms increases – although at unspecified scale – but also to provide tax breaks for private health insurance. On the morning of Breakfast with Frost, Fox was quoted in the Sunday Times as saying that ‘philosophically’ the Conservatives had ‘moved on’ from a fully comprehensive NHS, and that ‘insurance companies could cover conditions that are not high-tech or expensive, like hip and knee replacements and hernia and cataract operations.’ The aim, the Conservatives argued, being to increase health spending overall while having a larger private sector to reduce demand on the NHS. In other words, at the time of the famous breakfast, the NHS model was still under attack from the leadership of the UK’s main opposition party.
Labour’s record before the breakfast
Alongside this ideological assault sat Labour’s record since Tony Blair’s declaration ‘We have 24 hours to save the NHS,’ made on the eve of the 1997 poll that delivered his landslide. Once in power, Labour had repeatedly talked the language not just of improvement but of public sector ‘transformation’. But in its manifesto it had also promised to stick with the spending plans of its Conservative predecessor for its first 2 years. When these plans were announced, just ahead of the election, they were so tight that Andrew Dilnot, the director of the Institute for Fiscal Studies, suggested that Ken Clarke was ‘having a little joke’ at Labour’s expense.
The result was that money for public services, including the NHS, was seriously constrained. Thanks in part to the social security budget for once coming in some £2bn below forecast, Labour’s first big Spending Review in 1998 did deliver growth averaging 4.7% in real terms for the succeeding 3 years: above the long run average of just over 3%. Those increases, however, only started to flow in April 1999, a mere 9 months before the Breakfast with Frost. Furthermore, much of it was earmarked for centrally determined initiatives that were already under way – for example, the first walk-in centres, the creation of NHS Direct (now NHS 111), some refurbishment of A&E departments, cleaner wards, and the rebranding of the NHS so that it has a consistent logo. All but the last of these were intended to make the NHS more consumer friendly and accessible, while reducing the pressure on accident and emergency departments. But the result was the day-in-day-out services of the NHS, those in the GP’s surgery and on the wards, were still seen by clinicians to be under enormous pressure. Waiting lists were rising rather than falling – the money being so tight that Labour had had to translate an election promise to cut them by 100,000 into one that would be achieved not rapidly, but over the life of the parliament.
Back then much less data were available on NHS performance. But the state of the service can be illustrated by one reputable estimate that up to 500 cardiac patients a year were dying from their condition while on the waiting list. Over the 1990s, nurse numbers had fallen by 40,000 – a 10% reduction. In early 2000, more than 130,000 patients were waiting more than 6 months for an outpatient appointment once they had been referred by their GP. At this stage, the NHS did not even count the subsequent wait for diagnostic procedures – the scans, X-rays and tests that might well be needed at an outpatient appointment before definitive treatment was decided on.
At their worst, such waits could run to months. And once past that stage, with the patient on the inpatient list for definitive treatment, almost 70,000 were waiting more than a year. The result was that some patients were waiting more than 2 years from GP referral to treatment although the NHS had no real idea of how many, other than it was clearly many thousands, and – more likely – many, many thousands. As polling for the NHS Plan was later to underline, waiting times were the public’s number one concern about the service.
Furthermore, at the end of the 1990s, the first data on the outcomes of care internationally started to become available. On certain key aspects, these showed that the NHS was not doing well. Back in 1994 the Organisation for Economic Cooperation and Development (OECD) in one of its regular economic surveys had judged the NHS to be ‘a remarkably cost-effective institution.’ It had, since the later 1960s, spent appreciably below the EU and OECD average. By 2000, however, as the new information on outcomes became available, the OECD sharply changed its tune. It highlighted poor cancer survival rates. It suggested that other outcomes – for example for heart disease and diabetes – did not look good. It noted the apparent underinvestment in doctors and buildings. It added in the long waiting times and concluded that the NHS was probably underfunded.,,
Since its foundation, the NHS has always had a tendency to have ‘winter crises’, as do many other health care systems. But the winter of 1998/99 proved a really tough one, and in summer 1999, at its annual conference, the British Medical Association (BMA) launched a stinging attack on the government’s health priorities and its management of the service. The charge was that the government was indulging in spin over substance and had distorted priorities by rebranding the NHS and creating walk-in centres rather than getting money onto the wards and into GP surgeries. That contributed 2 days later to Blair’s famous aside about ‘the scars on my back’ from attempting to improve public services. He followed that by his party conference speech in the September about ‘the forces of conservatism’ that were holding back public service reform.
Over the same summer, Alan Langlands, the NHS chief executive, held an executive away day at which he told colleagues that things were so bad that to get the NHS back to a high quality service it needed not 4 or 5% real-terms increases but growth rates of 7 or even 8%.
In October, Frank Dobson, Labour’s health secretary since 1997, who had proved adept at extracting at least some extra cash from the Treasury in these straitened times, was persuaded – to his later regret – to leave the post to run for mayor of London. As one of his final acts he sent Blair a personal note – outside of the official channels – telling him, ‘If you want a first-class service, you are going to have to pay a first-class fare.’ While also, in Dobson’s inimitable phrasing, ‘giving him plenty of examples of things that we were crap at’. Dobson says that was ‘probably the most important thing that I did as health secretary, full stop’. A couple of years later, the Wanless review having delivered, Blair went to the trouble of sending Dobson, now a backbencher, a note saying, in Dobson’s recollection, that ‘it would not have happened, but for your note triggering it off’.
In Downing Street, Robert Hill, Blair’s health adviser, had also become convinced that the NHS needed a serious and lasting injection of funds. ‘Over the preceding 2 years I had written a series of notes pointing out the dire financial straits of the NHS. We were constantly having to shove stop-gap amounts of money in, and having fairly constant battles with the Treasury on that, including a huge row over the funding for statins when the national service framework for heart disease was introduced. They resisted that like mad. My role was to convince the PM that this was not the department doing a bleeding stump act. That there was a genuine problem here, and that we can’t go on like this.’
For these and other reasons, Blair knew that the service needed a serious injection of long-term funding, while believing in his bones that the NHS, like much of the rest of the public services, needed reform. Alan Milburn, Dobson’s successor, shared those views. If anything even more strongly.
Alan Milburn arrives
Milburn was a rising star, already tipped by some as a possible successor to Tony Blair, which did nothing to endear him to Gordon Brown, who believed he had a deal under which he would take over as Prime Minister if Labour won a second term.
Milburn had been minister of state for health between 1997 and late 1998 and closely involved in some of Labour’s lasting initiatives: the creation of what became a proper NHS inspectorate in the Commission for Health Improvement (now the Care Quality Commission) and NICE (the National Institute for Health and Care Excellence). He had, however, spent the intervening 10 months as chief secretary to the Treasury, a role that had given him a good idea of what might be possible financially. Milburn was also aware of private Labour party polling showing that support for the NHS was diminishing, particularly among the young. He believed both that some pretty fundamental reform was needed in order to produce better outcomes, and to make the service less paternalistic, less institutionalised, and more consumer oriented. But he also believed that he was unlikely to get that until sufficient extra money was on the table to allow the argument with staff to be one about reform, not the shortage of money. Milburn adopted a high-risk strategy.
2 days after his return to health he told the regular dinner of the ‘top ten’ – leading figures from the medical royal colleges, the BMA and the like – that the NHS was in ‘the last chance saloon.’ If it did not modernise, he said, it would die. In public he talked up figures showing huge variations in the cost of treatment around the country, large variations in outcomes, and indeed of patients’ chances of dying in hospital, depending on where they were treated.
There was a twin-track approach here. By highlighting the service’s variations in performance, and by implicitly attacking the BMA for obstructing progress, Milburn hoped to foster a greater pace of change. But by emphasising the service’s inadequacies he hoped also to loosen the Treasury purse strings. Blair, as we have seen, had already agreed that the service needed much more money. And in the November and December of 1999, there were heavy public hints from both Blair and Milburn that more money would indeed be forthcoming.,
The problem – entirely unsurprisingly – was that the Chancellor wanted to control all of this. Whatever other ministers might think, including the Prime Minister, he regarded public spending as entirely his bailiwick. He was already working on both what the March Budget might contain, and on Labour’s second comprehensive Spending Review due for the July of 2000, which would set out the spending plans for all departments for the next 3 years.
Early in Milburn’s tenure in an, at the time, off-the-record conversation (though to be fair Milburn does not recall this), he told this reporter, ‘It’s not him I need to convince,’ – gesturing towards Brown’s Treasury – ‘It’s him,’ – gesturing towards Number 10. In his memoir, Blair says he had ‘a conversation or several’ with Brown during this period about greater spending but ‘he was fairly adamant against doing anything big’.
Winter arrives… And so does Winston
The final and perhaps decisive step in the lead-up to Breakfast with Frost was the winter of 1999/2000. A later analysis by the Department of Health was to conclude that the NHS in fact did better that year than the year before. But that was not what it felt like at the time, and certainly not what the media headlines said.
As December turned into January there was a moderate outbreak of flu, something Labour had managed to escape during its first two winters in government. It was well short of the official definition of an epidemic. But alongside it went a 15-year high in other respiratory illnesses. The result was long trolley waits in casualty, cancelled operations and a shortage of critical care beds. A consultant from the Royal London made headlines by going on television news between Christmas and January to warn that seriously ill patients were being shunted around the country to find a critical care bed, and were thus at serious risk. Alongside this was the damaging story of an Ipswich hospital hiring a freezer lorry because its mortuary was full. The most distressing story – again the subject of headlines widely– was that of Mavis Skeet, a 78-year-old woman with throat cancer, whose operation was cancelled four times in 5 weeks, to the point where it became inoperable.
The final straw was Robert Winston. An internationally regarded fertility specialist, Lord Winston was the most famous television doctor of the day. Not only was he a Labour peer, he was seen as close to the Blairs. He gave an interview to the New Statesman that made the papers the Friday before Breakfast with Frost. He relayed the experience of his 87-year-old mother on a mixed sex ward after a 13-hour wait in casualty. ‘None of her drugs were given on time, she missed meals, and was found lying on the floor when the morning staff came on… she caught an infection and now has a leg ulcer.’ That was, he said, ‘normal’ adding that ‘the terrifying thing is that we accept it.’
On top of the personal story, however, was a much broader attack on Labour’s performance and tenure. The government, he said, had been deceitful in its claims to have abolished the internal market. It was providing funding ‘not as good as Poland’s’, while it was attempting to blame everything on its Conservative predecessor. Phrases like ‘we haven’t told the truth’ littered the article. The way the NHS was funded might even have to change, he said, if Britain was to have a health care system to match that of even of its less well-off neighbours.
Combined with the other terrible headlines, this was devastating stuff. That winter was dreadful. Indeed, Milburn is on the record as saying that he might not have survived that winter had he not returned, only recently, to health having had that crucial break at the Treasury in between. By now, thanks to the service’s performance and the arguments about whether the NHS was sustainable, only three of the main national newspapers were still, in their leader columns, supporting the NHS model – as opposed to some other arrangement involving more charges, private insurance, or social insurance, or at least that a debate should be held about it.
Time for breakfast
On the Saturday 15 January 2000, according to Blair’s account of his time in office, he had already decided to make a commitment ‘to raise NHS spending to roughly the EU average.’ He says he worked through the possible permutations of what that would mean with Robert Hill, his health adviser – although Hill has no clear memory of that. ‘I talked again to Gordon,’ Blair says, ‘who became more adamant [against doing anything big]. But I was convinced, as a matter of profound political strategy, that the decision had to be taken and now.’ To signal such a commitment would have its own determinative impact, he says. He also took the view that with Milburn now at health, ‘we had a chance of getting the reform’.
So the next day Blair went on Breakfast with Frost and deliberately said it. In Blair’s words, ‘It was a straightforward pre-emption.’ And to reporters like me on the day, it was clear that it was a bounce on his Chancellor. By early afternoon it was possible to talk to Simon Stevens, Milburn’s special adviser, who had caught up with what was going on, and to Robert Hill in Downing Street who said ‘we’ll get you those figures’ as I was giving him my understanding of them. No amount of phone calls, however, managed to raise the Chancellor’s advisers. These days Ed Balls, Gordon Brown’s most senior special adviser and a future Labour Cabinet minister and shadow chancellor, agrees. ‘It did come out the blue for us [at the Treasury]’. But that leads us to the other, and not incompatible, version of the Wanless review’s origins.
Origins version two: ‘This did not happen because of one interview on the Frost programme’
Towards the end of 1999, the Treasury was already working towards the March 2000 Budget and Labour’s second comprehensive Spending Review, due in the July. Gordon Brown, Ed Balls, Ed Miliband – Brown’s other top adviser – and indeed the Treasury more broadly, knew something had to be done about the NHS.
Thinking, on a jet plane
‘We had levered some more money into the NHS in the first comprehensive Spending Review in 1998,’ Balls says. ‘But we were continually moving short-term sums of extra money in to deal with winter pressures and the like, and we needed to get something that changed the paradigm in terms of modern health spending.
‘There was more that we could do within our fiscal rules. But unless you could make the case for more taxation there was only so far that you could go. So, by the end of 1999, we felt we had got to the end of the road. If we were going to fight the [2001] election on “schools and hospitals first”, which was our plan, we did not feel as though a 3-year settlement for health in the 2000 Spending Review would be enough. We needed a paradigm shift. And our view was that you had to make the case for the need before you could go on to the argument about tax.
‘So what we needed was a long-term vision of the sort of health service we wanted, and fight the election with that plan. But have a financing review which has not yet reported, but will report after the election. And then after the election you say, “We have a mandate from the election to deliver our 10-year plan, and the financing report, which was in our manifesto, says this is what is needed…”, and therefore we get on and do it.
‘So, at the end of 1999, Ed [Miliband] and I were flying out to New York for an international meeting and talked all this through before we met Gordon and Bob Shrum [the long-time Democrat political consultant]. We came up with a twin-track approach. Which was first to push the perspective about the National Health Service into a longer time frame, and then to start a pre-election debate about the funding of the National Health Service – one which could figure in the manifesto for the general election, but which would not be concluded until we had a mandate to deliver that manifesto in the second term.’
It was tax, not just spend
As far as Ed Balls is concerned, that was the origin of the Wanless report. A report that would make the case for much more generous funding for the NHS and which would, in turn, justify the tax increase needed to achieve it. And that too is the view of Ed Miliband, Brown’s other key adviser and future Labour party leader. Miliband also – quite independently – remembers that long plane journey and the lengthy discussion ‘about how do you argue for the proper financing of the health service?’
‘And I remember Gordon saying, “You can’t just come out of the middle of nowhere and say this is what we are going to do. You have to methodically go out there and make the case for it.” We needed a review.’
Wanless, Miliband says, ‘certainly did not happen just because of one interview on the Frost programme. For the Treasury to be volunteering to spend a lot of money on the health service is quite an unusual thing. But that was the case. It was long planned in the sense of making this argument about financing the health service properly, and then raising the taxation needed for that to happen.’
Nick Macpherson, the Treasury’s director for public services at the time and later its permanent secretary, confirms that by the end of the 1990s the Treasury was well aware that the NHS needed more money, but was also thinking about how to raise the revenue to pay for it. There had been some growth in NHS expenditure since Labour took power, Macpherson says, ‘But I think it is fair to say that the outputs of the service were not consistent with the vision of a New Labour government, elected with a huge majority, which was promising not just to change public services but to transform them.’
In the late 1990s there had been a big surge in revenue. ‘But by the early 2000s the days when we were awash with tax revenues were beginning to recede. So if you were going to give the NHS more resources over the medium term, which I think everyone agreed was almost certainly necessary, you needed to get public opinion on side.
‘So, from a Chancellorial and Treasury point of view this wasn’t simply about announcing spending increases. It was also about trying to create a bit of a public debate to facilitate serious revenue measures that would help finance the health service in the medium to long term. Like a lot of the reviews that Mr Brown had commissioned, and there had been quite a few of them by then, the review process was designed to try to create an emerging consensus.’
By 2001, Macpherson says, Milburn and Blair were developing much more of a reform agenda for the NHS, ‘But I don’t think the Blair gang ever really got their head around the revenue which would be necessary to finance it. So that was part of the thinking underpinning Wanless.’
Love’s Labour’s Lost: Number 11, Number 10 and the Department of Health
The Treasury was, of course, interested not just in more money for the NHS but in the modernisation of its operations to provide better and more productive services. And in the Blair government, there was, of course, the second power base in Gordon Brown’s Treasury, which had already introduced hundreds of targets for public service improvements through detailed departmental public service agreements, including for health. At the same time, Blair, as we already have seen, was deeply committed to public sector reform in general, and of the NHS in particular.
One factor in this, Balls says, was the Treasury’s relationship with health. ‘With some departments, our relationship was very bilateral. With trade and industry, for example, and with the regions and transport. In the case of education, Tony had things he cared about and Gordon had things he cared about, and Gordon always had a good relationship with Blunkett [David Blunkett, Labour’s first education secretary]. Whereas with health, from a policy point of view, the health department was really run from Number 10. We’d discuss things with Jeremy Heywood [the Prime Minister’s principal private secretary and future Cabinet secretary] and Robert Hill [Blair’s health adviser], and we would have left it to Hill to sort the department out.’ Which is also a polite way of saying that Alan Milburn and Gordon Brown were not exactly soulmates.
‘We were in this conversation with Number 10 about all this already. We were wanting to focus on what kind of long-term health service are we trying to achieve? What goals do we want to achieve? What outcomes do we need? And how do we get the financing to do it? And Tony knew that is what we wanted to do. It was what he wanted to do.
‘And then suddenly, out of the blue, on the Frost programme, he says this thing about getting us up to the EU share.’
Ed Balls’s theory is that Robert Hill had written Blair a policy note saying, ‘We really should be ambitious in going for the EU share of GDP.’ ‘Tony reads it and goes on the Frost programme and says it. And maybe he said it because he wanted to be on the lead on health for the Budget, and maybe it was just in his head and he said it… and who cares?’
Hill is not entirely sure about that, and the government papers that would make it clear are not yet available. Hill says: ‘I was asked to write a note ahead of the interview, but I wasn’t really given the context, and I was not privy to the way the Prime Minister’s mind was working. I had previously briefed the PM on the percentage of GDP that various European nations were spending on health. But my recollection is that this was more in the context of bolstering the case for upping our game on health spending, rather than understanding that we were specifically considering going for the EU average. I genuinely can’t remember whether I put the EU figures in the note ahead of the Frost programme. Certainly there was no modelling.
‘When he said it, I was surprised by the precision of the commitment. I certainly wasn’t sitting there thinking Oh, right he has said it – good. Tick. If I was expecting anything, it was that he might commit a Labour government to more substantial real-terms increases in NHS spending year on year. If I’d been expecting the commitment to the EU average, I wouldn’t have needed to put that call in to Clive Smee.’
Furthermore, in sharp contrast to Ed Balls’s recollection, Hills says he was unaware of the Treasury game plan that became the Wanless report, it becoming clear only after Breakfast with Frost with ‘the Treasury becoming more open about the Wanless project’.
What is clear is that, in Ed Balls’s words, Blair’s announcement was both annoying and frustrating. ‘Gordon was grumpy about it: “Why is he doing it on the Frost programme when we are trying to do it in the Budget?”.’
‘The reason we were frustrated was twofold. One, he made the measure of success the input, not the output. And our whole strategy was to have the money following the goal. The goal should be about the ambition of our health agenda, and there is nothing galvanising or dynamic about the EU share of GDP. It is an input. It doesn’t say anything about why, or how well it is spent.
‘And secondly, we always knew that to win this argument, we had to put in place the reforms and accountability which would persuade people that the money would be well spent – and the problem with that announcement was it was not really attached to any reform. In that sense it was a bit old fashioned. Let us set an input spending target rather than focus on the outcomes you wanted to get for that. So it was a bit jarring for our political strategy. But you know – on the balance of this – while we were annoyed about it, we then thought fine. This was going to help shake things up. He was throwing health into a longer term perspective. So it was consistent with everything we were trying to do.
‘But I would have had some slightly difficult conversations with Jeremy [Heywood] about why is he doing this? Why didn’t we talk about this in advance? Why was there not a bit more conditionality?’
And, Balls says, it was unusual. Despite what their staff dubbed ‘the TB/GBs’, ‘for all that is said about Blair and Brown, we very rarely surprised each other. There was genuinely a conversation about how things were to be done. If there was a disagreement it was normally resolved before things went out. A bit of give here, or a bit of give there. There was not normally ‘out of the blue’. Tony rarely saw Gordon interviews and thought Oh God, why has he said that? – or vice versa.’
Alignment at last
What immediately followed Breakfast with Frost, according to Blair, was ‘a few days of tin-helmet time with Gordon’ but the announcement ‘allowed me to get on with the other part of the plan: to work with Alan on a serious proposal of reform’.
What eventually emerged, to go with the March Budget, was a formal statement from Blair the day afterwards. It announced work on a multi-year plan for modernisation and reform of the NHS.
Ed Balls says the Treasury team pressed hard for that. ‘We needed something that showed we had ambitions which went beyond the 2000 Spending Review, and it needed to be big and significant, so the PM agreed to do the statement on the 10-year plan the day afterwards.’ The Prime Minister fronting the statement, with the Chancellor sitting ostentatiously alongside him, was ‘symbolic and important’, Balls says, underlining the scale of the ambition.
In the wake of Breakfast with Frost, however, some commentators viewed that announcement much more cynically. Brown had found the money, or at least the first tranche of it, but Blair was in charge of spending it. If the project failed, Brown would know, and would make sure that everybody else knew who was to blame.
In his statement Blair spelled out the manifold challenges that the NHS faced, promising action. He invited the BMA, the royal colleges, the unions and others to help devise by July ‘a detailed 4-year action plan for the NHS’. That did indeed become the ‘big tent’ operation that produced the NHS Plan, subtitled A plan for investment. A plan for reform – although by then it had morphed into a 10-year plan. Its promises included a more responsive service and more of pretty much everything – staff, equipment, hospitals, students – while setting Labour’s first targets for cutting waiting times. It also announced a new ‘concordat’ with the private sector, without that new relationship being very precisely defined. And, of course, in the Budget the Chancellor had announced the as yet unnamed Wanless review.
Blair and Brown were now, at least temporarily, aligned. The strategy that would lead to the tax increase necessary to hugely improve the NHS, and increase health expenditure up to the EU average, was in place.
* See, for example: Glaziers and window breakers: former health secretaries in their own words. 2nd edn. The Health Foundation, 2020 (https://doi.org/10.37829/HF-2020-C03); Never again? The story of the Health and Social Care Act 2012, 2012; ‘The world’s biggest quango’: The first five years of NHS England, 2018 (both Institute for Government and The King’s Fund); and finally, The five giants: A biography of the welfare state, William Collins, 2017.
† At the time I was public policy editor at the Financial Times.
‡ The only remotely comparable independent exercise was the Guillebaud report of 1956. Set up by the Treasury in the hope it would recommend cost constraints at a time when NHS expenditure appeared to be out of control, the report concluded that to be anything but the case. Instead, it made recommendations that ‘will tend to increase the future cost’. Unlike Wanless, however, it did not make long-term projections of likely future costs.
§ ‘Internal market’ was always a misnomer. In theory, and indeed at the time in practice, the private sector competed for NHS contracts although to a very limited extent.
¶ Known in the jargon as a ‘quasi-market’ because, while it had elements akin to a private sector market, patients – of course – did not themselves pay.
** I remember declining to take part in a BBC programme whose thesis was that privatisation of NHS trusts was inevitable. My view was that it was possible, but not inevitable.
†† Seven out of ten felt waiting times were too long in polling for the NHS Plan. See Annex 1, The NHS Plan. Department of Health; 2000 (http://1nj5ms2lli5hdggbe3mm7ms5.wpengine.netdna-cdn.com/files/2010/03/pnsuk1.pdf).
‡‡ For example, Blair had already set up a cancer action taskforce. See: https://reader.health.org.uk/unfinished-business/timeline
§§ Labour had abolished GP fundholding, but not the purchaser/provider split. Health authorities had morphed into Primary Care Trusts which continued to commission care from nominally competing NHS trusts and the private sector, even though they had had a duty of cooperation placed on them.
¶¶ The three were The Guardian, the Daily Mirror and the Financial Times.
*** The fiscal rules were that Labour would borrow only for capital investment, financing current expenditure out of tax and other revenues. And that it would keep public sector debt at a ‘stable and prudent level’, which it defined as less than 40% of GDP. Both rules applied on average over the economic cycle, rather than having to be met each and every year.
††† This chimes with Gordon Brown’s account in his memoir My life, our times. Vintage; 2017 (p 163).
‡‡‡ Gordon Brown, in his memoir, ibid, (p 164) says that, ‘Tony had announced the gain – the spending increase – without announcing the pain – the tax rise.’
§§§ One other exception was Blair’s announcement in March 1999 that the government intended to abolish child poverty over 20 years.
The Wanless review and reports
Getting going
The chair and terms of reference
The Treasury lead for the Wanless review was Anita Charlesworth, deputy director of public spending at the time. It was not until January 2001, almost a year after Breakfast with Frost, that Charlesworth was appointed and substantive work started. As a result the review was conducted under appreciable time pressure.
‘The first I heard of it,’ Anita Charlesworth says, ‘is when Nick Macpherson came to me and said, “They want to do a review of NHS funding, would you lead it?” And I said “Well, there is no way of doing it that will not come up with a huge number. And I don’t want to do something like that for a year and more and then you have to bury it because no one likes the answer. So are they really up for that?”
‘So he said, “Go and see Ed Balls.” And it was clear that actually they were up for it, and they did understand that this was going to be a very large number.’
Furthermore, ‘It was clear that they were interested in other issues beyond the politically important one of waiting times. Issues such as outcomes. And that was to Treasury ministers’ credit. You might say, well once you’ve set the target of getting to the European average, why would you bother doing this?
‘But people did want to think more fundamentally. Part of that was Gordon Brown’s view that if you are going to start to spend – and he clearly wanted to spend – they had to be seen not just to be spenders. The ‘something for something’ agenda, the ‘rights and responsibilities’ agenda, the ‘prudence with a purpose’ agenda. All of that was deeply felt. Deeply felt by him personally, but also felt by him to be incredibly important for a Labour government that was going to start to spend. He felt that had to be handled really carefully.
‘So he really did want to be very clear about what you were going to get for the money, and how that would deliver both substantive improvements but also a more efficient system. There was a very strong desire to tilt the focus of the system towards not just access issues but outcomes. And I certainly felt it was a worthwhile endeavour to be doing, for those reasons.’
Two of the most important questions to settle were the terms of reference and the chair. The terms of reference reflected those in the Chancellor’s Budget statement and amplified them. Namely:
- To examine the technological, demographic and medical trends over the next two decades that may affect the health service in the UK as a whole.
- In the light of (1), to identify the key factors which will determine the financial and other resources required to ensure that the NHS can provide a publicly funded, comprehensive, high-quality service on the basis of clinical need and not the ability to pay.
- To report to the Chancellor by April 2002, to allow him to consider the possible implications of this analysis for the government’s wider fiscal and economic strategies in the medium term; and to inform discussions in the next Spending Review in 2002.
The devolved administrations – Scotland, Wales and Northern Ireland – were to be involved.
The terms of reference did three things. First, they made it clear that the NHS model was not in question. Second, it did not need much reading between the lines of point three to see that this might be used to justify tax increases. And third – by being silent on the issue – this review was not going to look at the management and organisation of the NHS. That was going to remain Milburn and Blair’s jealously guarded territory – via the NHS Plan and what followed from that.
Who was to chair it? Discussions were held with two people. Adair Turner, the former director general of the Confederation of British Industry, and Derek Wanless, who had recently ceased to be the group chief executive of NatWest. Wanless was a member of the Statistics Commission, a body that Gordon Brown and the Treasury had just created and which had brought the two into contact. As Ed Balls puts it: ‘We wanted it to be somebody who would be a credible person talking about the money and the finances, and productivity and value for money. But also someone who was a believer in the National Health Service.’
At this time, well before the financial crash of 2008, New Labour in general, and Gordon Brown in particular, had a distinct fondness for using bankers and business people as outside chairs for the huge range of external reviews, or external advisory bodies, set up in Labour’s early years. Part of its ‘big tent’ approach to politics.
Thus, to take just two examples from the many, Martin Taylor, the chief executive of Barclays, had chaired a task force on work incentives looking at social security benefits, tax and national insurance and that had recommended the introduction of tax credits. Sir Colin Marshall, the chairman of British Airways, had a look at industrial energy use, a report that led to the climate change levy. Both policies that Gordon Brown wanted to adopt, but using, as with Wanless, an external imprimatur to help make the case for the change.
Adair Turner fell out of the running because he wanted not just to look at likely trends and demands over the next couple of decades, but to ask the question about whether a tax-funded NHS was the right model. It is all but certain, from his other writings and pronouncements, that Turner would have concluded in its favour, at least in the medium term. But he was not prepared to undertake the review without asking the question.
But as Balls says: ‘The reality is that this was a Labour government committed to a National Health Service in the public sector, based on need not ability to pay and free at the point of use. So we were not looking for someone who was going to come along and go back to first principles. This was not about the financing of UK health care, it was about the financing of the NHS into the future… we were not going to ask an unelected Adair Turner, former head of the CBI, to do a review into whether the basis of the Labour party manifesto of 1997 was correct.’ That conversation therefore ended, though amicably enough.
Instead the task went to Derek Wanless who was happy with the constraint on the terms of reference. Although, as we shall see, the question of alternative funding mechanisms did eventually surface in the interim report.
Style and methodology
Anita Charlesworth says: ‘Derek was no socialist. He was a banker. But he did believe in public services in general, and the NHS in particular. And that was important for people in the NHS. I think for everybody who met him through the process, many started with a fair degree of scepticism about a banker. But he did, I think, win everybody over. People had confidence in him. And that was really important.
‘Furthermore, he was a statistician by background and that was also important. He was very analytical. It was always clear that this was aimed at the 2002 Budget. So we did not have very much time to do this, and you needed someone who gets the hang of the numbers very quickly. So his background in statistics helped a lot. He was very numerate.
‘The doctors and the analysts liked him because he was a technocrat in many ways. He listened to evidence and he liked evidence. So he got a lot of cooperation and collaboration. And, of course, canny people recognised the massive opportunity that this offered. It was also important that he was from Newcastle.
‘Obviously, Alan Milburn was not entirely happy about this process. I had to sit in a meeting where Alan Milburn and Derek Wanless met each other, talked about the football club, and established that Derek was OK. It also established that Derek would deal with the funding and would not look at how the NHS was run. And that was very much Milburn’s stipulation. He was not having the Treasury telling him how to run the NHS.
‘What I’ve said may imply that Derek was up for being pushed around. He wasn’t at all. He was very clear at the beginning that it would be his answer to this question, and that it would be published regardless. He made that absolutely clear. And he was later to stretch his terms of reference by at least taking a look at social care.’
The Wanless review may have been born out of deep internal tensions within the Labour government. But once the terms of reference had been agreed and the team appointed, it was all pretty much sweetness and light.
The Treasury team was assembled and to it Steve Dunn was seconded, an economist by background and a member of the Department of Health’s recently formed strategy unit. Dunn had in turn been placed into the unit by Clive Smee, who wanted to know what it was up to. ‘I was, so to speak, Clive’s mole in the strategy unit – but they knew that,’ Steve Dunn says. During the Wanless review Dunn played a similar mole-like role, that was similarly recognised. He reported back into the strategy unit as he spent 4 days a week in the Treasury, and a day back in the department.
There was, however, no real tension. Anita Charlesworth says that Smee and his team were ‘absolutely critical’ with Robert Anderson and John Henderson, two senior economic analysts in Smee’s team, doing a lot of the work. It also helped that Charlesworth had previously worked for Smee and knew many in the team.
If you were to carry out the Wanless exercise today, Charlesworth says, ‘There is a lot of data that is now routinely published that you could use.’ But back then there was less information and even less of it was routinely published. ‘So the technical task of doing the review required a very great deal of cooperation and support from the system, particularly from the public health community, the stats community, the economists, etc. And most of those worked in the Department of Health, getting the data and getting it organised so that we could use it. Without serious cooperation, support and collaboration, we would have been sunk.’
The review originally intended to build up the profile of NHS costs disease by disease, but there were insufficient data to do that. What came to the rescue – and proved in many ways to be the technical backbone of the report – were the National Service Frameworks. These documents, originally commissioned in Frank Dobson’s time as health secretary, set out the standards of care for particular disease areas, pointing to the most effective treatments both clinically and in terms of value for money, while suggesting the best way to organise services. Detailed costings had gone into them, not least to help persuade the Treasury to provide funding. As Wanless was getting going, these covered only coronary heart disease, cancer, renal disease, diabetes and one being developed for mental health. Between them, the five covered only around 10% of NHS expenditure. But between them they also accounted for about 50% of all mortality and some 12% of morbidity.
‘A huge amount of work had been done to build and cost those,’ Charlesworth says, ‘and I think Clive, in the nicest possible way, added a huge amount to their cost for the purposes of the Wanless review. Some of the costings proved reasonably flexible … and we could not have done that depth of work in the time available.
‘Furthermore, a lot of people in the department had worked on those. They were also clinically led, so in developing them the department had built a network of clinical engagement and consensus involving all sorts of people, including the royal colleges, and we were able to build off that.’
The review also created an external advisory group that helped identify what data were more than likely available if you knew what to ask for. As Charlesworth puts it: ‘You can’t always ask for what you don’t know about. And sometimes these sorts of review can struggle because if people have not produced things in the way you need them, you may not know that can in fact be done. So we used the advisory group to be able to get at those sorts of things officially.’
The review held three workshops, one each hosted by the Nuffield Trust, The King’s Fund and the Association of British Pharmaceutical Industries, with similar events in Edinburgh, Cardiff and Belfast to ensure engagement across the UK. It visited the United States and Australia, the latter including discussions with delegates from New Zealand. And in October 2001 it held a wider 1-day conference, just before publication of the interim report in November, to which selected media were invited.
And across the whole exercise there was a cross-departmental steering group of civil servants, chaired by Nick Macpherson, whose membership included Nigel Crisp, the NHS chief executive and permanent secretary at the Department of Health, and Liam Donaldson, the chief medical officer. ‘This was not one of those reviews that was done in secret,’ Nick Macpherson says. ‘It was all pretty transparent, and the cross-Whitehall group allowed everybody to feel they knew what was going on, and they could report back to ministers if they had problems. But I don’t recall any.’
Box 2: Summary of the interim report, November 2001
The interim report opened with two core questions. ‘What are people likely to want [from the NHS] in 20 years’ time? And what resources likely are required to deliver the service?’ It underlined that this was ‘the first time in the history of the NHS that such a long-term assessment of resource needs has been attempted’ – while acknowledging that looking so far ahead ‘is fraught with difficulty’.
It set out funding over the 40 previous years, during which annual increases had see-sawed between +11% and -1% in real terms, noting that ‘this variability can only have added to the difficulty of managing the service effectively and efficiently’. The report then took what looked to be a carefully selected group of comparator countries against which to benchmark the NHS’s performance – France, Germany, the Netherlands and Sweden, along with Australia, Canada and New Zealand. These countries were chosen, the report says, for having similar aspirations to high quality and comprehensive care, while having incomes per head that were broadly similar. The comparison, across a range of measures, painted a generally unhappy picture. Survival rates for cancer lagged well behind European comparators, for example. More children died in the first year of life than in any of the comparator countries other than New Zealand. Health outcomes generally were poor. Waiting times for treatment were long.
But it then set out what was arguably the killer fact in either the interim or the final report. Namely, a widening gap had developed between UK health spending as a share of GDP and the average spent in the EU. Over the 16 years between 1972 and 1988, the cumulative underspend compared with the EU average was between £220bn and £267bn, depending on whether an income-weighted or unweighted average was used. ‘Not surprisingly, with such significantly lower spending, UK health service outcomes have lagged behind continental European performance.’ Very drily, it noted that ‘the surprise may be that the gap in many measured outcomes is not bigger, given the size of the cumulative spending gap’ (p 37).
The interim report did look at funding mechanisms, concluding, unsurprisingly given the terms of reference, that general taxation held up well against the alternatives. ‘There is no evidence that any alternative financing method to the UK’s would deliver a given quality of health care at a lower cost to the economy. Indeed other systems seem likely to prove more costly.’ (para 2.21).
It discussed the methodology for estimating the future demand for resources, saying that ideally they would be built bottom-up on a disease-by-disease basis. But that was only possible in the limited areas where the government had started to create the already mentioned National Service Frameworks for specific conditions. In the absence of better disease data, it took a life course approach, using a mix of demographic data and figures showing that average annual expenditure varied by age from around £2,000 per head for births and for those aged 85 and older, to a couple of hundred pounds a head on average for those aged 5–15 (p 15).
It acknowledged that patient expectations would rise, with future patients likely to be better educated, more affluent, less deferential and wanting more choice. They would also want better integrated care, much shorter waiting times, and improved accommodation – ‘not The Ritz, but not the YMCA’. And it set out a series of questions for consultation around all these issues, to help inform the final report.
The interim report also noted, accurately, ‘Trying to look ahead over such a long period of time is fraught with difficulties. The uncertainties are huge.’ By way of illustration, the report expressed concern about a shortage of cardiac surgeons, but, entirely understandably, failed to spot the rapid rise that was on its way in interventional radiology, which has meant that procedures, such as revascularisation, could be carried out by others. Equally, the section on delivering quality mental health care considers drug costs but failed to foresee the rise in the use of CBT and other talking therapies that was to come within the next 5 or so years.
The interim report
The interim report ploughed the ground and sowed the seeds for the final report to come. It laid out the core arguments about resourcing, including comparisons with other countries’ spending and set out the review’s methodology. But it did so without yet putting any numbers on the increases it was to recommend in the final report.
It contained one surprise, given the original debate with Adair Turner over its terms of reference. The report noted that it was set up to examine the resources required to run the health service in 20 years’ time – and that it was ‘not set up to examine the way in which those resources are financed’.
Nonetheless, its fourth chapter did examine alternative funding mechanisms, including social insurance, out-of-pocket payments and private insurance, and how those were used in the countries that it had chosen for comparison. Entirely unsurprisingly, it concluded that the UK’s model of general taxation held up well. ‘There is no evidence,’ it said, ‘that any alternative financing method to the UK’s would deliver a given quality of health care at a lower cost to the economy. Indeed other systems seem likely to prove more costly.’
Anita Charlesworth’s recollection is that it was Ed Balls who instigated the financing section. ‘We had not set ourselves up to look at alternative financing methods. It was not in the brief, and it was pretty much excluded by the terms of reference. Indeed, I had spent a lot of time explaining to those we talked to that it was outside the brief. And then suddenly it was in. So we had to do this very rapidly. And it shows, I think, in the interim report.’
Balls confirms that the decision to put in a section on funding models came from him. ‘The Conservative Party’s line at the time was to paint the NHS as a failed model,’ he says. ‘And I remember a discussion with the editorial people at The Times as the interim report was being done and them wanting to have a discussion about whether the Wanless report was ducking the big issue – which was whether a tax-funded NHS was the right model. So what became clear is that while our focus was on matching reforms with resource to deliver a 21st century National Health Service, there was a prior argument to be fought about whether the NHS was the right model.
‘It was never Wanless’s job to do that. It was our job, and the Conservatives were seeking to open up that dividing line. So I said to Anita that the interim report will be the platform on which we will have to go out and win arguments between now and the Budget. I know that the whole terms of reference are about a free-at-the-point-of-use, tax-funded health service. That is our starting point, and we are not asking Derek to examine that. But if there is nothing at all in the report about that issue, and why that is our starting point, it is going to look pretty weird. So would Derek be happy in having a short discussion in the report about why this is the starting point in the terms of reference? And that was what went in.’
With a bit of a blip: ‘I have not sought to bury anything’
The inclusion of a section on alternative funding mechanisms led to a bit of a blip when the interim report was published, alongside the pre-Budget report in November 2001.
Gordon Brown, in his speech, underlined the Wanless conclusion that, ‘There is no evidence that any alternative financing method to the UK’s would deliver a given quality of health care at a lower cost to the economy. Indeed other systems seem likely to prove more costly. Nor do alternative balances of funding appear to offer scope to increase equity.’ Michael Howard, the Conservative shadow chancellor, dismissed the report in general and that finding in particular.
Given that the terms of reference were ‘… to consider a health service that was exclusively publicly funded,’ Howard said, ‘it should not surprise anyone that Mr Wanless came up with the answer that the Chancellor wanted him to find; that a publicly funded service would be better. If you ask a Labour question, you get a Labour answer.’ He added that it was ‘now clear to everyone except Gordon Brown that without fundamental reform of health care, more money will not deliver the results which people in this country are entitled to expect’.
The ‘Labour answers to Labour questions’ jibe appeared to sting. And at a press conference called 2 days later to promote the report more generally, Wanless, when challenged on the alternative funding issues, stood by his conclusion that the NHS was underfunded. And that if equity was important to the British people then a tax-funded system was the most fair and efficient way of doing it. But, he said, it was ‘not his job’ to bury alternative funding models. He promised to talk to the Association of British Insurers further about their role, adding: ‘I have not sought to bury anything for good. It would be quite presumptuous and premature to do that.’
Anita Charlesworth’s explanation is that the funding section went in late. ‘So we did not go through a big process where we exposed him to lots of views, and gave him time, and built a roundtable – with time to think about it [the issue of alternative funding mechanisms]. So it came in quite late, and I think he was still cogitating, rather unhelpfully, when the interim report came out.’ The Conservatives sought to make capital, but Wanless’s ‘it’s not my job to bury anything’ proved to be only a 1 or 2 day wonder.
That did not mean that the media reaction to the interim report was a universal welcome. Anything but. It was not just the right-wing press, for example the Daily Telegraph, which accused both Wanless and the Chancellor of closing down the argument that the NHS should continue ‘as a publicly funded monolith’. The Independent said that ‘… those with more open minds will want to consider in more depth the evidence against alternative funding methods’. Anthony Browne, The Observer’s health editor, declared: ‘Whether it is paid for by tax or by other forms such as social insurance is the subject of a national debate that Gordon Brown said we must have. We do need this debate, yet Brown also declared the answer: more tax is the only way to pay for the NHS.’
If that showed that the essential argument for the NHS model had still to be won – let alone the argument that tax rises would be needed to pay for it – work nonetheless resumed on the final report. Wanless was later to be attacked for paying insufficient attention to other countries. But between the interim and final reports the review visited France, Germany and Sweden, held discussions with the Netherlands and examined a report it had commissioned from the European Observatory on health care systems that looked at the trends and challenges in eight countries. Although, to be fair, the focus was much more on the approaches these countries were taking to long-term resource planning, rather than on alternative funding mechanisms. There was considerable time pressure. The final report was due just 4 months after the interim, to be published alongside the March Budget of 2002.
The final report
Anita Charlesworth says that both before and after the interim report, the review did a lot of heavy lifting around workforce. ‘One thing we were very worried about, alongside the money, was whether you could get the staff. Particularly if you were going to load it so upfront.
‘So we developed a workforce model that hadn’t been done before. It was a spreadsheet. It had all the right parameters, though it might not have had the right numbers! We did spend a lot of time trying to work out whether you could save staff time through things like technology, and whether giving staff more time for audit and reflection and learning would raise quality. That was quite thoughtful work. Was there a potential productivity gain? But as with much of the rest of the Wanless report, it turned out that there was nowhere where it could really dock into the system.’
The final report also contained the three scenarios of fully engaged, steady progress and slow uptake (see Box 3). These, Charlesworth says, stemmed in part from the worries of the ‘classic’ Treasury which was becoming somewhat alarmed at the huge sums that the final report was going to recommend. ‘There were Treasury officials getting very scared at growth rates of 7% a year over 20 years. The more established Treasury was not comfortable with this.’
Box 3: Summary of the final report, April 2002
The final report – Securing our future health: Taking a long-term view – took into account demography, the commitments already made in the NHS Plan of 2000, an estimate of changing patient expectations and likely changing health needs, advances in medical technology (while accepting those became less certain the further out they were projected), prices (including the cost and likely availability of skilled staff, using a workforce model) and potential levels of productivity.
It then painted three scenarios – ‘solid progress’, ‘slow uptake’, and ‘fully engaged’:
- ‘Solid progress’ assumed increased life expectancy, with 5% fewer acute health problems among older people. The result would be a mix of additional healthy and unhealthy years of life, split roughly half and half. It assumed improved curative care, with a better skill mix in the workforce, and more efficient use of IT. Younger people would be more health aware, and existing targets for public health would be met – including reduced smoking, reduced obesity, better diets and lower rates of teenage pregnancy. The gap in life expectancy between the poorest areas and the average would fall by 10%. Broadly speaking, ‘The service is fully integrated, efficient, and has closed the major gaps with other countries.’
- Under ‘slow uptake’ life expectancy still rises but more of people’s extra years are spent in ill health. The uptake of new technologies is relatively slow. Potential productivity improvements are not fully realised. The quality of care is good, but does not offer a whole system, fully integrated approach. Public health targets are not met, with levels of smoking, obesity and physical exercise essentially unchanged. This is the most pessimistic scenario.
- Under ‘fully engaged’ people live both longer and healthier, with the proportion of a life spent in ill health declining. Public health improves dramatically and patients are fully engaged with a fully integrated health and care system. The reductions in risk factors from smoking, obesity and lack of exercise are largest where they are currently highest – in the most deprived areas. In the long run, this is the least expensive scenario.
In terms of resources, Wanless judged that there was little difference between the scenarios in the first 5 years because these would be a period of catch up. It projected annual increases of between 7.1 and 7.3% in real terms. After that, the scenarios diverged. Under solid progress, health spending would rise from £68bn in 2002 to £161bn in 2022. The fully engaged scenario, which would deliver the best health outcomes, would involve an increase to £154bn. Slow uptake, which would produce the worst outcomes, would also be the most expensive, taking total spending to £184bn. In terms of share of GDP, the outcomes in 2022 ranged from 10.6% for the fully engaged scenario to 12.5% for slow uptake.
The report contained a prescient warning. ‘I believe our projections for real terms spending growth of 7.1 to 7.3% a year over the next 5 years are at the upper end of what should sensibly be spent. Indeed, to be wisely spent, they already represent a very considerable management challenge.’
The report made clear that as work had progressed it had become ever more obvious that health and social care needed to be considered together. The data available to provide similar projections for social care spending were missing, Wanless said. Nevertheless: ‘I have considered it necessary to go beyond my remit to begin to consider social care.’ Using simple projections from current spending, the report estimated that social care spending needed to rise by between 2.0 and 3.4% a year in real terms, taking spending from £6.4bn in 2002 to between £10bn and £11bn by 2022. But that made no allowance for improving the quality of social care, so those figures were ‘underestimates of the resources required’.
Any future review ‘… should fully integrate modelling and analysis of health and social care. Indeed it is for consideration whether a more immediate study of the trends affecting social care is needed’. That did not happen.
Given the worry in some parts of the Treasury over the scale of increases that the review looked set to recommend, ‘One of the things that the scenarios were about was: is there a spend to save option?’ Charlesworth points out. ‘Gordon Brown had already created a bunch of ‘invest to save’ programmes, and Derek, being a banker, instinctively wanted a return on his investment. Plus, the fully engaged scenario included a large dose of people taking responsibility for their own health, which appealed very strongly to both Gordon and Derek.
‘Essentially, the scenarios were about saying that rather than pouring money into exactly the same system, is there a way – a fully engaged scenario, with fully integrated services but people changing the way they live and taking more responsibility – that gets you down to increases in spending over the long term that are a couple of points of GDP lower than the slow uptake scenario. In other words, is there a win-win here which looks much less scary in terms of fiscal sustainability? One that delivers really strong outcomes and a good deal for the taxpayer at a lower long-term cost. That’s what the scenarios were trying to do.’
With a twist
The twist for the final report came in the form of Derek Wanless going beyond his terms of reference to say something about social care. In the end that proved not to be a major problem – at least in terms of its inclusion in the final report.
Anita Charlesworth says: ‘Derek’s eternal regret, I think, was that he did not realise at the beginning the importance of social care and just how linked it is to health.’
There were, however, two additional problems. First, assembling the data to make sensible projections on health spending was a challenge, but the data on social care were much worse. As the final report put it: ‘The review had neither the information nor the resources to be able to develop a ‘whole systems’ model’ that would have included social care.
The second issue was political, and in some ways the more profound problem for the report. Wanless was announced in March 2000, just a year after the Royal Commission on Long Term Care had reported. Labour had created it. But the commission split into a minority and majority report. One of its members neatly characterised the divide as: ‘The majority recommended what they thought a Labour government should do, the minority recommended what they thought a Labour government would do.’
The majority recommended free personal care – help with bathing, dressing, toileting and cooking for those who needed it. The relatively newly devolved government in Scotland accepted that. The Westminster government rejected it. England and Wales did put in some extra money, via the NHS, to support those in care homes who had the most extreme nursing needs. But it did not do much else. Those recent decisions made the issue intrinsically difficult to revisit.
‘The shadow cast by the Royal Commission cannot be underestimated,’ Charlesworth says. ‘It was a burning coal. And the fact that Scotland had accepted it and England rejected it was an additional layer of complexity. There was plenty of knowledge about what the options were, but with free personal care having been rejected it was quite hard to know what they were. For social care, Wanless happened at the wrong time.’
Nonetheless, Wanless felt he wanted to say something about it. In the final report he specifically noted that he had gone beyond his terms of reference and that social care should be included in any future review, for which much better data needed to be assembled.
Ed Balls says, ‘There were sensitivities about it, because of the proximity to the Royal Commission and what Scotland had done. But Anita was one of the best, most savvy civil servants and she was on our wavelength and very close to Derek. She would have come to us and said, “Derek wants to say this about social care.” And we would have said, “That’s fine … So long as this does not open up [a can of worms] …”’
As indeed Wanless’s recommendations did not. They dealt with the quantum – that spending on social care would need to rise and that much better forecasting of that was needed. But it did not get into who should pay for the higher expenditure – the future division, for example, between individuals, families or taxpayers.
‘We weren’t at the time,’ Ed Balls says, ‘seeking to solve the social care funding issue. This was about the National Health Service. 5 years later it would have been different. One could not have done a Wanless report without social care being in at the beginning.’
Or, as Nick Macpherson puts it: ‘There had been the Royal Commission. Everyone knew it was a problem. Everyone knew it needed to be addressed. But not this year thank you very much, and so it has continued to this very day …’
Publication
Finishing the report on time was a challenge. Indeed, the March 2002 Budget was pushed back to 17 April partly to allow for that, and partly because Gordon Brown and his wife Sarah had early that year lost their 10-day-old daughter Jennifer. But in the Budget, with publication of the final report taking place alongside it, Gordon Brown set the envelope for the July Spending Review. This would later spell out the precise allocations for most departments for the next 3 years.
Towards the end of an hour-long speech, however, as its final flourish, Brown laid out the NHS settlement – the fruit of the review. The NHS was to get an unprecedented 5-year deal, with sustained real terms rises of 7.4% a year – well over twice the long run average of just over 3%.
Social care was not forgotten. It was to receive 6% a year in real terms for 3 years. And with all that came the National Insurance increases to pay for it. A 1% increase in National Insurance contributions for employers, for employees and for the self-employed.
‘The fundamental long-term choice that our generation must make,’ the Chancellor said, ‘is whether the national consensus that existed for the last half century for an NHS freely accessible to all is to be renewed for the years ahead.’ The NHS 10-year plan of 2000 was already bearing fruit he argued, and the health secretary, Alan Milburn, would announce further reforms the following day. Because of these modernisation programmes, he said, resources could now follow reform. In terms of that fundamental question – whether the national consensus on the NHS would be renewed – ‘We have made our choice. This is a Budget to make our NHS the best insurance policy in the world.’
The Conservative reaction
Charles Kennedy for the Liberal Democrats welcomed the announcement. Ian Duncan Smith, by now the Conservative leader, did not. He dismissed the report because the Chancellor ‘had already told him [Wanless] what to say’. Waiting lists were rising, accident and emergency waits had grown longer, and hospital beds were blocked because care home beds had been lost, he said. The odds of surviving cancer in Britain were among the worst in Europe. The Chancellor, he argued, had refused to learn from other countries’ health systems. The announcement was merely one of ‘more talk’ and ‘more taxes’ and a prelude to ‘more failure’.
Duncan Smith was to be proved wrong about ‘more failure’. His comments on the state of the NHS had more substance. As already noted, Labour had put some additional money into the NHS in its first term. But the service has tanker-like properties. Performance takes a long time to turn, both when money is injected and when it is reduced. By the time the Wanless review was published, the service was in fact improving. But the published numbers were behind the reality, and it was taking a long time to turn. An analysis just ahead of publication of the Wanless report showed that the Department of Health was missing, or on course to miss, a third of the 35 targets the Treasury had set for it.
One more step back in time
In the summer of 2001, not long after that June’s general election, with the Wanless review under way but with NHS performance on waiting times if anything appearing to be getting worse, both Alan Milburn and Tony Blair became alarmed at the lack of progress. Each held separate weekend ‘away days’ with their staff to consider what to do. Blair commissioned Adair Turner to take a look at the part of the NHS outside Wanless’s remit – the management of the service. Milburn’s still relatively new strategy unit, along with his new adviser Paul Corrigan (Simon Stevens having moved to Number 10), got to work, with large-scale input from Stevens. The result was a programme of reform that ran in parallel to the Wanless review, but was put together entirely separately.
The outcome was the introduction of an array of more market-like mechanisms to the NHS. In effect the reinvention of the so-called ‘internal market’ in a much more sophisticated form – although health ministers would look with dagger eyes at any reporter who dared to suggest that. In its first term Labour had already created NICE to recommend which treatments the NHS should and should not adopt. It had also created the first full-blown NHS inspectorate, which it was shortly to revamp into the Commission for Healthcare Audit and Inspection (now the Care Quality Commission). But in a series of remarkable speeches from October 2001 onwards, Milburn began to trail what was shortly to be announced in detail the day after the Wanless report was published.
Delivering the NHS Plan, included the tariff – a price list of NHS treatments – that would finally and genuinely allow money to follow the patient. This restored patient choice over where they were treated, something that had largely gone missing as an unintended side effect of original internal market reforms, in which patients largely had to be treated in hospitals with whom their health authority or GP fundholder had a contract. With few exceptions, patients had had to follow the contracts, rather than money following the patient.
This time round, money would genuinely follow the patient. The tariff would ensure that hospitals that did more would get paid more, thus creating more competition than in the original version. Hospitals would be able to become ‘foundation trusts’ – rather more free-standing enterprises than NHS trusts had become. They would have some additional freedoms, and this time a stronger statutory underpinning to their nominal independence. Overseas suppliers would be brought in to compete to provide Independent Sector Treatment Centres – in effect surgical factories providing waiting list-type operations exclusively for NHS patients. In time, patients would be able to go to any private hospital willing to treat them at the NHS price. In other words, a ‘competition and choice’ model of NHS reform. It is, however, important to note, given Andrew Lansley’s Health and Social Care Act 2012 sought to take these more market-like mechanisms to extremes, ‘competition and choice’ sat alongside a set of other management tools. These included the myriad waiting time targets, their weekly pursuit through the Prime Minister’s Delivery Unit, clinical audit, and some at times decidedly vigorous performance management.
In the weeks running up to publication of the Wanless review, Number 10, the health department and the Treasury were essentially aligned on these reforms. Paul Corrigan, at the time Milburn’s heath adviser and later Blair’s, remembers taking these into Ed Balls at the Treasury, presenting them as ‘things we [the health department] believe will construct a higher return for the money you are putting in’. Things such as competition, choice and diversity of supply were, Corrigan says, ‘very Treasury sorts of things’ – and there was no push back. Indeed, he says, ‘these were slightly odd meetings’ given the Treasury’s tendency to seek to impose its own conditions over the receipt of money. ‘In the end we were to be held to account for the things we wanted to be held to account for. I can’t think of anything they imposed on us. They were all things that we imposed on ourselves.’
Later in the year there was to be a bitter and decidedly bruising battle over foundation trusts. Delivering the NHS plan declared, with no more detail, ‘we will explore options’ to allow foundation trusts ‘to access finance for capital investment under a prudential borrowing regime’. What this turned out to mean in more detail was an ability for them to borrow privately. And what complicated this was that there had never been any limit on how much private work NHS hospitals could do. Most did relatively little. But private patients made up some 20% of turnover in a few, chiefly in London. And for one or two specialist centres, such as the Royal Marsden cancer hospital, the figure was higher.
This raised two key concerns. First, if there was no cap on private patient numbers then foundation trusts that borrowed privately might well be tempted to up their percentage of private patients to service the debt. This would leave hospital patients in the same position as dental ones, where dentists, as independent contractors, mix public and private work. The public too often complained that the pricing for private treatment was opaque, and suspected that dentists pushed them towards private treatment by telling them that NHS treatment was inferior. Brown and Balls did not want that to happen to hospital patients. And there was a second, even more fundamental problem. Namely, if a hospital over-borrowed and went bust, its services could not, in political reality, be shut down. It would have to be rescued. And the Treasury would have to do the rescuing. Brown therefore insisted that their capital borrowing would have to take place within the overall NHS capital allocation. An additional layer to the dispute was, yet again, internal Labour party politics. Brown was convinced he had a deal to take over as Prime Minister, but inevitably feared a challenge: possibly, even, from Milburn. The Chancellor wanted the vote of the unions on his side in any such contest, and the health service unions were opposed not just to these issues around foundation trusts but to the whole ‘competition and choice’ agenda – including the greater use of the private sector that had been promised in Delivering the NHS plan. Resisting the idea that foundation trusts should be able to borrow privately would do the Chancellor no harm should a leadership contest occur.
The resulting row exploded into the open at the Labour Party conference in the October after the final Wanless report. It was finally settled by Brown winning the argument over private borrowing – correctly, in this author’s view, as the Treasury would have had to pick up reckless borrowing by a foundation trust. Separately, but with that, came a complex rule applied to foundation trusts so that they could not earn more in private income than the percentage they had been earning in 2006. In his memoir Blair describes the whole row as ‘endless, rancorous and destabilising’., Brown, in his account of events, makes clear that he was not prepared to tolerate a position where the government was ‘accepting all the liability, while ceding almost all control’. At the time the Wanless report was published though, such tensions, and indeed other tensions with the Treasury over the ‘choice and competition’ agenda, had yet to materialise.
The welcome for Wanless
In many quarters, the Wanless package went down well, though not with the Conservative leadership. Liam Fox, the Conservative health spokesperson, continued to argue that alternative funding mechanisms should be looked at more closely. Indeed, a week before the final report, a tape of Fox’s address to a fringe meeting at the Conservative spring conference emerged, in which he said: ‘We’ve got a problem in this country where the NHS and health care have been synonymous. We’re here to break that. That means we get money, raise money from people through tax, certainly by health insurance and even more so, it means, from self-pay. The big growth market in the UK is people paying from their own savings.’ He had added that the Conservative’s task was to convince the public that the NHS ‘won't work and cannot work’.
By contrast, Dr Ian Bogle, chair of the BMA, described the report as ‘a hugely important step forward’ and a ‘watershed for the medical profession’. The Health Service Journal called it ‘riches beyond compare’. From the private sector, Mike Hall, chief executive of Standard Life Healthcare, said the report was ‘a major step forward in revitalising the NHS’. The Daily Telegraph, in an ingenious piece of logic, called the national insurance increase ‘a scandalous breach of the spirit of Labour’s election promise not to raise income tax’. But at the same time, it published an opinion poll showing that 77% of those questioned supported the increases in NHS funding, with only 11% against. 63% felt that the increase in ‘direct taxation’ was justified, while 30% did not. A MORI poll for the Financial Times showed 65% judged the Budget to be ‘good for the country as a whole’, with just 20% taking the opposite view – making it the best received Budget in MORI’s long-running series since the 1970s.
In the immediate aftermath, and in the years running up to the 2005 general election, Ed Balls remembers citing these and other polls. ‘All the opinion polls – and we kept saying this to the Sun and the Mail, “You attack us if you want, but your readers think this is absolutely the right thing to do.”’
There was – and remains – a bit of a mystery as to why the increase was the remarkably precise 7.4% real a year over 5 years. Given that this was the first tranche of what was meant to be a 20-year programme, a rounder figure – say 7.0 or 7.5% – might have seemed more likely. There is no practical difference between the upper end of Wanless’s estimate of 7.1 to 7.3% for the first 5 years – the difference being merely the accounting base from which it was measured. So why 7.4%?
Ed Balls says with a smile, ‘We never minded a bit of spurious accuracy.’ No one interviewed for this study was able to recall quite why that figure. But Balls adds that in the run-up to the 2002 Budget, ‘The tax receipt numbers deteriorated. It was a bad January. And we had to work out how the health settlement was going to fit into the wider 2002 Spending Review. So it was quite dynamic in that period. And the 5-year number had to be consistent with the 3-year settlements for other departments – which is why we went for 3 years for social care not 5. It was not as though we had decided 9 months before that: this is the critical number for health and that is what we are going to announce.’
¶¶¶ Gordon Brown says in his memoir, ibid, that ‘I discovered that we had similar experiences growing up’ of their parents telling them the NHS had been ‘the deliverance from evil’ (p 164).
**** This may sound trite but virtually everyone interviewed for this study remarked, unprompted, what a genuinely nice man Derek Wanless was.
†††† The advisory group and the huge list of those consulted externally are listed in the interim and final reports.
‡‡‡‡ The member was Robin Wendt. See Timmins N. The five giants: A biography of the welfare state. William Collins; 2017 (pp 604–605).
§§§§ Known as NHS Continuing Health Care.
¶¶¶¶ Interview, April 2020. Somewhat extraordinarily, Gordon Brown in his memoir says these were reforms ‘that I had not been informed about – most of which I welcomed but some of which led us into huge difficulties’. My life, our times, ibid, (p 168).
***** A cap that the Health and Social Care Act 2012 raised to 49% for all types of NHS hospital.
††††† For a more detailed account of this dispute and its consequences see See Timmins N. The five giants: A biography of the welfare state. William Collins; 2017 (pp 623–625) and its references.
Aftermath and legacy
The immediate aftermath: ‘Take the money and run’
The immediate aftermath of the Wanless report might be best summed up by the phrase ‘take the money and run’. That is not precisely what the Department of Health did. But it is pretty close. Before looking at what happened to Wanless’s three scenarios of ‘fully engaged’, ‘solid state’ and ‘slow progress’ (see Box 3) it is, however, worth examining what happened to three specific recommendations that the report highlighted.
Three specific recommendations
The three recommendations were that:
- NICE should not just assess newer treatments and technologies in order to decide whether they were sufficiently cost-effective for the NHS to adopt. It should examine older ones to see if they remained cost-effective.
- A major IT programme was needed to provide electronic patient records and much better data.
- There should be much better workforce planning.
The first of these proved not to be very fruitful. As two senior figures from NICE were to explain in a British Medical Journal paper many years later, no country has found running a programme to disinvest in older and possibly ineffective treatments easy. There are questions around cost-benefit – how much might be saved in reality given the cost of reviewing many hundreds, if not thousands, of treatments? Furthermore some, including Professor Andrew Stevens, one of the longest-serving members of NICE’s appraisal committees, argues that the ‘easy’ hits, such as unnecessary tonsillectomies and overuse of grommets for glue ear, had already been largely killed off by the evidence-based medicine movement from the 1980s on. Sir Michael Rawlins, the former chair of NICE, was to argue that there is little now in the British National Formulary – the clinician’s guide to pharmaceuticals – that is actually ineffective. ‘There aren’t, now, a lot of useless drugs,’ he says, ‘and very little is spent on the few that you could argue are pretty useless. So there are no big savings there.’
A national programme for IT was launched at an eventual cost, depending on whose figures you choose to believe, of £6bn, £12bn or £20bn. It was not a success. Even now, its holy grail of an electronic patient record, fully interchangeable and accessible in all health care settings and ideally in social care, has not been achieved. It was not quite the total disaster that is often painted. It did successfully produce a unique and accessible individual patient number, hugely reducing the large dangers of one Mr Patel or Mrs Smith being muddled up with another of the same name. It did replace costly and inaccessible X-ray film with cheaper and accessible digital imaging. It provided a valuable internal messaging system for the NHS – the so-called ‘spine’ – which among other things gives access to a summary care record, electronic prescribing and electronic referrals. And it did renew some creaking hospital administration systems. But it was most definitely not value for money.
On the third of these recommendations – better workforce planning – there was some impact. Hugh Taylor, who went on to be permanent secretary in the department but who, at the time of Wanless was director general for workforce, says that when he took on the role in 1988, ‘It could not have been much worse. I inherited a complete absence of a workforce plan.’ Workforce planning had been part of the task of the regional health authorities, which had been abolished in 1996, ‘and that had never been properly replaced’.
The job was nominally devolved to NHS trusts but they, inevitably, took a very short term and very local view. The NHS Plan in 2000 had committed the government to a big expansion in medical student numbers and nurse training, ‘And there were successive attempts to set up quasi-regional planning groups under Labour,’ Taylor notes. ‘But it is genuinely difficult to do at a national level and it always tends to concentrate on the hospital sector at the expense of primary care and the social care sector, where it has always been pretty woeful. Wanless did lead to a greater emphasis on workforce planning. There was a huge planned and carefully monitored increase in workforce numbers as the extra investment came through, alongside improvements to recruitment and retention. But I wouldn’t like to say that it was ever done particularly well.’
Richard Murray, now chief executive of The King’s Fund, and who rejoined the department not long after the review to work in Clive Smee’s section says, ‘There was an impact on workforce that was probably more visible internally than externally. I am not saying this was all due to Wanless, but there were huge nurse recruitment drives with jumbo jets flying off to Manila. And you could not put up any submission for change for quite a long time without a workforce analysis. ‘How are we going to staff this?’’ The tragedy, Murray says, ‘… is that all fell away and we now have another workforce crisis’ – with, at the time of writing, the NHS waiting for another, and long overdue, workforce plan.
Dust on the shelf
Beyond those three items, however, the Wanless report was to quite rapidly gather dust on the department’s shelves. One reason, a view of Alan Milburn’s shared by a good proportion of our other interviewees, is that the Wanless report was the Treasury’s – not the health department’s.
Milburn says: ‘It was a good piece of work and the analysis was important in identifying the need for increased investment and a more engaged public. It helped make the case for the tax increase. That was all good stuff.’ But ‘… it was very much a Treasury play, and the subterranean politics were all about Gordon’s power grab over the future of the NHS – and in the end that all failed.’ While the exercise was under way, Milburn points out, ‘It didn’t cause me any sleepless nights. I was clear that whatever happened, Wanless or no Wanless, I was going to secure large increases in funding for the NHS and for social care, because Tony had made his promise – and Tony and I were aligned.
‘The internal politics massively devalued the report’s purchase. That was not Derek’s fault. He was an innocent bystander. But it was a Treasury exercise. The Treasury can muscle as much as it likes, but unless the ownership is jointly and separately shared with the relevant delivery department then it is going to go nowhere. It inevitably turned to dust.’
Richard Murray says, ‘There was no constituency for it within the department. The only people who really spoke about it were my fellow analysts – who had done a lot of work on it. But the fully engaged, not engaged scenarios – they fell away pretty quickly.
‘I do remember a conversation with Michael Barber, the head of the Prime Minister’s Delivery Unit, asking, how do I get from one scenario to another? What would the target be? And our answer was well… we can’t really tell you that. We had the Wanless model, and people were asking shall we maintain it – keep it up to date? – which would have been a lot of work. But there were no requests, and there was no interest from policy leads and politicians in that. So it just stopped. The interest was all about waiting times and foundation trusts and the tariff, and all that delivery agenda.
‘I would not want to damn the report with faint praise. The money made an enormous difference. There was the IT programme. And there was that impact on workforce.’
Hugh Taylor says it was a missed opportunity that the public health aspects implicit in the fully engaged scenario were not pursued more vigorously in the way that the National Service Frameworks were, for example. But Taylor also says there was scepticism in the department about the scenarios. The report described broadly what they would look like, but with no real detail about how they might be achieved. ‘Furthermore I thought they looked rather naïve,’ he adds. ‘This sort of thinking is still alive and kicking, but I have never seen any convincing evidence that improving people’s health in an economically active and successful country, and integrating services much better, reduces the demand for health care and reduces its cost – or indeed that it significantly slows the rate of growth. It can certainly improve quality, but I was and remain sceptical that it reduces cost.’
And indeed, as others have said, the report got caught in the crossfire first between Alan Milburn and Gordon Brown, and then between John Reid – Milburn’s successor – and the Chancellor. And, indeed, in the steadily deteriorating relationship, with some big ups and downs on the way, between the Prime Minister and his Chancellor.
Richard Douglas, the department’s longstanding director general of finance, judges that the national IT programme would not have launched without Wanless. But, he says, it was always clear that the department was going to decide how to spend the money. ‘I remember being told that “We are very happy to use your spreadsheets to get the money, but once we have got it, we tear them up.” And a minister saying during a Spending Review that “I want you in and out of the Treasury every day. But once we have got the money I never want you to talk to them again.” It was “do anything to get the money, but then don’t tie us to anything, don’t tie us to how we spend it.”’
David Nicholson, who became chief executive of the NHS Executive within the department in September 2006, says at that time the department operated as ‘a wholly owned subsidiary of Number 10, and Wanless was seen as the Chancellor’s’. But, like others, Nicholson points out that Wanless did not contain a plan about how to achieve a fully engaged scenario. ‘There was no machinery to make it happen. Nor was it part of a conversation I ever had with a secretary of state… or indeed with Paul Corrigan [Blair’s health adviser at the time].’
But, oh boy, did the money make a difference
The impact of the spending decisions that flowed in the wake of Breakfast with Frost and Wanless were, however, profound. Carol Black, president of the Royal College of Physicians when Wanless reported, recalls ‘It was a time of real hope. It provided the money for the National Service Frameworks. Cardiology was transformed from being a speciality that really couldn’t cope because it didn’t have the equipment. Before Wanless, if you weren’t near a major teaching hospital your outcome was likely to be worse, and cardiology just blossomed as the money started flowing. Geriatrics went from being a really miserable dead subject that nobody wanted to do, to one that enabled people to study interesting neurology in the elderly because you had much better scanning and much better interventional radiology, and that led to better treatments. Across specialist medicine, we got the scopes we wanted and modern MRI scanners. All specialist medicine benefited, and we had fallen so far behind. There was a real sense of energy and of advance.’ General practice, and much else, was also re-energised.
The inputs included a rise of a third in NHS staff in England – up from 893,000 in September 2000 to 1,177,000 by September 2009. These inputs produced both outputs (more activity) and better outcomes (better results from treatment). Outcomes for a whole range of conditions improved and waiting times tumbled. To the point when in 2008 – excluding a couple of specialisms, such as spinal surgery where there was a worldwide shortage of surgeons – the NHS largely hit the 18-week target. Namely that from GP referral to diagnostics being completed and substantive treatment starting, 90% of patients should wait no longer than 18 weeks if admitted to hospital. For those not requiring admission that target was 95%. And that, of course, meant that the average (median) wait was way shorter. Around 8 weeks for those admitted and 4 weeks for those who did not require admission.
Patients were no longer regularly dying from their condition on a cardiac waiting list which, for urgent cases, no longer really existed. On the OECD’s calculation, the median wait for a hip replacement – one of the high volume waiting list procedures that had proved harder to crack – had gone from more than 7 months in 2001 once it had been decided an operation was needed (ie not counting the additional waits for an outpatient appointment and subsequent X-rays and any other diagnostics), to 78 days from the GP’s referral to the actual operation taking place. There is no easy way to compare waiting times internationally. But, taken as a whole, this looked likely to be about as good as anywhere in the world.
Furthermore, the public recognised that this was happening. In November 2001, as the interim report was published, 70% of those questioned in an Ipsos MORI poll said that the state of the NHS was the most important issue facing Britain. By 2008 that had fallen to 12%, the lowest in decades.
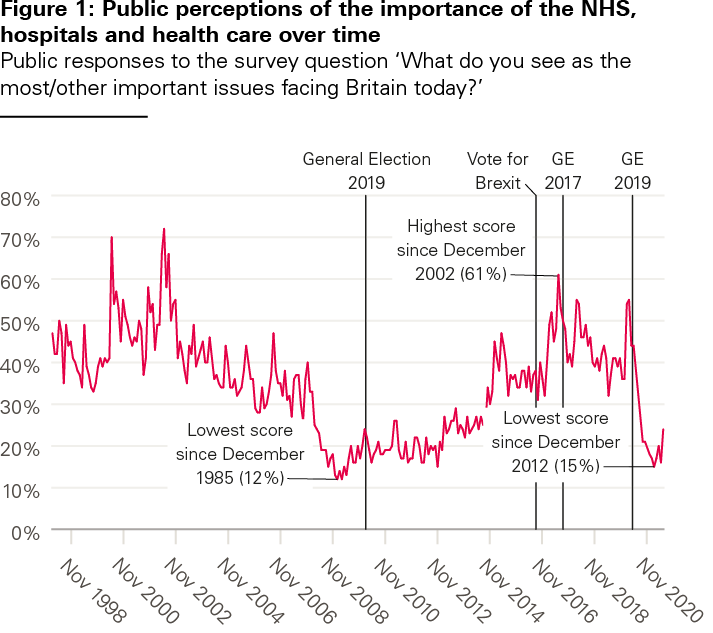
Source: Ipsos MORI. Base: representative sample of c 1,000 British adults aged 18+.
Satisfaction with the NHS, as measured by the long-running series in the British Social Attitudes Survey, was to soar. In 2001, those dissatisfied with the NHS marginally outnumbered those satisfied with it. By 2010, 70% declared themselves satisfied – a record high – and barely 20% were dissatisfied.
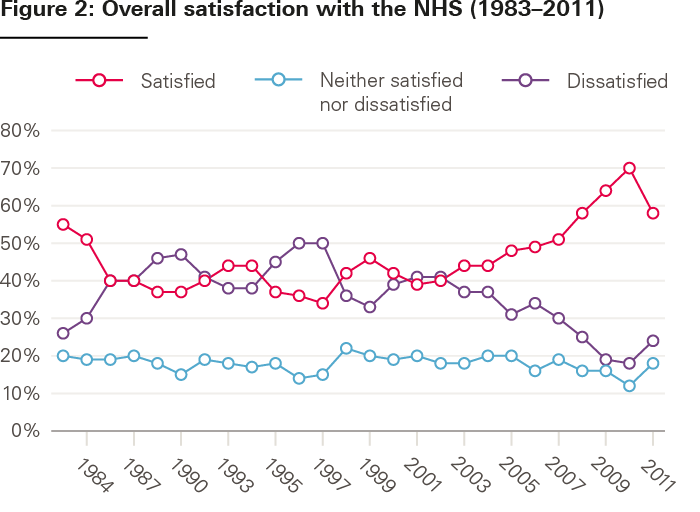
Source: British social attitudes 29; 2012.
Could the money have been better spent?
All that said, as Carol Black among others put it, while hospitals were transformed and general practice received a big investment, ‘Hand on heart, I don’t think the money was spent as well as it could have been.’ Derek Wanless’s warning proved prescient. Increases of around 7.4% in real terms over 5 years were ‘… at the upper end of what should sensibly be spent. Indeed, to be wisely spent, they already represent a very considerable management challenge’.
The troubles with the IT programme have already been mentioned. A big pay rise for NHS staff was clearly needed. But a lot of money went into pay by way of new contracts for all the staff groups, each costing much more than anticipated. To the point where, very briefly, outside of the United States both consultants and GPs became arguably the best paid doctors in the world. Steps were taken to integrate hospital, GP and community services better, but progress was limited. It was not helped by the NHS achieving the remarkable feat in 2005/06 of overspending by £570m at a time of record growth, having to take £1bn out of the next year’s budget to rebalance the books. The NHS did an awful lot more and did it better – but it tended to be more of the same. Ara Darzi, the distinguished surgeon who became a became a health minister in 2007, and whose 2008 report also argued for better integrated care, has judged that, ‘We missed the best opportunity in the history of the NHS to actually reform it… we just threw money at it.’
That has led to debate about whether the service might have been better served by a slower rate of growth – say 7 years of 5% a year real terms increases, rather than 5 years of 7%. That is certainly the view of Adair Turner. Alan Milburn concedes, ‘The system found it difficult to manage the sudden increase in resources after years of drought. So I think that is a reasonable critique to make. I have mixed views about it.’
As do others. There is an argument that a longer, slower rate of growth might have seen the money better spent. But politically, it was never going to happen. 5 years of 7% in real terms took Labour to 2007/8 – beyond the next election, but an election it looked to have a reasonable chance of winning (as indeed it did). Anything longer felt as though it stretched too far out into the distance, and Labour wanted results. Furthermore, as Richard Murray puts it: ‘If you are a spending department and it is jam today or jam tomorrow… well jam tomorrow never arrives. “I want this frontloaded so I have got it in my pocket.” If it is backloaded the fear, and too often the reality, is that it never arrives.’
The view of Richard Douglas, the head of finance, on whether slower, longer growth would have been better is that: ‘It is quite hard to say. There was this incredibly naïve belief, which I shared, which was that if you only had the money you could do anything. And there just wasn’t the management bandwidth, either nationally or locally.
‘If you are trying to change the structure of the NHS, bringing in foundation trusts, bringing the independent sector in, doing the biggest PFI programme we’d ever done, changing the contracts of all your staff, trying to get at least some better integration, doing the national programme for IT… trying to do all that stuff at once was absolutely insane, however much money you have got.
‘If it had been 5% over 7 [years] rather than 7% over 5 , would we have tried to do anything different? No, probably not. We would probably have tried to do all that stuff and would probably have failed in a similar way, with an even higher level of optimism bias!’
On public health
Securing our future health was not the last of the Derek Wanless commissions from government. In 2004 he produced a further study for the Treasury: Securing good health for the whole population, looking at what needed to happen to public health if the fully engaged scenario from the 2002 report was to be achieved.
This subsequent review also started out with something of a row, according to Alan Milburn. ‘The original terms of reference were not about public health at all. They were about trying to improve efficiency within the NHS. Which was entirely, of course, an attempt to land grab the implementation/operational agenda from the department. I saw the terms of reference and I went ballistic. With Gordon directly, and more generally with the Prime Minister. And we vetoed that. Simon Stevens, who was at Number 10 by this stage, was instrumental in rewriting the terms of reference so that it became about public health, not about the system.’
Over 185 pages, plus annexes, the public health report came up with 21 recommendations. These called for much better cost/benefit analysis of public health programmes; targets for the reduction of smoking, alcohol consumption and obesity; better understanding of what motivates the public to accept or reject healthier styles; improved evaluation of public health programmes once up and running; some restructuring of the arm’s-length bodies involved in public health – and the potentially rather more controversial recommendation that ‘The right of the individual to choose their own lifestyle must be balanced against any adverse impacts those choices have on the quality of life of others.’
The report has a lengthy chapter on the wider determinants of health that are beyond the reach of the NHS – income, education, housing and other elements of the broader social and economic environment. It cites developments following on from the Black report of 1980 and the more recent Acheson report of 1998, which was within Labour’s time, both of which focus on the wider determinants. It notes initiatives taken by the Labour government, in part as a limited response to the (very expensive) Acheson proposals. These included the introduction of Sure Start, and measures to reduce unemployment, pensioner poverty and the number of children killed on roads. But its focus is much more around what might be dubbed ‘classic’ public health issues, such as smoking and obesity. And unlike Black and Acheson, it does not propose specific new measures to tackle the wider determinants. It was followed by a white paper on public health – subtitled Making healthy choices easier – in November 2004. That led, among other things, to the ban on smoking in public places in England (Scotland having already pioneered it), along with improved food labelling to help consumers make healthier choices.
The fact is, however, that for many but not all of our interviewees, the public health report had almost entirely faded from memory. It still resonated most strongly, and unsurprisingly, with those who had a public health background – or who went on to work in the field.
Sian Griffiths, president of the Faculty of Public Health at the time of publication, remembers spending many hours with Wanless working on the report. ‘The public health community,’ she says, was, at the time, ‘a bit of a shambles’ and needed a review of its work. There was also the attraction that the fully engaged scenario was ‘a public health agenda, not just a health service one. That you needed to think about the economic determinants of health, and about reducing health inequalities’.
When the report was published, Griffiths welcomed it in the British Medical Journal as a ‘once in a lifetime chance’ for public health ‘to be taken seriously, not seen as a bit of froth on the side. We have to use this report to engage not just those of us who are enthusiastic about public health but a far wider audience’. But she acknowledges that others, in the same BMJ piece, were more critical, arguing that it was short of details on how the changes were to be achieved. Looking back, Griffiths says, the fully engaged scenario was always ‘more of a mantra than a programme… You needed to win hearts and minds, and there was not a lot on how to do that. But it did push public health up the agenda to another level and got the attention of the Treasury, which it had not really had before.
‘But public health then got a bit fractured in the big reorganisation of primary care trusts that subsequently happened. And it got a bit lost in the choice agenda and in the public/private partnerships that were being used to drive activity in the acute sector.’
Sally Davies, who was radically revamping the NHS’s research and development programme at the time of Wanless and would serve as chief medical officer from 2010 to 2019, says, ‘I think it really woke the health community up. The sense that, if we get the engagement, we will get a return on our investment. When I look again at the 2004 report, so many of the recommendations that I made in my annual reports [around tackling excess alcohol consumption, obesity and junk food for example] he made first. If I had realised I would have attributed it to him […] So I think he shaped much more subliminally than we give him credit for. It kind of went into our inner brain, and it is interesting how much many of us have since been basing on it, but not recognising it.’
By contrast, in the annual reports of Liam Donaldson, the chief medical officer at the time of Wanless, there is merely a passing reference in 2003 to the original Wanless report. And only then to the extent that it ‘… has also emphasised the importance of better population health and prevention of disease to the sustainability of the health service in the future’. But there are no further references either to the original report or, perhaps more remarkably, the subsequent public health one in Donaldson’s succeeding reports which run up to 2009, although he does reference Wanless’s work elsewhere.
On social care
Derek Wanless’s other contribution was a 2006 study on the future funding of social care, commissioned by The King’s Fund – once it became clear the Treasury was not going to ask him. A comprehensive piece of work, the report went through the myriad funding options, concluding that there was no such thing as a perfect system, while coming down ‘on balance’ in favour of a partnership model involving contributions from both individuals and the state. A full reform of the funding of social care is, of course, still awaited.
In addition, Wanless advised on a review of health and social care for the Welsh assembly published in 2003. But as with any detailed account of his social care report, that falls outside the scope of this study.
Legacy version one: ‘The memory lingers on’
As with the origins of the Wanless review, there are essentially two views of its longer term legacy for the UK. One can be seen as somewhat dispiriting. The other, for those who believe in the NHS model, is much more positive – if essentially political. We start with the more dispiriting view of its UK legacy. But it is first worth noting some international impact.
As already noted, the OECD had been putting more emphasis on the outcomes achieved by health spending: its analysis having, for example, shown the NHS was coming up short. But ‘the Wanless report definitely put wind in those sails,’ according to Mark Pearson, for a long-time head of the OECD’s health division. No country directly copied the Wanless exercise, Pearson says. But. ‘The UK had a leading voice in health discussion globally at the time. It did encourage people to move away from debates about “What is the latest on co-payments?” to “Why are our health systems not delivering?”, and to more talk about effectiveness and outcomes. Some of what happened afterwards also had an impact, almost as a cautionary tale. A lot more money was going into health in other countries at the time. But what the UK did in terms of pay and conditions – the new contracts in particular, with too much extra pay without enough in return in terms of changed work practices – that had a very big effect on many countries. They talked about what not to do, as well as what to do.’
The money in the medium term
The Wanless review provided the justification – as it was designed to – for the huge spending increases, and for the National Insurance increase needed to pay for those. There is an argument that the money could have been better spent. But there is no doubt that the money made a profound difference to the quality and accessibility of NHS services.
To that extent, the Wanless review can be seen as one of the most important documents in the history of the NHS – even if, as Milburn and others including this author believe, huge increases would have had to flow anyway from Tony Blair’s commitment as Prime Minister on Breakfast with Frost. The medium-term picture is more nuanced. The money was meant to be the first tranche in a 20-year programme. Derek Wanless’s recommendation that the whole exercise be repeated every 5 years or so was not followed up, nor his recommendation that social care should be subject to a similar analysis and included in future reviews.
One of the reasons a 5-year follow up did not happen was that after the 2005 election, Tony Blair was under growing pressure to go, with Brown ever more forcefully pushing to take over. ‘There were two problems,’ Nick Macpherson says. ‘One was that the fiscal situation was more of a constraint. But the real blow was the 2-year period after the 2005 election when Mr Brown was waiting for Tony Blair to go. Blair was busy thinking about his legacy. There was not, by then, an appetite for another big round of tax increases, and the period 2005 to 2007 was in my view an opportunity missed. Because Brown did want not to do anything to rock the boat, but he also did not want to do anything that could be used by Blair to promote his legacy. And then Northern Rock took place at the end of 2007…’ (The collapse of Northern Rock being the first UK sign of the global financial crash to come in 2008.)
Had the exercise been repeated, the forward projections of necessary expenditure would no doubt have been revised. But under the fully engaged scenario from 2002, spending would have continued to rise from 2007 by 4.4% in real terms out to 2012, and by 4.7% if the NHS and health care more generally was making solid progress. The 2007 Spending Review does reference the Wanless report at some length, while delivering promised increases of 4% in real terms out to 2010/11 (see also Box 4). This was, as was then standard, a 3-year Spending Review rather than another 5-year award. Local authorities, who commission social care, were treated much less generously, receiving a 1% per annum real increase. The Spending Review also promised a green paper on the options for social care funding reform, referencing among others, Wanless’s report for The King’s Fund. So, within government, the memory of Wanless did linger on, but without anything substantive being done to pursue its longer term funding approach.
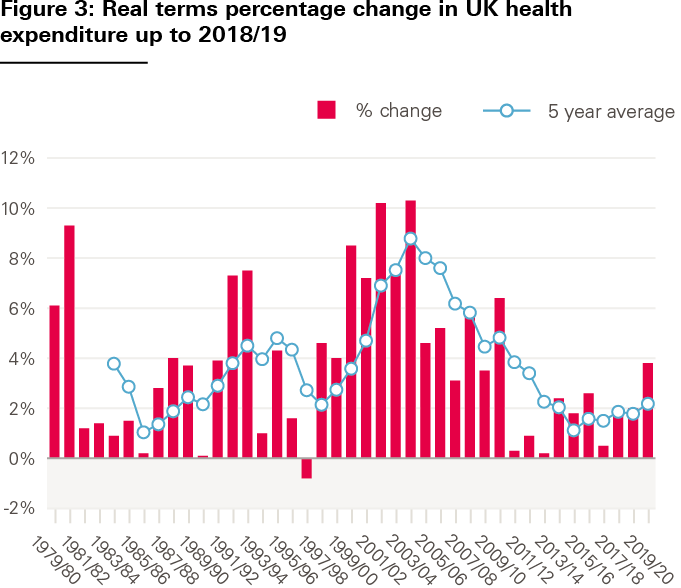
Source: House of Commons Library briefing paper. NHS funding and expenditure; 17 January 2019 (https://researchbriefings.files.parliament.uk/documents/SN00724/SN00724.pdf).
The second 5 years of generous funding, as envisaged in the report, was not delivered in full. The global financial crash of 2008 was to usher in, from 2010, the better part of a decade of austerity. The NHS, while faring better than all other public services, still saw historically low rates of expenditure increase.
Box 4: Expenditure
It is beyond the purpose of this study to analyse in any detail what has happened to health expenditure following the projections in the Wanless report. But it would be incomplete without a glance at what has happened.
Table 1 compares Wanless’s three scenarios against actual data across a range of health spending measures. Note, we make no attempt here to incorporate recent spending on COVID-19, even in projections. This is both because this does not yet feature in the relevant data series, but more importantly such emergency spending would obscure any comparisons.
Table 1: UK health spending – Wanless vs actual/projected
|
2007/08 |
2012/13 |
2017/18 |
2022/23 |
||
|
(1) Solid progress |
7.7 |
9.4 |
10.5 |
10.9 |
11.1 |
|
(2) Slow uptake |
7.7 |
9.5 |
11.0 |
11.9 |
12.5 |
|
(3) Fully engaged |
7.7 |
9.4 |
10.3 |
10.6 |
10.6 |
|
Actual |
8.1 |
9.0 |
10.1 |
9.9 |
n/a |
|
Difference vs (1) |
0.4 |
-0.4 |
-0.4 |
-1.1 |
n/a |
|
2007/08 |
2012/13 |
2017/18 |
2022/23 |
||
|
Wanless |
|||||
|
(1) Solid progress |
6.5 |
8.2 |
9.3 |
9.7 |
9.9 |
|
(2) Slow uptake |
6.5 |
8.3 |
9.8 |
10.7 |
11.3 |
|
(3) Fully engaged |
6.5 |
8.2 |
9.1 |
9.4 |
9.4 |
|
6.2 |
7.2 |
8.1 |
7.7 |
8.3 |
|
|
Difference vs (1) |
-0.3 |
-1.0 |
-1.2 |
-2.0 |
-1.6 |
|
Wanless |
|||||
|
(1) Solid progress |
96 |
135 |
170 |
199 |
227 |
|
(2) Slow uptake |
96 |
137 |
179 |
218 |
259 |
|
(3) Fully engaged |
96 |
135 |
168 |
193 |
217 |
|
Actual/projection |
93 |
126 |
140 |
153 |
178 |
|
Difference vs (1) |
-2.5 |
-9.7 |
-30.0 |
-45.3 |
-48.5 |
|
Wanless |
|||||
|
(1) Solid progress |
6.8 |
7.1 |
4.7 |
3.1 |
2.7 |
|
(2) Slow uptake |
6.8 |
7.3 |
5.6 |
4.0 |
3.5 |
|
(3) Fully engaged |
6.8 |
7.1 |
4.4 |
2.8 |
2.4 |
|
Actual/projection |
6.7 |
6.1 |
2.3 |
1.8 |
3.4 |
|
Difference vs (1) |
-0.1 |
-1.0 |
-2.4 |
-1.3 |
0.7 |
Direct comparisons are not easy. There are discrepancies in the base year (2002/03) – Wanless figures for that year were estimates and public health spending came in slightly lower than expected. In addition, more complete data are now available from the ONS to describe all health spending, including a breakdown of private and other spending. These factors help explain the higher total health spending figure for 2002/03.
The pattern, however, is clear. Growth in health spending quickly fell short of all Wanless’s projections. As Figure 4 shows, the shortfall accelerated after 2008/09, such that by 2017/18 a £45bn gap had opened between annual spending and that projected under the solid progress scenario – a 22% shortfall. This illustrates how, despite health continuing to receive modest real-terms increases after the financial crash, a near-decade of austerity took its toll. Even now, increases in line with the NHS England settlement (our projected values for 2022/23) will do little to close that gap.
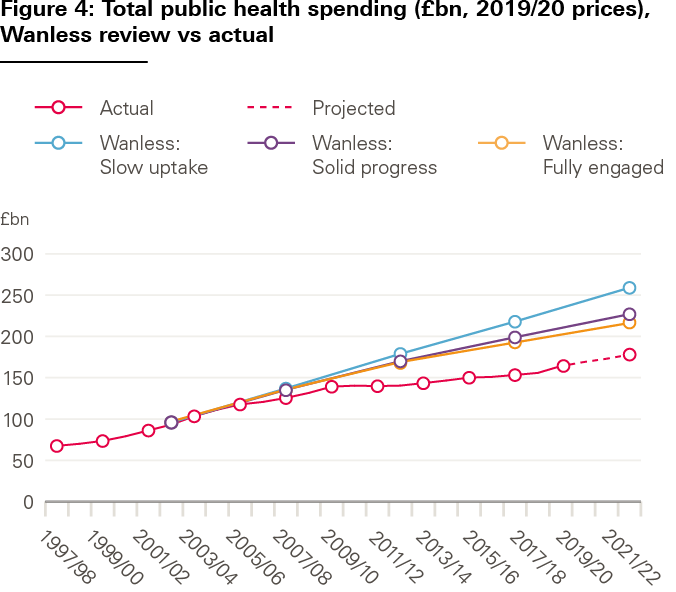
The broader legacy
For some – including Anita Charlesworth – a rereading of the main Wanless report on funding is, as she puts it, ‘a slightly depressing exercise’. Wanless does not use the precise phrase ‘integrated care’, although it clearly is talking about that when it refers repeatedly to a ‘whole systems’ approach to health and social care. It says much better IT is needed, and much better workforce planning, while the public health report underlines the need for healthier lifestyles and improved prevention. ‘When I reread it,’ Charlesworth says, ‘I have the mixed feeling of “Gosh, I am quite proud of that,” and then I am really quite depressed about how much of it you could still write today.
‘There was not some big reaction against what it was saying,’ she says. ‘It had, certainly among the public health community and the clinical community, an awful lot of support. And I still get invited to speak to people now about it. So it is kind of weird that something that could not have had a better following wind led to so little progress.’
Likewise Nigel Crisp, chief executive of the NHS and permanent secretary at the Department of Health at the time of Wanless, says: ‘I am very depressed. It was a fundamentally sound piece of work. But we are still hung up with 20th century health care systems. Why has more progress not been made? In terms of the NHS it took the money and concentrated on its priorities. “Thank you Wanless, and goodbye,” is more or less what happened.
‘We did try to return to it, around 2005, shifting the focus from targets to health. But we didn’t put the energy behind what was then called the patient empowerment agenda that we had put behind the service improvement agenda.’ In some ways, Crisp says, the timing was wrong for the report’s broader health agenda. ‘The right time to do something about it was when we had beaten the waiting lists into submission. What everyone wanted at the time – and I include myself and the public in this – was to get waiting lists down and to stop people dying on the cardiac waiting list.’
Paul Corrigan, who in 2005 moved from the health department to be Tony Blair’s senior health adviser, says: ‘I remember reading the report with this idea of the fully engaged scenario and thinking this could be really important, but then just going back to the choice and competition agenda and getting on with it. To be fair, we were really, really, busy implementing a whole bunch of things designed to make the NHS work better.
‘If we had engaged with it, I am not sure we would have known, back then, quite how to do it. We do know now, for example, that if people with diabetes do more self-management that it is both better for their health and cheaper. And, while this comment is slightly ridiculous, if the report had not just talked about the fully engaged scenario, but had said “Here are 10 different thoughts I’ve had about how we might do that,” while asking “How are choice and competition doing to do that?”, we might have got to the issue of long-term conditions and better integration much sooner. But that is our fault, not his. By 2005 we were, with Patricia Hewitt, starting to talk about long-term conditions and better integrated care.’
As already noted, a public health white paper did follow the public health report, and in 2005, in Patricia Hewitt’s day as health secretary, a large public engagement exercise was launched. This concluded in a 1,000-strong ‘Citizens Summit’ that led to Our health, our care, our say. That white paper continued to put a strong emphasis on patient choice. It addresses the need to concentrate tertiary services in fewer hospitals, while moving others out of district general hospitals and closer to home. But it also refers extensively to integrated health and social care. ‘Far more services will be delivered – safely and effectively – in settings closer to home; people will have real choices in both primary care and social care; and services will be integrated and built round the needs of individuals and not service providers,’ it says, to quote just one example.
Patricia Hewitt says: ‘I thought the device of the fully engaged scenario was absolutely spot on. And it remains true today. Public health was part of that, and we did make commitments on public health. We already knew we had to do more on prevention, and Wanless strengthened that. We also saw some emerging partnerships between local councils and the go-ahead primary care trusts who did really good work on prevention locally. And we did put a lot of effort into Our health, our care, our say.’
But while the fully engaged scenario was, Hewitt says, ‘… an interesting analysis, and we all agreed with it, sadly, in the end, it got put on the shelf. The service demands of the NHS itself were just so inexorable.’
Part of the issue may have been, as Corrigan hints, that while the original report made plenty of recommendations around what the fully engaged scenario would look like, it had nothing substantive to say about how it might be achieved. Essentially the three scenarios were concepts, the ‘how to get to them’ remaining in the province of the Department of Health.
Furthermore, the challenge of assessing the scenarios is shown in work that Derek Wanless himself undertook, again with The King’s Fund, in 2007. In the absence of a further government-commissioned review, Our future health secured? sought to assess progress since 2002, although for much of the performance data it had to rely on 2005/6 figures, and occasionally from 2004. The report does not present an overall conclusion. But on key elements of the service – input costs, IT, services delivered, population health and productivity, for example – it puts progress at somewhere between slow uptake and solid progress, at times veering more towards one than the other. But what is clear from the report is that these are – indeed had to be – perceptions, rather than judgements made on predetermined metrics. The three scenarios remained, essentially, concepts.
There are other circles where the memory lingers on. Norman Lamb, the Liberal Democrat health minister between 2012 and 2015, says he regularly referenced it in opposition up to 2010. And when he stepped out of line as a health minister in 2014 to call for an immediate cash injection for the NHS, ‘I am not sure whether I referenced the Wanless report, but it was in my mind.’ Likewise, Lamb says, when again in opposition after 2015, he referenced its work as he sought with others to build a cross-party consensus for a long-term settlement for the NHS. But against this, aside from the attention paid immediately after the main report’s publication, Wanless did not cut through with the general public in the way of the Beveridge report, or the Turner pensions commission report – although, in fairness, few such reviews do.
Looking back from today’s vantage point, almost 20 years on, it is possible to take a rosier, if mixed view, rather than an entirely depressing one. The impact of the money – whether you believe that stemmed from Breakfast with Frost or Wanless – has already been discussed. The picture on public health is nuanced. Some trends have headed in the right direction – smoking and drinking among younger people, for example. But health inequalities have widened, and since 2010 past increases in life expectancy at birth appear to have stalled. Even so, public health is better than it was in 2004. On IT, the NHS still lacks a fully integrated electronic patient record, but the use of IT within the NHS is appreciably better than it was. There is, at the time of writing, the glaring absence of a long overdue workforce plan for either health or social care, but on the plus side the drive towards integrated care systems does appear to be making some progress – although a fuller analysis of how they are doing is beyond the scope of this report.
Mark Pearson from the OECD agrees that there is a long way to go on two of the review’s key themes – IT and integrated care. But he notes that while there are good examples of both within various health systems around the world, ‘I am not sure that any country has made really good progress. The UK is not alone. These are quite difficult things to do.’
Furthermore, someone being generous could, on better integrated care, draw a line of inheritance that stretches through Patricia Hewitt’s Our health, our care, our say (2006), on to parts of Ara Darzi’s High quality health for all (2008), on in turn to David Nicholson’s Call to action (2013), culminating in Simon Stevens’s Five year forward view (2014) and the subsequent documents that have led to the drive for integrated care systems.
There is, however, another way entirely of looking at the legacy of the Wanless report.
Legacy version two: ‘It’s the politics, stupid’
The other version lies in the view of Ed Balls who says, ‘When I think back on my time in politics it is, I think, the thing that I am most proud of. You have a left of centre government that set out to make the case for a tax rise. Not because it had screwed things up, but in order to spend more on a key public service at a time when the main opposition party is trying to undermine – in fact to destroy – the post-war consensus about the National Health Service being the best funding model.
‘The strategy is, you can make the NHS perform much better but it needs to be properly resourced. So we have this twin track. Derek does a report which is well received. It is absolutely the platform for the National Insurance increase to deliver the longest, most sustained increase in national health spending in the history of British health policy.
‘And that in turn delivers enormous improvements in health outcomes, in terms of waits and a lot of other things as well. There is an absolutely legitimate debate about whether the money was spent as well as it could have been. But that is a second order question.
‘Look at the 2005 election. If you go back to the Conservative’s statements on the day Wanless reported, you would think the report would be at the centre of a massive row – in which the betrayal of the economy, through this terrible tax rise from a Labour party that always wanted to raise taxes, and then wasted the money, would be central to the election campaign. Nothing.
‘The Tories still clung to the patient passport in 2005. But they were not saying that Wanless was wrong. That we should not be spending all this money on health. That they would reverse the tax rise. They did not because it was hugely supported in all the opinion polls. So in the 2005 election, the most controversial thing we had done in tax and spending policy is barely mentioned. Because we have massively won the argument for a tax rise to improve the health service with Derek’s report at its centre.
‘It was a triumph of public policy and politics. In 2005 Michael Howard [Conservative party leader] found he could not fight the election on “The NHS is a failed model” and by the time you get to David Cameron in 2010, he is telling the public that he can do his priorities in three letters – N-H-S – and that “I will cut the deficit, not the NHS.” That was the biggest tribute to Wanless and to Anita and everything we did.
‘It transformed the whole debate about the National Health Service. You have to go back to the bitterness of the autumn of 2001 to see quite what a journey has happened. When I think back on reviews I have been involved in, and I have been involved in some really good ones over the years, the Wanless review is by far the most politically significant with the longest lasting effects.’
Nick Macpherson concurs, at least on the tax raising point. With 30 years’ experience at the Treasury behind him, it is, he says, ‘The only serious, discretionary, non-forced tax increase in my life. All the other ones were forced. So it was a political achievement.’
‡‡‡‡‡ These assessments come at different stages of the programme. But see eg, The National Programme for IT in the NHS: Progress since 2006, Commons Public Accounts Committee, January 2009; The National Programme for IT in the NHS: an update on the delivery of detailed care records systems, National Audit Office, May 2011.
§§§§§ As they did in other countries. The UK’s performance in terms of outcomes lagged and still lags some other countries on some measures.
¶¶¶¶¶ HM Treasury analysis was that only in the US were doctors paid more on average. For nurses only those in the US and Australia were better paid. See Treasury stalls on pay rises in the NHS, Financial Times 17 March 2006. For salaried doctors see OECD Health Data 2007 (www.oecd.org/newsroom/38976572.pdf). The BMA conceded in its evidence to the DDRB in 2006 that earnings were ‘broadly comparable with their compatriots in other countries’ (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/273263/6733.pdf) (para 2.29).
****** For figures see 17th Report of the Commons Public Accounts Committee; February 2007 (https://publications.parliament.uk/pa/cm200607/cmselect/cmpubacc/361/36103.htm) and The five giants, ibid, (pp 635–639) for a fuller account of cause and effect.
†††††† 2002/03 figures in Wanless are estimates.
‡‡‡‡‡‡ Source: ONS, Healthcare expenditure, UK Health Accounts: 2018 (2020). Data are reported according to system of health accounts (SHA). Financial years are calculated pro-rata from calendar years.
§§§§§§ Wanless figures all include an assumed constant of 1.2% for private sector health spending.
¶¶¶¶¶¶ 2002/03 figures in Wanless are estimates.
******* Source: ONS, Healthcare expenditure, UK Health Accounts: 2018 (2020). Data are reported according to system of health accounts (SHA). Financial years are calculated pro-rata from calendar years.
††††††† Health spend defined as government-financed only. Wanless figures are all minus 1.2%.
‡‡‡‡‡‡‡ We have estimated future total health spending using the real-terms growth from the NHS funding settlement (3.4% per year) as a basis for DHSC health spending only. Other aspects of health spending from SHA assumed stable as proportion of GDP. GDP deflator from HMT (2020).
§§§§§§§ Source: HMT, Public Expenditure Spending Analysis (PESA), public sector expenditure on services by function. Actual data up to 2019/20.
¶¶¶¶¶¶¶ Source: Growth figures are annual averages for the 5 years up to that date (Wanless figures are for 4 years in the period up to 2002/03).
Conclusion and coda
Conclusion
What was the Wanless report about? That was the opening question put to the interviewees for this study. And, as has become clear, the answers are many.
It was indeed a ‘His Master’s Voice’ report, commissioned by the Chancellor to produce the outcome he wanted, as Andrew Turnbull, permanent secretary at the Treasury at the time of the Wanless reviews, dubbed it. But to see it only as that is to do it an injustice. Within its terms of reference, it was an independent review. Witness not least Wanless’s re-raising of the issue of social care at a time when the government had only recently made a controversial decision to do little about it.
The Wanless report was both a product, and in some ways a victim, of the politics of the day. A product of the internal tensions within the Labour government, Blair having promised to raise spending to the EU average with Brown seeking to wrest back control – but with Blair and Milburn determined that reform of the management of the service would be theirs. But seeing the report only in these terms would also be an injustice.
At the time the NHS model was under attack from longstanding opponents, but was also subject to continuing worries that it might not be sustainable even among some of its natural supporters. It was also the case that the Conservative party’s formal position was that the NHS was a failing model and that the answer was to inject higher private spending. Thus the argument presented here by Ed Balls has weight – that, at least from the Treasury’s point of view, a Labour government had not only to make the case for additional sustained increases in NHS expenditure, but also the case for a tax rise to pay for it. It did, as Nick Macpherson observes, lead to the only serious, non-forced, discretionary tax rise since at least 1979 – and one that proved electorally appealing.
The least generous view has to be that it was, at a minimum, a stepping stone to a predetermined shore: the big increases in NHS spending that Tony Blair had promised.
But regardless of whether the increases are viewed as inevitable (given Blair’s promise) or as the product of the review, the money that flowed into the NHS made a real difference. If there is a case that the Griffiths management review of 1983 rescued the NHS, there is equally a case that the money rescued an NHS that was in fact failing – falling behind international standards and leaving dissatisfied large elements of the public, whose support as taxpayers was crucial. By the end of the spending periods that the Wanless report affected, public satisfaction with the NHS was to reach a record high.
None of what might be dubbed the report’s key operational themes were new. What we now call ‘integrated care’ had sailed under various banners beforehand – coordinated working, inter-agency working, managed care – and, indeed, as far back as 1974, that year’s mighty NHS reorganisation was intended to make hospital services, community services and primary care work better together. There had been an understanding for some time that the power of computing – already widespread in GP practices – needed to be harnessed to deliver not just better data (which has happened) but a fully interchangeable electronic patient record (which remains a long way from completion). Indeed a £1bn 7-year initiative to achieve that had been launched in 1998., The absence of proper workforce planning had become a recognised problem, not least since the abolition of the Regional Health Authorities in 1996. But the Wanless report underlined each of these and put fresh energy into them all. Even if the national IT programme proved anything but a huge success, workforce planning has gone missing again, and social care remains a problem to be solved.
As to why the report did not have the wider or more lasting impact that many wished for it, four factors were in play. The first three are interrelated. First, it was both a product and to some extent a victim of the Blair/Brown tensions. The Department of Health never owned it. And, perhaps most importantly, as several interviewees noted, while it provided a broad description of what fully engaged looked like, it did not provide a plan, blueprint, or route map of how to get there. To be fair, it was not asked to. But in the absence of the blueprint, the first two factors ensured that one did not get built. The fourth factor, as Patricia Hewitt puts it, was that ‘The service demands of the NHS itself were just so inexorable.’ The primary focus – rightly at the time – was on waiting times, compounded in the short term by the need to tackle the NHS overspend (which was not, it must be said, Patricia Hewitt’s fault).
For those who want to take a more optimistic view of its impact, a line can be drawn, as already noted, from the Wanless report’s call for better integrated care through subsequent initiatives and on to the integrated care systems of today.
Most importantly, however, the Wanless report was the only serious attempt by any government since 1948 to make an independent assessment of the NHS’s likely future needs, and likely cost, over the next 20 years. That alone makes it a landmark report. An exercise that, for all the very real difficulties in forecasting medical advances and other changes over such a long timescale, has to be worth repeating. Not least because the data available to do this are so much better now than they were at the time.
Coda
1: Could it be done better next time?
If there were to be a Wanless-type exercise at another time, could it be done better? There is no easy answer to that question.
In 2018 the Institute for Government, with support from the Health Foundation, looked at the many ways governments have sought to use inquiries to solve knotty public policy problems, though with varying degrees of the success. The methods range from Royal Commissions to various other types of independent inquiry. The 20 case studies it examined included the Beveridge report, the Low Pay Commission, the Pensions Commission, the Dearing and Browne reviews of higher education funding, the Armitt review that produced the Infrastructure Commission, the Dilnot inquiry into social care and the Committee on Climate Change.
Among the study’s key conclusions relevant to a Wanless-type exercise were that to be successful, at a minimum, such inquiries need the full support of the Prime Minister and Chancellor. In addition, inquiries often seem to work best when they publish an interim report that prepares the ground ahead of final conclusions. By the time Wanless reported, it met those criteria.
The fact that it was a Treasury-led review, however, proved to be both a strength and a weakness. The strength was that this was the Treasury untying its own purse strings, rather than an outside body persuading it so to do. The weakness was the ownership. The Department of Health provided much key statistical support and indeed had its own civil servant working on the review team. So to that extent it was shared. But all the department really wanted was the money. It never owned the review in any wider sense, and Labour’s internal party politics meant that once the money was delivered, health ministers and the department were never likely to own its other recommendations, apart from where they already fitted with the department’s own agenda. As Nick Macpherson puts it: ‘You want departmental ownership. The only way anything really happens is that the department really owns something.’
It is on occasion possible to reverse engineer a Treasury review into the heart of departmental policy. For example, the Treasury-led 1997/98 Review of services for young children resulted in the Sure Start programme, where large amounts of Treasury cash became married to the objectives of successive education secretaries, backed up by a cross-departmental Cabinet committee. This ensured that the Department of Health and others played their part. The slow burn effect of the Committee on Climate Change is another example, as is the Treasury inspired creation of welfare-to-work programmes, again in Gordon Brown’s day. It is not possible to legislate such ownership. It is a product of the internal politics of the government of the day.
Given this, there were few suggestions from our interviewees about how the Wanless report could have been given a greater impact than it had. The main suggestion was to do something rather different. Not so much for government to repeat the exercise but to set up a standing review of likely future health and social care costs, undertaken either by the Office for Budget Responsibility (OBR), or an equivalent body.
Chris Ham, who ‘lived and breathed the review by proxy’ as head of the department’s strategy unit says: ‘It would really only have had a lasting impact if you had institutionalised the Wanless process. Effectively, it was a one-off. So long as Blair and Brown were around, the commitment was there. If it is not institutionalised, then with a change of government, or just a change of Prime Minister or Chancellor, there is always the risk it will go in another direction.
‘It might have been more sensible to have an OBR-type arrangement that would be charged with doing it on a regular basis. I am not sure that doing it again 5 or 10 years later would have been sufficient.’
Nick Macpherson likewise judges that such an arrangement could work – but work best if there was some form of soft hypothecation – some form of earmarked tax – for health and social care, and if the UK sticks with fixed-term parliaments. That, he says, ‘… would create clarity about the medium-term pressures on health and social care, to better inform a debate about funding. We have defence reviews as a matter of course to ask what do we want to fund our armed forces for? There is a genuine advantage in reasonably transparent reviews of pressures that better inform funding, but which also debate what the state should be doing, and whether there should be changes in the way the state delivers things. I think that has a wider application, beyond health.’
The Treasury, Macpherson says, will always be worried that such an approach would become a permanent source of even greater pressure on it to ‘reconcile the irreconcilable’. ‘But I think, just as the OBR has created better decision making, so should a better quality, better informed set of projections on health and social care. The lesson of Wanless is that getting things out into the open, ensuring that there is some debate, is likely to improve the quality of decisions.’
Hugh Taylor, who was permanent secretary at the Department of Health between 2006 and 2010, says that if there were to be another Wanless ‘The one additional thing I would like it to do is make the economic case for health spending. Not just in the sense that if you have a healthier population you keep people in work and reduce benefits, but the investment it brings in science and technology and the life sciences. When push comes to shove, the Treasury always treats the NHS as an overhead, not as a key area of wealth generation. But two of the unique selling points of the UK ought to be the excellence of its universities and the capability of the NHS, which has access to patients and data in ways that make doing the science easier.
‘To be fair, when I was in government, the Treasury was incredibly supportive of the R&D agenda. But at the simplest level, the NHS employs a lot of scientists, it does a lot of construction work, and it plays right at the edge of technological change in almost every dimension you can think of. Part of the economic success of the state is the spending on health, which in turn has given pharmaceutical companies, and potentially the wider life sciences industry, a hugely strong base in the UK. There is a strong economic case for investing in the NHS, and it needs to be better understood.’
Medical advances
It is clear that one of the biggest challenges in such an exercise is predicting scientific and medical advances – over 5 years let alone 20. And then assessing which, if any, are likely to have a significant impact on the overall cost of health care.
As already noted (see Box 2), the Wanless report, entirely forgivably, failed to spot the impact of the rise of interventional radiology on cardiac surgery, or the NHS’s much greater adoption of talking therapies (such as CBT), both of which happened within 5 years of the final report. Both clearly affected the shape of the workforce that would be needed. The former clearly improved productivity as well as clinical outcomes. The latter is judged to be cost-effective in comparison to other treatments for certain conditions. Neither, of course, was of sufficient scale to alter the quantum of funding increases that Wanless recommended.
A combination of many such things, however, might well affect productivity significantly. And productivity is an element that needs to be assessed in judging the scale of future spending increases likely to be needed.
Take a couple of examples from well before the Wanless report. The arrival of more modern anaesthetics and of laparoscopic surgery not only improved patient outcomes but raised productivity. Both reduced the trauma that patients undergo thus allowing swifter discharge from hospital and a much faster return to normal life. It would have been mighty hard, however, to project the remarkable speed with which laparoscopic surgery came to be adopted once it was available.
Anyone producing a Wanless-type report in 2019 would, of course, recognise that gene therapies may well change the way medicine works profoundly. Whether in the longer term they will prove to be cost enhancing or cost reducing remains, however, very hard to predict., Equally, a 2019 study would have registered the potential of mRNA techniques, given that these have been studied for decades. But it would have taken remarkable foresight to predict that mRNA technology would be capable, within a year, of producing new vaccines to counter a pandemic.
The Wanless review was not short of clinical engagement. A glance at those who not merely delivered written evidence but who were met for discussion shows that (pp 129–135 of final report). But it is worth observing that despite the inherent difficulties of projecting the impact of medical advances, any future exercise should work hard to ensure that it can make the best possible judgement.
2: Lessons for a post-pandemic world
Are there lessons from the Wanless review that could apply during the COVID-19 recovery and beyond? The short answer is yes. Three stem from the report itself. But two others relate to the broader context in which the report was produced.
The three that stem from the report have already been covered – the 25-year failure to find a new settlement for social care in England; the continued absence of a fully integrated electronic patient record; and the lack, once again, of a decent attempt at some form of effective workforce planning – understanding the pressures and putting policies in place to tackle them.
The two others are capacity and bandwidth. Workforce, of course, is part of capacity. But with NHS waiting times sharply on the rise as a result of the pandemic, it is not clear that the government fully grasps the scale of the challenge of getting them back down again.
The goal of achieving the 18-week target was first announced in 2004 by John Reid, Alan Milburn’s successor as health secretary. It took 4 years for that to be reached. It took 8 years if counting, more realistically, from the NHS Plan of 2000. This had set the initial target of a maximum 3-month wait for an outpatient appointment and 6 months for subsequent inpatient treatment – goals that were well on their way to being achieved by the time of Reid’s announcement. In other words, cutting waiting times took many years to achieve. In addition, it cost many, many billions of pounds. It is close to impossible to calculate how much of the extra money went on cutting waiting times as opposed to other improvements to the service. But it is entirely clear that the cost ran into many billions.
Furthermore, the backlog this time looks likely to include many, many thousands of patients whose delayed assessment and treatment is urgent – cancer and cardiac cases, not just the hips and cataracts and similar elective procedures that made up most of the longest waits by the mid-2000s. These, while painful and/or life limiting, were by and large not life threatening. David Nicholson, who lived through that period first as a strategic health authority chief executive and then from 2006 as NHS chief executive, says, ‘It will take years and years of sustained investment to get this into any kind of order.’
It should also be underlined that the time it took in the 2000s was not for want of effort. As already noted, there were the targets themselves, the Prime Minister’s Delivery Unit driving their achievement, the introduction of the competition and choice approach which included the tariff, the arrival of the independent sector treatment centres, and the ability of patients to go to any private hospital willing to treat them at the NHS price. Quite how big a part each of these played is open to debate. But it is clear that the targets and the tariff drove up activity, and all of it was backed up by some pretty vigorous performance management. It still, however, took years and cost billions. If much shorter waiting times are once again to be achieved, the same is likely to apply.
Closely tied to the issue of capacity is the question of bandwidth. The key priority was waiting times. But as Richard Douglas underlined, alongside that, and in some cases in support of it, the Labour government undertook much else. The huge IT programme, wholesale renegotiation of staff contracts; the creation of foundation trusts and of the tariff; a massive PFI programme to build hospitals and some surgeries; greater involvement of the private sector, including the creation of independent sector treatment centres; revamping the inspectorate, first into the Healthcare Commission and then into the Care Quality Commission, while at the same time seeking better integrated services and putting the NHS through another big structural reorganisation in 2006.
After it was elected in 1997, Labour abolished GP fundholding, replacing it with an initial 481 primary care groups which morphed into primary care trusts. In 2002, Labour abolished the 95 district health authorities, replacing them with 28 strategic health authorities and 300-odd primary care trusts. In 2006, however, it reduced the number of strategic health authorities from 28 to 10 and the number of primary care trusts from 303 to 152, while at the same time seeking to develop ‘practice-based commissioning’ for GPs as a sort of watered-down version of GP fundholding. A huge amount was achieved. But there was quite simply not the bandwidth, either nationally or locally – where the management reorganisations consumed much time and effort – to achieve all of that successfully.
It was made clear at the outset that this study does not attempt anything like a full account of the management of the NHS post-Wanless. But to jump forward briefly to today: the government is promising legislation to unscramble much of the 2012 Health and Social Care Act. This involves some structural reorganisation that will itself have opportunity costs at a time when the service will still be coping with COVID-19 and the huge backlog awaiting treatment. It is also worth noting that while the 2012 Act has played out very differently to the way it was envisaged, its creation of what is now NHS England has led to a consistency of purpose in working towards better integrated health and social care for the better part of a decade. There should be no shift from that. And it could be concluded that in tackling the recovery from COVID-19, more is likely to be gained by a few clear-cut priorities than attempting everything that anyone could wish for. The phrase ‘to govern is to choose’ comes to mind.
Acknowledgements
This study would not have been possible without the time, insights, recollections and reflections of a whole string of people involved, in one way or another, with the Wanless reports. The author and the Health Foundation are immensely grateful to them all. In the above text, titles have not been used because at the time these events took place they had not (other than professorships) been awarded. We trust no one feels insulted. They are spelt out here. In alphabetical order, those who generously found time for interviews were:
Ed Balls, Dame Carol Black, Anita Charlesworth, Paul Corrigan, Lord Crisp of Eaglescliffe, Dame Sally Davies, Richard Douglas, Stephen Dunn, Professor Sian Griffiths, Sir Chris Ham, Patricia Hewitt, Robert Hill, Norman Lamb, Sir Nick Macpherson, Alan Milburn, Ed Miliband, Richard Murray, Sir David Nicholson, Mark Pearson, Sir Hugh Taylor.
Others who helped in various ways, not always consciously, either because we were able to draw on earlier relevant interviews, or who pointed us to key issues and sources, include Professor the Lord Ara Darzi, Frank Dobson, John Henderson, Rudolf Klein, Sir Alan Langlands, Ben Page of Ipsos MORI (who filleted years of opinion poll data), Clive Smee, Lord Turner of Ecchinswell, Lord Turnbull and John McTernan. Dr Liam Fox declined an invitation to be interviewed. There were others who we would also like to have interviewed but who failed to respond.
Drafts of this were read by a goodly number of the interviewees whose comments and suggestions decidedly improved it. To their absolute credit, none sought to withdraw or amend any of their quotes, other than by way of minor clarification.
At the Health Foundation thanks are due in all sorts of ways to Anita Charlesworth (whose idea this was) and to Hugh Alderwick, Jennifer Dixon, Pete Stilwell, Tim Gardner and Ruth Thorlby, while Stephen Rocks undertook the calculations and did much to draft the expenditure box. Sean Agass is, as ever, an excellent and constructive editor. Despite all this assistance, any errors of fact, interpretation or judgement remain those of the author.
******** Always assuming that a fully engaged scenario would in fact reduce the rate of growth in expenditure.
†††††††† For an account of cause and effect see The five giants, ibid, (pp 635–639).
‡‡‡‡‡‡‡‡ The OBR provides independent forecasts for the economy and for the public finances. It was created in 2010. It does already make some forecasts of likely health and social care expenditure. But not in the detail or on the scale that is presumably envisaged here.
§§§§§§§§ Macpherson favours an extended version of National Insurance.
¶¶¶¶¶¶¶¶ A draft bill proposes abolishing fixed-term parliaments.
About the author
Nicholas Timmins is the author of the award-winning The five giants: A biography of the welfare state (Williams Collins, 2017). He was a journalist for 40 years including being public policy editor of the Financial Times between 1996 and 2011. He is a senior fellow at the Institute for Government and the King’s Fund, and a Visiting Professor in Social Policy at the London School of Economics. He is also an honorary FRCP.
References
- Wanless D. Securing our future health: Taking a long-term view. Final report. HM Treasury; 2002 (www.webarchive.org.uk/wayback/en/archive/20130416040413/http://webarchive.nationalarchives.gov.uk/+/http://www.hm-treasury.gov.uk/consult_wanless_final.htm).
- Breakfast with Frost [TV broadcast]. BBC News; 16 January 2000. (Transcript: http://news.bbc.co.uk/hi/english/static/audio_video/programmes/breakfast_with_frost/transcripts/blair16.jan.txt).
- Rawnsley A. Servants of the people: The inside story of New Labour. Hamish Hamilton; 2000 (p 338).
- Smee C. Speaking truth to power. Nuffield Trust; 2005 (pp 24–25).
- Commons Hansard; 19 January 2000 (vol 342 cc 835–41).
- Budget 2000. HM Treasury; March 2000 (paragraph 5.69) (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/265498/hc346.pdf).
- The King’s Fund. How much has been spent on the NHS since 2005? The King’s Fund; 2010 (www.kingsfund.org.uk/projects/general-election-2010/money-spent-nhs).
- Department of Health. Working for patients. CM 555. HMSO; 1989.
- Timmins N. The five giants: A biography of the welfare state. William Collins; 2017 (p 387).
- NHS ‘to decline into safety net for old’. The Independent; 16 September 1995.
- Healthcare 2000. UK health and healthcare services: Challenges and policy options. Healthcare 2000; 1995.
- New B. The rationing agenda in the NHS. Rationing Agenda Group. British Medical Journal 1996; 312: 1593–1601.
- Robertson R, Appleby J, Evans H, Hemmings N. Public satisfaction with the NHS and social care in 2018. Results from the British Social Attitudes survey. The King’s Fund and Nuffield Trust; 2019 (www.kingsfund.org.uk/sites/default/files/2019-03/Public_satisfaction_with_NHS_social_care_in_2018.pdf).
- NHS chief attacks bleak prediction of future cost. The Independent; 3 November 1995.
- Department of Health. The National Health Service: A service with ambitions. Department of Health; 1996 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/259812/ambition.pdf).
- Curing the NHS. Sunday Times; 16 January 2000.
- Magic required. The Guardian; 23 January 1997.
- Comprehensive Spending Review July 1998. HM Treasury (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/260743/4011.pdf).
- Bridgewater B. Death on the waiting list for cardiac surgery. Heart 1999; 81(6) (http://dx.doi.org/10.1136/hrt.81.6.564).
- Department of Health. In-patient and out-patient waiting time statistics. Historical time series. Department of Health (https://webarchive.nationalarchives.gov.uk/20130104155640/http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalWaitingTimesandListStatistics/index.htm).
- Organisation for Economic Cooperation and Development. Economic Surveys: United Kingdom 1993–94. OECD.
- Organisation for Economic Cooperation and Development. Economic Surveys: United Kingdom 2000. OECD.
- Smee C. in Timmins N (ed.). Rejuvenate or retire? Views of the NHS at 60. Nuffield Trust; 2008 (pp 92–95) (www.nuffieldtrust.org.uk/research/rejuvenate-or-retire-views-of-the-nhs-at-60).
- Doctors attack government’s management of the NHS. Financial Times; 6 July 1999.
- Blair T. Speech to Venture Capitalists Association. London; July 6, 1999.
- Private information.
- Interview with author, Frank Dobson; January 2015.
- Interview with author, Robert Hill; June 2020.
- The five giants, ibid, (p 608).
- NHS cash pledge as report damns healthcare. Financial Times; 1 December 1999.
- Milburn hints at real-term increase in NHS spending. Financial Times; 9 December 1999.
- Blair T. A journey. Hutchinson; 2010 (p 263).
- Riddel M. Robert Winston interview. New Statesman; 17 January 2000 (www.newstatesman.com/node/150550).
- Interview with author, Robert Hill; June 2020.
- Blair, ibid, (p 264).
- Ibid, (p 265).
- Interview with author, Ed Balls; May 2020.
- Interview with author, Ed Miliband; October 2020.
- Interview with author, Nick Macpherson; May 2020.
- Blair, ibid, (p 265).
- The five giants, ibid, (p 596).
- Commons Hansard. 22 March 2000, col 983 (https://publications.parliament.uk/pa/cm199900/cmhansrd/vo000322/debtext/00322-04.htm).
- Department of Health. The NHS Plan: a plan for investment a plan for reform. 2000; (https://webarchive.nationalarchives.gov.uk/20100407193447/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002960).
- Interview with author, Anita Charlesworth; March 2020.
- Taylor M. Work incentives: A report by Martin Taylor. The modernisation of Britain’s tax and benefit system no. 2. HM Treasury; 1998.
- HM Treasury. Economic instruments and the business use of energy: a report by Lord Marshall. HM Treasury; November 1998.
- Rejuvenate or retire?, ibid, (pp 169–174).
- Interview with author, Adair Turner; 2018.
- Anita Charlesworth, ibid; March 2020.
- Commons Hansard; 27 November 2001 (cols 838–841).
- Treasury report’s author reopens the debate over funding for the NHS. Financial Times; 30 November 2001.
- Securing our future health, ibid, box (p 120) (www.webarchive.org.uk/wayback/en/archive/20130416040413/http://webarchive.nationalarchives.gov.uk/+/http://www.hm-treasury.gov.uk/consult_wanless_final.htm).
- Brown, ibid, (p 162).
- Budget 2002. HM Treasury; 2002 (paragraph 1.14) (https://webarchive.nationalarchives.gov.uk/+/http:/www.hm-treasury.gov.uk/media/4/1/Budget_2002.pdf).
- Commons Hansard; 17 April 2002 (cols 577–592).
- Ibid, (cols 594–599).
- Health Department misses third of targets. Financial Times; 16 April 2002.
- The five giants, ibid, (pp 619–621).
- Department of Health. Delivering the NHS Plan. Department of Health; 18 April 2002 (https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4005818).
- Commons Hansard; 18 April 2002, (cols 714–717).
- Blair, ibid, (p 491).
- Brown G. My life, our times. Vintage; 2017 (p 169).
- Commons Hansard; 23 April 2002 (col 162).
- Tories ‘should break NHS funding’. The Guardian; 11 April 2002 (www.theguardian.com/politics/2002/apr/11/nhs.conservatives).
- Riches beyond compare. Health Service Journal. 25 April 2002.
- Patients welcome Wanless report. BBC News; 17 April 2002 (http://news.bbc.co.uk/1/hi/health/1935089.stm).
- Reward system ‘will expand NHS Plan’. Daily Telegraph; 19 April 2002.
- Ben Page of Ipsos MORI. Personal communication; December 2020.
- Budget 2002, ibid, (p 121).
- Garner S, Littlejohns P. Disinvestment from low value clinical interventions: NICEly done? BMJ 2011; 343: d4519 (https://doi.org/10.1136/bmj.d4519).
- Timmins N, Appleby J, Rawlins M. A terrible beauty: A short history of NICE. The National Institute for Health and Care Excellence. 2016 (www.idsihealth.org/wp-content/uploads/2016/02/A-TERRIBLE-BEAUTY_resize.pdf).
- Interview with author; June 2020.
- Interview with author; June 2020.
- Interview with author; July 2020.
- Interview with author; March 2021.
- Interview with author; July 2020.
- NHS workforce statistics 1999–2009 (https://digital.nhs.uk/data-and-information/publications/statistical/nhs-workforce-statistics-overview/nhs-staff-1999-2009-overview).
- Department of Health. Referral to treatment times. Historical series on page: https://webarchive.nationalarchives.gov.uk/20130104155640/http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/HospitalWaitingTimesandListStatistics/index.htm
- Timmins N. Road to recovery. FT Weekend Magazine; March 13/14 2010 (p 24).
- Gardner T, Charlesworth A, Watt T. Returning NHS waiting times to 18 weeks for routine treatment: The scale of the challenge pre-COVID-19. The Health Foundation; 2020 (www.health.org.uk/publications/long-reads/returning-nhs-waiting-times-to-18-weeks).
- High quality care for all: NHS next stage review final report. Department of Health; 2008 (https://webarchive.nationalarchives.gov.uk/20130105053023/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_085825).
- Timmins N. Wisdom of the Crowd: 65 views of the NHS at 65. Nuffield Trust; 2013 (www.nuffieldtrust.org.uk/research/the-wisdom-of-the-crowd-65-views-of-the-nhs-at-65).
- Rejuvenate or retire?, ibid, (pp 169–174).
- Wanless D. Securing good health for the whole population: Final report. HMSO; 2004 (https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4074426).
- Ibid.
- Marmot M. From Black to Acheson: two decades of concern with inequalities in health. International Journal of Epidemiology. 2011; 30(5), 1165–1171 (https://doi.org/10.1093/ije/30.5.1165).
- Choosing health: Making healthy choices easier. Department of Health; 2004 (https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4094550).
- Shannon C. Second Wanless report welcomed by public health experts. British Medical Journal. 2004; 328(7439): 542 (www.ncbi.nlm.nih.gov/pmc/articles/PMC381076).
- Interview with author; June 2020.
- Interview with author; July 2020.
- On the state of public health: Annual report of the Chief Medical Officer 2003. Department of Health; June 2004 (www.researchgate.net/publication/319998715_On_the_state_of_public_health_Annual_report_of_the_Chief_Medical_Officer_2003).
- Donaldson L. The future of public health in Europe. The European Journal of Public Health. 2005; 16(5) (www.researchgate.net/publication/31061752_The_future_of_public_health_in_Europe).
- Wanless D. Securing good care for older people: taking a long-term view. The King’s Fund; 2006 (https://kingsfund.org.uk/publications/securing-good-care-older-people).
- Welsh Assembly Government. The review of health and social care in Wales. The report of the project team advised by Derek Wanless. Welsh Assembly Government; 2003 (www.wales.nhs.uk/documents/wanless-review-e.pdf).
- Interview with author; June 2020.
- 2007 Pre-Budget report and comprehensive Spending Review. HMSO; 2007 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/243167/7227.pdf).
- Department of Health. Our Health, our care, our say: A new direction for community services. Department of Health; 2006 (https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/272238/6737.pdf).
- Wanless D, Appleby J, Harrison A, Patel D. Our future health secured? A review of NHS funding and performance. The King’s Fund; 2007 (www.kingsfund.org.uk/sites/default/files/field/field_publication_file/our-future-health-secured-review-nhs-funding-performance-full-version-sir-derek-wanless-john-appleby-tony-harrison-darshan-patel-11-september-2007.pdf).
- Marmot M et al. Health Equity in England: The Marmot Review 10 Years On. Institute for Health Equity; 2020 (www.health.org.uk/publications/reports/the-marmot-review-10-years-on).
- High quality care for all, ibid.
- NHS England. The NHS belongs to the people: A call to action. NHS England; 2013 (www.england.nhs.uk/wp-content/uploads/2013/07/nhs-belongs.pdf).
- NHS England. Five year forward view. NHS England; 2014 (www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf).
- Timmins N. Highlights of Turnbull Interview. Financial Times; 20 March 2007, quoted in, Seldon A (ed.) Blair’s Britain 1997–2007. Ch 5, p 98. Cambridge University Press; 2007.
- Dickson N. Sir Derek Wanless obituary. The Guardian; 28 May 2012 (www.theguardian.com/society/2012/may/28/sir-derek-wanless).
- Sara S, Rosen R, Rumbold B. What is integrated care? Nuffield Trust; 2011(www.nuffieldtrust.org.uk/files/2017-01/what-is-integrated-care-report-web-final.pdf).
- IT suppliers welcome £1bn strategy for NHS records. Financial Times; 25 September 1998.
- Information for Health: An Information Strategy for the Modern NHS 1998–2005. NHS Executive; 1998 (https://webarchive.nationalarchives.gov.uk/20120503231618/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4014469.pdf).
- Davies N, Campbell L, McNulty C. How to fix the funding of health and social care. Institute for Government; 2018 (www.instituteforgovernment.org.uk/sites/default/files/publications/IFG_Funding_health_and_social_care_web.pdf).
- Cohen J, Chambers J, Silver M, Lin P, Neumann P. Putting the costs and benefits of new gene therapies into perspective. Health Affairs; 4 September 2014 (www.healthaffairs.org/do/10.1377/hblog20190827.553404/full)
- Marsden G, Towse A, Pearson S, Dreitlein B, Henshall C. Gene therapy: Understanding the science, assessing the evidence, and paying for value. A report from the 2016 ICER Membership Policy Summit; March 2017 (www.ohe.org/system/files/private/publications/ICER-Gene-Therapy-White-Paper.pdf).
- CDC. Understanding mRNA COVID-19 vaccines. CDC; March 2021 (www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/mrna.html).
- Department of Health. The NHS Improvement Plan. Department of Health; 2004 (http://1nj5ms2lli5hdggbe3mm7ms5.wpengine.netdna-cdn.com/files/2010/03/pnsuk3.pdf).