Acknowledgements
We would like to thank David Dixon, Wendy Lewis and Andrew Wilson for their contributions to this report, and Tom Downes, Ruth Glassborow, Andrew McLaughlin, Christine Owen, Zoe Radnor and Sharon Williams for their helpful comments on earlier drafts.
We would also like to thank colleagues at the Health Foundation and the Advancing Quality Alliance (AQuA) for their support, guidance and patience during the research, drafting and production of this report.
About this joint publication
Improving flow on a whole system basis is a field in which the Health Foundation and the Advancing Quality Alliance (AQuA) – an NHS quality improvement organisation – have a long-standing interest.
Over the past decade, the Health Foundation has supported a number of large-scale programmes aimed at improving the reliability and quality of clinical systems.,
One of the key sources for this report is the learning from one of these – the Flow Cost Quality programme – which set out to improve patient flow along the urgent and emergency pathway in two NHS foundation trusts in England., This programme has had a significant and sustained impact on service and patient outcomes, and has gained national recognition., To support other organisations seeking to make large-scale change, in 2015 the Health Foundation published a report, Constructive comfort.
This identifies a series of success factors that need to be in place for change to happen, and describes the steps that national bodies need to take to create the right conditions for change.
AQuA, meanwhile, has extensive experience in supporting and enabling change on a system-wide basis over the past six years. AQuA has worked with health and social care system leaders across the UK to design and implement new models of care based on a common vision focused on the needs and ambitions of each community. In early 2016, AQuA conducted a 90-day rapid review into whole system flow. The review sought out case examples from health care systems in the UK and internationally, considered the available evidence base and gained insights from other industry sectors. This report reflects AQuA’s learning from the review, and its work in supporting systems to build the capability to plan, deliver and sustain change.
As well as drawing on existing expertise and knowledge the Health Foundation and AQuA have gained from supporting system-wide change, this report is informed by a series of discussions and workshops with experts in complex systems change and reviews of the published evidence. A summary of our research and engagement approach is set out in Appendix 1.
While we have drawn on learning from research and practice where it exists, many of the case studies explored in this report are at the leading edge of health care improvement practice. This work is typically at an early stage and is yet to produce measurable or independently validated results. The studies are presented here in order to provide insight into how some health and social care systems are beginning to grapple with the challenges of improving flow on a system-wide basis.
Executive summary
Improving the flow of patients, service users, information and resources within and between health and social care organisations has a crucial role to play in driving up service quality and productivity.
If every organisation in each health and social care economy were able and willing to work collaboratively to design services that optimise flow, it could lead to major improvements in patient and service user experience and outcomes.
The importance of flow is increasingly recognised by practice leaders and policymakers throughout the UK. For example, there have been recent flow improvement programmes in both Scotland and Wales. The concept of improving flow is also referenced nationally and locally, across the UK, in strategies for service configuration and for tackling emergency and elective access challenges. Where providers have been able to match capacity and demand and enable better flow between departments and organisations, there have been impressive results.
However, while there are positive examples, and while flow has become common parlance in health service management, it is important not to underestimate the scale of the challenge facing those who want to realise the full potential of flow improvement. To date, virtually all attempts to improve flow have focused on single organisations or pathways. Hardly any have sought to improve flow across the entire primary, acute and social care spectrum. The task of bridging the entrenched cultural differences between professions and bringing together organisations that have often been governed, funded, inspected and regulated in isolation has been too daunting for most.
Nonetheless, this report argues that local health and social care economies are now well placed to improve whole system flow. Not only is there now a good understanding of the methods and skills needed, but the financial logic for tackling expensive and resource-intensive bottlenecks in the flow of patients and service users between organisations is hard to resist.
The aim of this report is to provide leaders and improvement teams in local health and social care economies across the UK with a guide to the activities, methods, approaches and skills that can help to improve flow across systems. It also describes the steps that policymakers and regulators at a national level need to take to create an environment that is conducive to change on this scale.
To support this, the report sets out an integrated, multi-level organising framework. This is supported by four case studies of innovative and effective practice: the Sheffield and South Warwickshire-based Flow Cost Quality programme; the Darlington Dementia Collaborative; the ‘Wigan Deal’ for adult social care and wellbeing; and the Winona Health Transformation programme in the US.
The organising framework focuses on four distinct but interdependent levels of the system:
- Care journeys – The primary focus of any flow-related initiative should be to improve the patient and service user’s experience. It can do this through the removal of the bottlenecks, waste, delays and duplication that affect the quality of patients’ and service users’ experiences and, in many instances, the effectiveness of the care they receive. Any redesign process should also look at how to eliminate the ‘failure demand’ – demand arising from failure to provide a service or to provide it in a timely and effective fashion – that leads to people flowing into the system unnecessarily.
- The report sets out a structured approach for improving flow at the care journey level that encompasses five key areas of work:
- Creating a space for system partners to come together, build relationships, develop a sense of shared purpose and deliver co-designed solutions.
- Understanding ‘the current state’ by enabling service providers and users to work together to map the processes in each care journey and identify non-value adding activity.
- Collecting and analysing data with a view to understanding the root causes of problems and identifying potential solutions that can then be tested.
- Developing a high level ‘future state’ plan underpinned by simple guiding rules that local teams have the licence to adapt to fit their own context.
- Implementing solutions in which all parts of the system have a shared stake and responsibility, and providing opportunities for collaborative reflection and further refinement as outcomes emerge.
- Team and organisational capabilities – To improve flow successfully at the care journey level, front-line teams need to have the skills and capacity to continuously improve the quality of the care they provide. Using examples from the UK and other countries, the report describes the steps that some organisations and local health and social care economies have taken to build and sustain improvement capability.
- Local health and social care economy enablers – System leaders in each economy have a key role to play in identifying and addressing the various operational, financial, information and workforce-related issues that may support or stand in the way of effective whole system working. They also need to focus on building a learning culture in which staff, patients and service users have the capability, capacity and confidence to work together to identify problems and carry out tests of change.
- National system change levers – In what is still a highly centralised health and social care landscape, national bodies have a major influence on the ability of local economies to drive and sustain change. The report highlights the need for central regulatory, financial and performance management levers to be closely aligned with nationally driven programmes aimed at promoting whole system working, such as Sustainability and Transformation Plans in England. Ensuring that these central levers and programmes are governed by a shared understanding of how to achieve change is particularly important.
The report also emphasises the need for policymakers to give local economies the time, space and resources they need to deliver meaningful change. Finally, it argues that there needs to be a closer configuration between the practice of improvement – where the emphasis is on discovering a way towards a tailored solution through repeated tests of change – and the prevailing discourse of public sector reform, with its emphasis on the rapid development and spread of previously identified solutions.
For local health and social care economies to achieve sustained improvements in flow on a whole system basis, progress will be needed on all four of these levels. However, doing so has the potential to greatly improve the quality of care provided to patients and service users, and to make their experience of care an altogether better one.
* In this report we use the term ‘whole system flow’ to define the coordination of all processes, systems and resources, across an entire local health and social care economy, to deliver effective, efficient, person-centred care in the right setting at the right time and by the right person. There is also a glossary on pages 52-57 to provide explanations of other terms used in the report.
† In this report ‘a local health and social care economy’ refers to a geographically-defined system of health and social care organisations and services, serving a particular area.
Introduction
Improving the flow of patients and service users within and between health and social care organisations is being increasingly focused on across the UK. It is seen by both practice leaders and policymakers across the UK as having a crucial role to play in driving up service quality and productivity, as well as greatly improving the experience of care for patients and service users.,,,,,
A range of important work is currently being done in this field around the UK. For example, in England, the Emergency Care Improvement Programme is helping to improve patient flow in 40 challenged urgent and emergency care systems. NHS Improvement has entered into a five-year partnership with Virginia Mason Institute to support five NHS trusts to develop a culture of continuous improvement. And providers and commissioners in each local health and social care economy are looking at how to improve service integration and patient flow as they develop Sustainability and Transformation Plans (STPs) and implement new models of care. Elsewhere in the UK, flow improvement programmes are being delivered in Wales – the evaluation of which is being funded by the Health Foundation – and also in Scotland.
The prize on offer is immense. If organisations are used to working collaboratively, and go out of their way to strengthen relationships and tackle the barriers to the smooth and efficient flow of patients and service users, they will be able to deliver better health and social care for their population and make better use of increasingly scarce resources. The experience for those using services would also be improved. However, there are some significant challenges that need to be overcome if the full potential of work on flow is to be realised. Chief among them is the entrenched divides between primary, acute and social care services that give rise to silo working and piecemeal, disjointed efforts to improve services.
It is critical to recognise that improving flow is as much a behavioural and relational challenge as it is a technical one. Much will hinge on the ability of local health and social care economies to foster a culture of learning that gives members of staff – working alongside patients and service users – the space, skills and permission to discover their way towards solutions to poor flow together.
As well as examining these challenges, this report sets out an organising framework, supported by case studies. The framework describes steps that can be taken to improve the flow of patients and service users, recognising this in turn requires improvements in the flow of information, equipment and staff. It provides leaders and improvement teams in local health and social care economies with a guide to the activities, methods, approaches and skills that can help to improve flow across whole systems. It also describes the steps that policymakers and regulators at a national level need to take in order to create an environment that is conducive to change on this scale.
The report consists of seven sections:
- Section 1 defines what we mean by whole system flow and explains why it is important. It also considers some of the factors that have made improving flow difficult to achieve to date. The section then describes the core components of a typical local health and social care economy and some of the techniques that can be used to understand whole system flow.
- Section 2 introduces the organising framework for improving flow across whole systems. This consists of four levels: care journeys; front-line team and organisational capabilities; health and social care economy enablers; and national system change levers.
- Sections 3-6 look in detail at each of the four levels in the framework
- Section 7 summarises the main messages from the report and provides a set of recommendations for providers, local system leaders, regional bodies and policymakers to help them take this work forward. Doing so successfully has the potential to greatly improve the quality and experience of care for patients and service users across the UK.
A note on language used in this report
Local health and social care economy: In this report ‘a local health and social care economy’ refers to a geographically-defined system of health and social care organisations and services, serving a particular area.
Whole system flow: We use the term ‘whole system flow’ to define the coordination of all processes, systems and resources, across an entire local health and social care economy, to deliver effective, efficient, person-centred care in the right setting at the right time and by the right person.
Context and definitions
What we mean by ‘whole system flow’ and why it matters
The language used by those who have an interest in improving the flow of people or resources within or between services is often technical: batching, bottlenecks, constraints and capacity management. Yet the effects of poor flow are all too readily apparent in the daily experiences of patients, service users and people working at the front line of health and social care. Stark examples of a lack of smooth flow through a system include ambulances queuing outside hospitals, crowded emergency departments, long waits on trolleys for a bed, pressures on community and social care services, overstretched GPs, and mental health patients being transferred hundreds of miles for an inpatient bed. All of this is stressful and frustrating for staff and can be devastating for patients, service users and their families and carers.
At a time when health care is under increasing financial pressure, poor flow is both a symptom and a cause of that resourcing crisis. Delays and waits are exacerbated by deficiencies in critical areas and the resulting disruption to flow leads to an ever more suboptimal use of the resources within the health and social care system.,,
Where providers have been able to match capacity and demand and enable better flow between departments and organisations, there have been impressive results.
Work supported by the Health Foundation at Sheffield Teaching Hospitals NHS Foundation Trust and South Warwickshire NHS Foundation Trust through the Flow Cost Quality programme has delivered sustained reductions in emergency care length of stay, bed occupancy and readmissions, while improving safety and the patient experience., In the US, leading high-performing providers such as the Mayo Clinic, Seattle Children’s Hospital and Cincinnati Children’s Hospital have achieved significant productivity gains and savings using flow improvement approaches (see Box 2).
Yet most flow-related initiatives to date have focused on a small segment of the patient or service user journey, usually within acute hospitals. There is a pressing need to look beyond the hospital and to give attention to every team, service and organisation that patients and service users encounter. As well as looking at services delivered within the NHS there is also a need for consideration of social care, health promotion and other local government services. Nor should the wider determinants of health (eg age, lifestyle, environment) be forgotten – or the need to tackle the gulf between physical and mental health services.
It is a lot easier to call for a whole system approach to flow than it is to deliver it. Over the past 15 years a series of UK national bodies have made strong cases for looking beyond the hospital – to look at flow from a system-wide perspective.
The most recent – but far from the first – example is NHS England’s 2015 guide for health and social care communities on delivering urgent and emergency care. This underlined the value of whole system partnerships in improving flow. A decade earlier, in 2005, the NHS Institute for Innovation and Improvement published a guide to improving flow for system leaders, which made the point that most existing flow-related improvement work had tended to focus on single bottlenecks in the system. Future work, it said, needed to understand the flow of patients across departments, organisations and the whole system. There was also a strong emphasis on ‘whole systems working’ in many of the programmes supported by the NHS Modernisation Agency; for example, the Acute Local Improvement Partnerships, announced in 2003, used ‘a whole systems approach to follow the patient’s pathway across departmental and clinical boundaries, to deliver better care and minimise delay’. In Scotland, meanwhile, a 2007 report on patient flow in planned care made it clear that ‘the importance of getting the flow of patients right across the whole system cannot be overstated’.
Yet it has proven difficult to translate this whole system vision into reality. In Section 1.2 we consider the issues that have made it so difficult, but also describe why there are reasons to believe that change is achievable.
The challenge of achieving system-wide change
Albert Einstein once said that ‘without changing our pattern of thought, we will not be able to solve the problems we created with our current patterns of thought’. It is a quote that often crops up in articles about how to enable change in complex systems such as the NHS27 – and it does so for good reasons. Health and social care leaders and policymakers across the UK have been trying for years to cajole or nudge the various organisations and groups within their world towards a more ‘whole system’ way of working. Yet despite a succession of national initiatives – the latest in England being the Integrated Care Pioneers and New Care Models vanguard partnerships – genuine, joined-up, whole system delivery is still the exception rather than the rule.
Various elements of the system are governed, funded, inspected and regulated in silos. This reinforces significant differences, not just geographically but also culturally, between those working in hospitals and those working in community services or in primary care. As the NHS five year forward view (Forward View) stated, in relation to England, many elements of the ‘classic divide’ between ‘family doctors and hospitals, between physical and mental health, between prevention and treatment’ that characterised the NHS in 1948 remain in evidence today.
The cultural divisions between the NHS and local government are often even sharper. Local authorities are less bound by central government direction, face resource pressures even more extreme than those in health care, and are driven by the need to deliver on a local democratic mandate expressed through elected members. Across the UK there is now a greater emphasis on collaborative working between local government and the NHS. A number of new initiatives such as health and wellbeing boards and the Better Care Fund in England, and health and social care partnerships in Scotland, have been set up with this aim in mind. But while these arrangements are helping to build trust and understanding between organisations, the picture is still very patchy. In some areas, the challenge of managing potentially thorny and politically contentious processes, such as the handover of patients from acute to social care settings, exacerbates tensions between providers.
During times of financial uncertainty and risk, it is not easy to encourage people and organisations to do things differently. While some see a ‘burning platform’ and are galvanised into collaborative action, others respond to the pressure of the situation by clinging ever more tightly to their established ways of working. As Peter Senge has noted, our brains tend to ‘downshift’ under pressure and we revert to our most habitual modes of behaviour. Evidence of this can be found in the tendency of some NHS providers, when faced with many competing demands, to adopt a highly bureaucratised form of management that leads to defensive and reactive behaviour and superficial displays of compliance rather than genuine efforts at improvement. Others, meanwhile, are so focused on the task of securing their immediate survival and on short-term business priorities that they do not have the headspace to think about the long-term gains that can come from working collaboratively. Quite simply, they are too busy firefighting the latest crisis to worry about anything else.
In saying this, there is room for some optimism. If you look at the factors that David Gleicher and others have suggested are necessary in order to deliver meaningful change – dissatisfaction with how things are now, a vision of what is possible, an appreciation of how change is to be implemented, and the capacity for change – there are grounds to think that we are close to tipping point on many of them.
With health and social care budgets severely stretched in every UK nation, the financial logic for tackling expensive and resource-intensive bottlenecks in the flow of patients, service users, information and equipment across the system is hard to resist. The moral and emotional case – exemplified by the human costs of delayed hospital discharge of frail, older people – is equally powerful. Moreover, there are enough inspiring examples of effective cross-organisational working – some of which are highlighted in Sections 3 to 5 – to show that real change is achievable even in the most pressured of times.
The renewed interest at national level in prevention and public health, described in England in the Forward View as being in need of ‘a radical upgrade’, is also helping to create the conditions in which local health and social care system leaders are ready to work together to improve flow – or, better still, ensure that people do not need to flow into the system at all. One indication of this is the emerging interest among public service leaders, particularly in Scotland,, in the concept of ‘failure demand’, or ‘demand caused by failure to do something or do something right for the customer’. By focusing on avoiding failure demand, a requirement is placed on health and social care leaders to work alongside their peers across the whole of the public sector, including, but not limited to, housing, education and employment.
There is also a better understanding of the capabilities and methods that can help to deliver whole system change. Senge, for instance, takes heart from the ‘extraordinary expansion in the tools to support system leaders’ to ‘see the larger system’, ‘foster reflection’ and ‘co-create the future’. He argues that the strategic use of these tools ‘at the right time, with the right spirit of openness’ can help to address ‘previously intractable situations’ and inspire confidence that change is possible. What is not in evidence, as yet, is a critical mass of people across the health and social care landscape with the capabilities to use these tools effectively.
This report aims to help local health and social care economy leaders as they begin to think about how to build the necessary capabilities to improve flow on a system-wide level. Section 1.3 describes the core elements of an archetypal local health and social care system, to which this report speaks.
Enabling change across an entire health and social care system is not easy. Even tasks that would appear to be fairly straightforward, such as defining what the system is, can be challenging. If you were to ask a dozen health and social care professionals to define their local system, you would likely receive a dozen different answers, even from people who worked in the same department. Ultimately, it will depend on what each person sees as being the core purpose of the system: those who see the avoidance of failure demand, for example, as being its key organising principle may define the system in broader terms than their peers focused on the operational realities of meeting the needs of the patients and service users in front of them. When change is being planned and delivered, it is important to surface such views early on to avoid potential misunderstandings and conflict at a later stage. Moreover, a shared definition of what is in and out of scope is an essential first step in understanding a system and identifying the weaknesses and constraints within it.
While each set of local leaders will define their systems according to their local context and priorities for action, it is useful to have an archetype in mind when describing, as this report seeks to do, the capabilities and resources needed to improve flow on a whole system basis. Our archetypal system, illustrated in Figure 1, is focused on the organisations that will be involved once a need for care has been identified. This care system sits within a wider system that influences the health and wellbeing of the public. The relationship between these two distinct but interlocking systems is crucial. From a health and social care provider perspective, a close and transparent relationship between them and other partners with a wellbeing focus – which provides scope for joint working, information sharing and peer challenge – will help to ensure that any care system redesign activity is consistent with the needs of the wider population. It may be, after all, that resources allocated towards optimising primary and acute care journeys could have a bigger impact if they were used to address an underlying cause of ill health in the area.
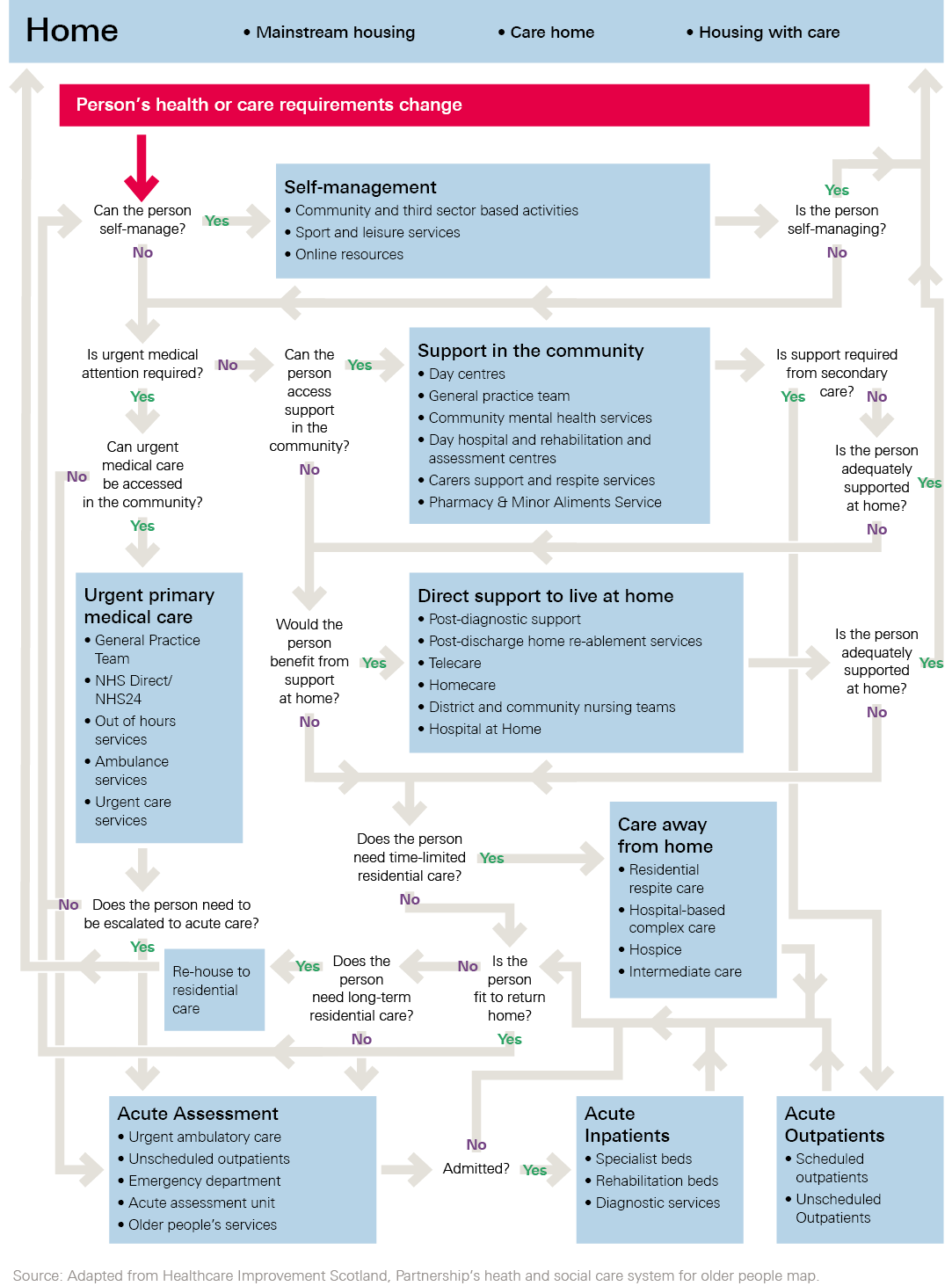
Figure 1 is based on a typical system in England and is designed to illustrate the possible extent of a system-wide approach to improving flow, in terms of the number of organisations, professionals, patients and service users involved. Figure 2 illustrates an example of the care journeys that run through a local health and social care economy. It shows the many teams potentially involved.
Figure 1: Anyborough, England – a local health and social care economy
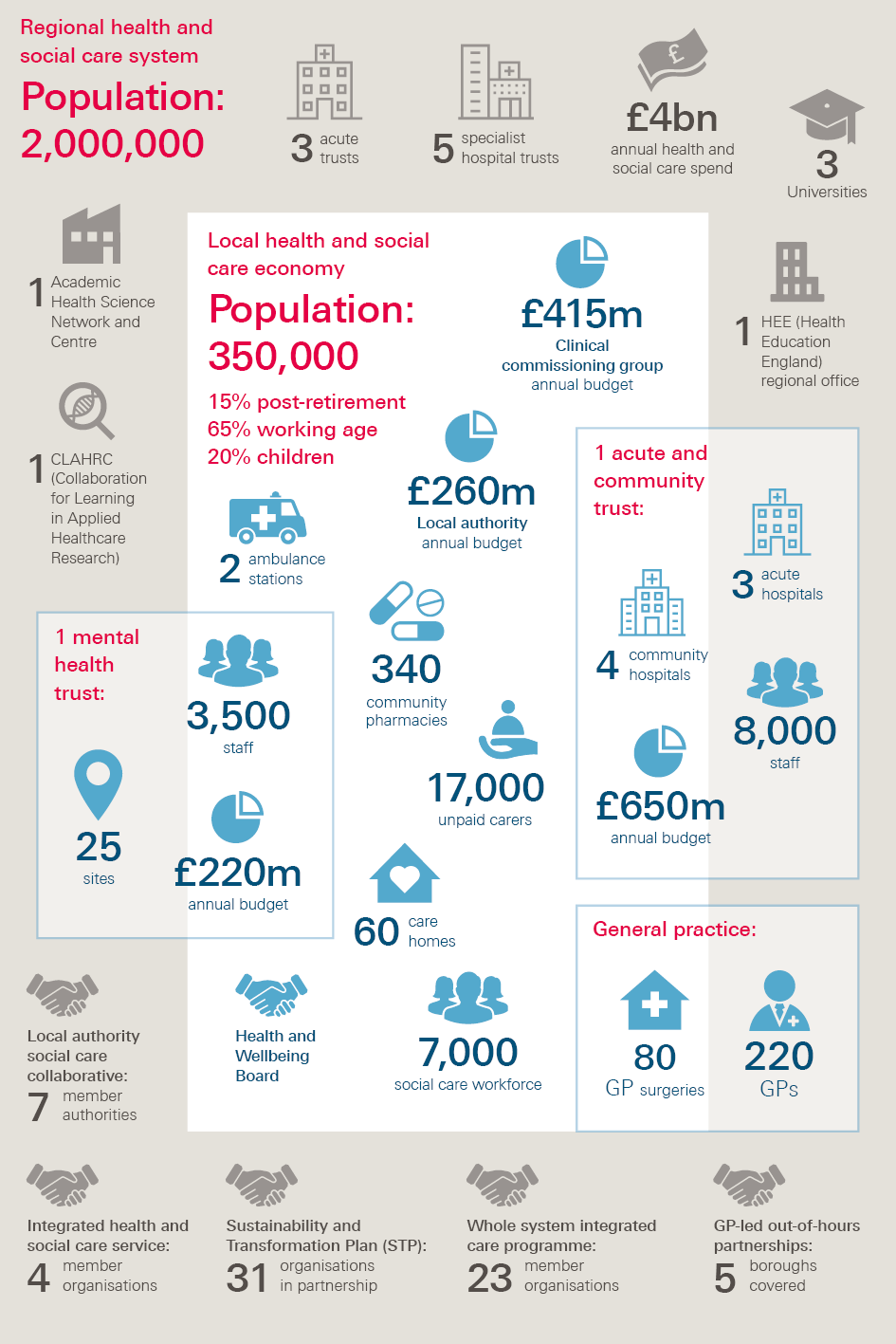
Figure 2: Anyborough local health and social care economy care journeys
It can be difficult, even for experienced system leaders, to navigate the landscape illustrated in the Figure 1. While this makes flow improvement hard, methods for understanding and improving flow (see Box 1 and Section 3.2) can help to make sense of the landscape. AQuA’s work with organisations in the north west of England has led it to conclude that a focus on patient flow can be an effective way of helping people see and understand the complexity of the system in which they are working. Flow improvement methods provide a means of fostering greater collaboration within and between organisations and designing care models that will better meet the needs of the local population.
The benefit of examining the system through a care journey lens, as shown in Figure 2, is that it allows system leaders to see how services are connected and where constraints may exist. It also allows them to start to consider what activities might be amenable to flow improvement approaches and what resources and capabilities they will require. It may be that approaches which have been primarily used to improve flow in acute contexts may need to be adapted, or may not be applicable at all, to the type of challenges faced by organisations focused on prevention and continuing care.
Identifying flow within the system
The concept of flow is closely associated with the approach to quality and productivity improvement known as ‘lean’ or the Toyota Production System. In their definitive book on the subject, Lean thinking, James Womack and Daniel Jones use health care as a prime example of the lack of flow in a system.
‘What happens when you go to your doctor? Usually you make an appointment some days ahead, then arrive at the appointed time and sit in a waiting room. When the doctor sees you, usually behind schedule, she or he makes a judgement about what your problem is likely to be. You are then routed to the appropriate specialist, quite possibly on another day, certainly after sitting in another waiting room. Your specialist will need to order tests… requiring another wait and then another visit to review the results… If you are unlucky and require hospital treatment, you enter a whole new world of disconnected processes and waiting.’
Lean practitioners argue that the absence of flow arises out of the ‘batching’ of patients, service users and routine tasks, so that they are seen or completed at the same time by members of staff. For patients and service users, this can be incredibly frustrating, as it means that they often have to wait in a queue until the next stage in the process is ready to begin. It is also an enormous source of potential error, duplication and waste.
As well as looking at the flow of patients and service users through a set of care processes, it is important to look at the flow of the information, resources and staff that need to come together to enable effective care of these individuals. In acute settings, the flow of staff to the patient can be critical, for example, having an early senior clinical decision maker available on arrival in an emergency department. Effective flow of information across a system also matters: for example, if all professionals treating a particular patient had access to a shared care record it would significantly reduce waste and delays.
An effective flow of resources is also essential so that a lack of finance in one part of the system – for example, in social care or domiciliary services – does not mean that patients and service users experience a delay in discharge and an unnecessary stay in hospital because there is nowhere for them to go. These different types of flow need to be made visible and purposefully designed and managed to ensure they are mutually supportive.
Understanding flow across the whole system
Once the different flows have been identified, further work is needed to understand variations in demand and capacity within the system and the root causes of them. While there are examples of analysing the flow of patients, service users, data and resources within specific services or organisations, rarely has this been done across a whole system.
Analysing flow across a whole system is a major undertaking. This is especially so given the lack of easily accessible cross-organisational data, and the shortage of analytical capability. Yet, as discussed in Key area 3, such analysis is critical.
While it is important to be pragmatic about the time and resource available for analysing the system, experience from other sectors underscores the importance of doing so. Analysis is especially important when the systems are too big and complex for people to easily see through their direct experience, or to be able to predict how they will respond to change. Consequently, there is a strong case for investing substantially in system analysis before making changes to care processes and services, especially given the potential cost and quality implications of any changes.
Some common approaches that have been used in the UK and other countries to understand flows across complex organisations or care journeys with many variables and interrelationships are described in Box 1.
Box 1: Methods for understanding system flow
SIMULATION AND MODELLING
Simulation and modelling of patient or service user flow can provide insight into where bottlenecks occur in a health care system. They allow service planners to evaluate the benefits and pitfalls of potential improvements before enacting them.
Simulation has been widely used in manufacturing and in the logistics sector with the aim of optimising throughput and profitability. Gatwick Airport, for example, has used simulation of passenger flow through the check-in process to increase understanding of variation and where bottlenecks were occurring. Gatwick was able to make changes to the process as a result and has seen an improved check-in process with reduced queue times and improved airline efficiency.
In health care, simulation and modelling approaches have been used to manage bed capacity, schedule staff, manage admission and scheduling procedures, and to test the value or functionality of new initiatives and services before they are implemented.
The effectiveness of these approaches is often contingent on the quality of the process mapping used to inform them, as well as the robustness of the data used to populate them. Finding sufficient funding and staff with the right skills to build and run simulations is a further challenge.
Resources
- SAASoft has developed a whole system dynamics simulation for education purposes, with five interdependent components: home, hospital, intermediate care, care home and cemetery.
- The Basic Building Blocks methodology published by the Scottish government offers a systematic approach to the demand and capacity analysis of existing care journeys. Its tools can be used for simulation modelling.
Examples from the peer reviewed literature
- In England, researchers used simulation to create a ‘perfect world model’ for accident and emergency (A&E) care – not as it is, but as it could be. Importantly, the ‘efficiency gap’ between the ‘perfect world’ and the ‘real world’ was used to identify the location of bottlenecks in the current ‘whole hospital’ care journey and brainstorm ideas for improvement.
- An English primary care commissioning organisation focused on improving the use of unscheduled care and support efficiency gains in the local hospital. A model of the system was developed to help set usage targets at the micro-level of the hospital. The model drew on a small number of readily available key data items. The model emphasised that primary care had an important role in changing the culture, communication and care provided within A&E and other unscheduled services.
- A Swedish hospital has used a simulation model to support discussions about the resources, capacity and work methods that would be required on a maternity ward that was shortly to be built.
- In Canada, a simplified, low-cost simulation platform, developed using spreadsheets, was found to be as effective in predicting patient flow patterns as more expensive commercial software packages.
VALUE STREAM MAPPING
Value stream mapping (VSM) is an approach that produces a visual map of a system or process.
It is often used by multidisciplinary teams to improve processes as part of lean/continuous improvement projects.
Using VSM, a team can produce a visual map of the ‘current state’, identifying all the steps in a patient or service user’s care journey.
The team then focuses on the ‘future state’, which often represents a significant change in the way the system currently operates. This means that the team needs to develop an implementation strategy to make the future state a reality.
Using VSM can result in streamlined work processes, reduced costs and increased quality.
Resources
- The NHS Institute for Innovation and Improvement produced a guide to using VSM.
- Another useful guide to VSM can be found on NHS Scotland’s Quality Improvement Hub.
Examples from the peer reviewed literature
- In Ireland, researchers used lean principles and the theory of constraints to identify bottlenecks in patient journeys through A&E. For each stage of the patient journey, average times were compared and disproportionate delays were identified using a significance test.
- A value stream map and the five focusing steps of the theory of constraints were used to analyse these bottlenecks.
- A US multidisciplinary team analysed the steps required to treat patients with acute ischemic stroke and developed a streamlined treatment protocol.
QUEUEING THEORY
Queuing theory, or the study of waiting lines, or queues, can help to understand and address mismatches between service demand and capacity. Usually a mathematical model is constructed to help predict queue lengths and waiting times. Historical data are analysed to explore how to provide optimal service while minimising waiting, thus providing an objective method of determining staffing needs during a specific time period. Popular in other industries, queuing theory has also been used in health care, particularly by hospitals wanting to understand waiting times for unscheduled care or the time spent waiting for specific equipment, surgery or laboratory results. It is also applicable to wider systems of care or transitions.
Examples from the peer reviewed literature
- A hospital in England used queuing theory to analyse one year’s worth of data to help understand the practical challenges associated with variation in patient demand for services and length of stay. The analysis found that daily bed shortages are mostly influenced by the timing of arrival and discharge of patients with a short length of stay, and that bed shortages around holiday periods are not due solely to increased demand, but also a reduction in staff and service capacity in and out of hospital around these times.
- In Canada, researchers used queuing theory at an organisational level to analyse the relationship between patient flow to A&E and patient flow to the inpatient unit. They then used the model to estimate the average waiting time for patients and the resources needed in unscheduled and inpatient care. The model was used to analyse the potential impacts on waiting time and resources of an alternative way of accessing unscheduled care and this helped managers plan the resources needed to enhance patient flow.
- The Scottish Whole System Patient Flow programme has also been informed by queuing theory (see Box 5).
Experience of improving flow at a system level
In recent years, there has been a significant growth in thinking about how to improve flow within health care processes and systems. One of the leading experts in the field, Eugene Litvak suggests that to improve flow in a health care setting it is necessary to:
- understand variation in the performance of a process over time and its sources
- separate patient flows into appropriate streams
- redesign work processes for those streams to smooth out the flow
- match capacity with estimated demand.
Around the world, a number of hospitals have worked to redesign care journeys in order to improve flow using these principles (see Box 2).
Within the UK, the Royal Bolton Hospital took a similar approach between 2004 and 2010. This led to improvements in quality and productivity. For example, a redesign of the process for patients with fractured hips reduced length of stay by 33% and reduced standardised mortality by 50%. An audit concluded that there had also been a 42% reduction in paperwork for the staff involved.
More recently, flow improvement programmes have been implemented across Wales and Scotland (see Box 3).
The Welsh Patient Flow programme, which involved all health boards with general hospitals that admit emergency patients and the Welsh Ambulance Service, has succeeded in delivering some improvements in flow in local pathways. It has also generated some valuable learning about the challenges involved in using a national breakthrough collaborative model to improve flow across multiple sites at the same time.
However, while primary, community and social care services have been involved in the Welsh programme, much of the improvement activity has focused on the acute sector. The same is true of the Scottish Whole System Patient Flow programme, which got underway in 2013, a few months after the Welsh programme.
The challenge now is to build on this work to improve flow within hospitals, and develop approaches which look at flow across the whole of the health and social care system. This would involve the smoothing of demand upstream – in particular in general practice – and the development of community resources downstream to allow a smooth and safe flow of patients out of hospital once they are fit for discharge.
Box 2: International examples of flow improvement programmes
Cincinnati Children’s Hospital implemented a series of measures to match capacity with demand and improve quality. It reported a cost avoidance of $100m in capital costs and an increase in its margin of more than $100m annually.
‘Esther’ in Jönköping in Sweden was led by a team of physicians, nurses and other providers who joined together to improve patient flow and coordination of care for older patients within a six-municipality region. It reported significant reductions in hospital admissions, days spent in hospital by heart failure patients, and waiting times for referral appointments with a range of specialists.
Intermountain Healthcare is an integrated system in Utah and Idaho in the US that consists of 23 hospitals and 160 clinics and has a workforce of 32,000. Its improvement journey, which began in the late 1980s, has been influenced by Deming’s insight that the best way to reduce costs is to improve quality. Intermountain has driven improvement by focusing on measuring, understanding and managing variation among clinicians delivering care. In the past 20 years it has delivered more than 100 clinical improvement initiatives that it reports have improved outcomes and reduced costs. The introduction of an elective labour induction protocol, for example, has helped to reduce the rate of caesarean sections and saved around $50m each year in Utah.
Lee Memorial Health System in Fort Myers, Florida, reported savings of $5.3m by adopting lean principles across the organisation. It also recorded improvements in unscheduled admission rates and overall patient flow.
The Mayo Clinic in the US used variability methodology to analyse surgeries over a three-month period and construct models of the resources used for scheduled and unscheduled cases. Guidelines were implemented to smooth the daily schedule and minimise variation. It reported a range of improvements in its productivity and resource use. Overtime staffing decreased by 27%, the number of elective scheduled same-day changes decreased by 70% and net operating income improved by 38%.
Seattle Children’s Hospital used Integrated Facility Design, an adaptation of the Toyota 3P process, to design a surgery centre with reduced variation and improved cost-effectiveness. Using this approach resulted in completion 3.5 months ahead of schedule, with estimated savings of $30m in project costs and improved patient throughput.
Virginia Mason Medical Center in Seattle is a leading example of the application of the Toyota Production System principles, or ‘lean’, to improve flow. After adopting lean as its management system in 2002, the center has reported appreciable and sustained improvements in clinical outcomes, safety, patient satisfaction, process indicators, staff engagement and costs. The prevalence of hospital acquired pressure ulcers, for example, fell from 5% to 1.7% between 2007 and 2012. Liability claims also dropped by over half and the centre achieved positive financial margins each year through efficiency savings, after previously losing money in consecutive years. It has also been named as ‘top hospital of the decade’ by Leapfrog and has been ranked in the top 1% of US hospitals for quality and efficiency.
Its success has been underpinned by an improvement approach – the Virginia Mason Production System – which seeks to standardise processes where possible, streamlining repetitive aspects of care to reduce waste and free up staff time with patients. All 5,500 staff at the centre are trained in the approach. The emphasis is on creating a culture of learning throughout the organisation, which can be applied successfully to drive continuous improvement.,,,
Box 3: UK examples of national flow improvement programmes
The Scottish government has developed two programmes that focus on flow, primarily within acute systems:
- Launched in 2013, the Whole System Patient Flow programme, which has been delivered in collaboration with the Institute for Healthcare Optimization (IHO), contains a number of acute-focused workstreams. The programme draws upon IHO Variability Methodology® and ‘classic queuing theory’ to describe and achieve ‘optimal flow’. Four territorial health boards have well-established projects; a further six (of a total of 14) have completed a Scottish Patient Flow Assessment and are starting their own pilot projects.
- The Unscheduled Care programme, launched in May 2015, is focused on achieving the four-hour emergency Access Standard across Scotland through six essential actions. The programme has adopted a collaborative approach underpinned by measurement for improvement and other quality improvement approaches. The building blocks of the programme involve six high-level themes, which are managed both individually and collectively. NHS Scotland has reported that this whole system approach has helped to improve flow for over 40,000 people in the last year: long waits of 8 hours and 12 hours have improved by 92% and 100% respectively.
The Welsh 1000 Lives Patient Flow programme was launched in June 2013 and ran until August 2015. It aimed to develop organisational capability and improve the effectiveness, efficacy and efficiency of the system for managing the care and flow of patients from the point of unscheduled entry, through diagnosis and treatment to discharge. Participants in the national roll-out of the programme included the Welsh Ambulance Services Trust (WAST) and the six Local Welsh Health Boards (LHBs) with general hospitals that admit emergency patients.
The programme was publicised as a ‘Breakthrough Collaborative’, modelled on the work of the Institute for Healthcare Improvement, and its conceptualisation and design was informed by the Health Foundation’s Flow Cost Quality programme. It had three main components: national learning events, a computer-based training course, and local workshops at each of the participating sites. The programme has achieved some improvements to patient flow within certain pathways and has led to the sustained use by some LHBs of the Big Room process and the A3 structured problem-solving process (see Case study 1 for details of these processes). However, it has proven more difficult – certainly within the relatively limited time and resources allocated to the programme – to deliver wide-scale improvements across participating sites.
Summary
This section has highlighted the importance of improving flow across whole health and social care systems. It has summarised what is known about how to develop a deeper understanding of flows and offered international and UK-based examples of what can be achieved through the application of flow improvement methods. While these methods have significant potential to help address the challenges faced by the system, realising this will require long-term commitment and investment.
Section 2 proposes an organising framework to guide such efforts. It identifies four levels of action that need to be woven into a coherent strategy to realise the potential of flow improvement.
‡ See glossary for definition of these terms, as well as others used in this report.
§ Eugene Litvak is at the Institute for Healthcare Optimization, which is supporting the Scottish Whole System Patient Flow programme.
¶ ‘upstream’ refers to services encountered early in a care journey (eg primary care), while downstream refers to those encountered at a later stage (eg secondary or tertiary care). See glossary for more details.
An organising framework for improving whole system flow
The need for a multi-level approach
Significantly reducing waste and waiting from local health and social care systems will require a joined-up development strategy operating at multiple levels (see Figure 3). At the care journey level, the tools and techniques of lean provide helpful insights into how to tackle bottlenecks and remove waste, delays and duplication. For this work to be successful, however, communities also need to invest in the improvement skills and capacity of front-line teams and organisations so that they are capable of continually improving the quality of the work they do. Senior system leaders within each local health and social care economy also need to identify and address the local issues that may impact effective whole system flow. Finally, national policymakers and regulators have a role to play in creating an environment that is conducive to improving whole system flow.
In developing and implementing a strategy across these levels, it is important to recognise that improving flow is much more than just a technical challenge. Behaviours and relationships matter as much, if not more. The ability of local health and social care economies to foster a culture of learning behaviour is critical. This culture is one where members of staff at all levels are in the habit of ‘repeatedly accumulating insights, improvements and innovations, and putting them to good use’, as Steven Spear put it. Equally valuable is the capacity to work collaboratively with people with different professional values and ways of working. In many cases, the success of large-scale change rests on the quality of these relationships.
Resilience is also crucial. On the shifting sands of the health and social care landscape – where new performance challenges are always emerging, strategic priorities and leaders come and go, and partnership arrangements are in a state of constant flux – it can be difficult to maintain enthusiasm and the momentum for change. Every change journey is pitted with obstacles and has points when things appear to be going backwards rather than forwards, putting hard-won gains in jeopardy. An ability to pick up the pieces after such setbacks and begin again is one of the most essential improvement skills, yet is rarely mentioned or appreciated.
The rest of this section provides an overview of what is needed, at each level, to improve whole system flow. Sections 3 to 6 discuss what is possible at each of the four levels in more detail.
Figure 3: An organising framework for improving flow across multiple levels
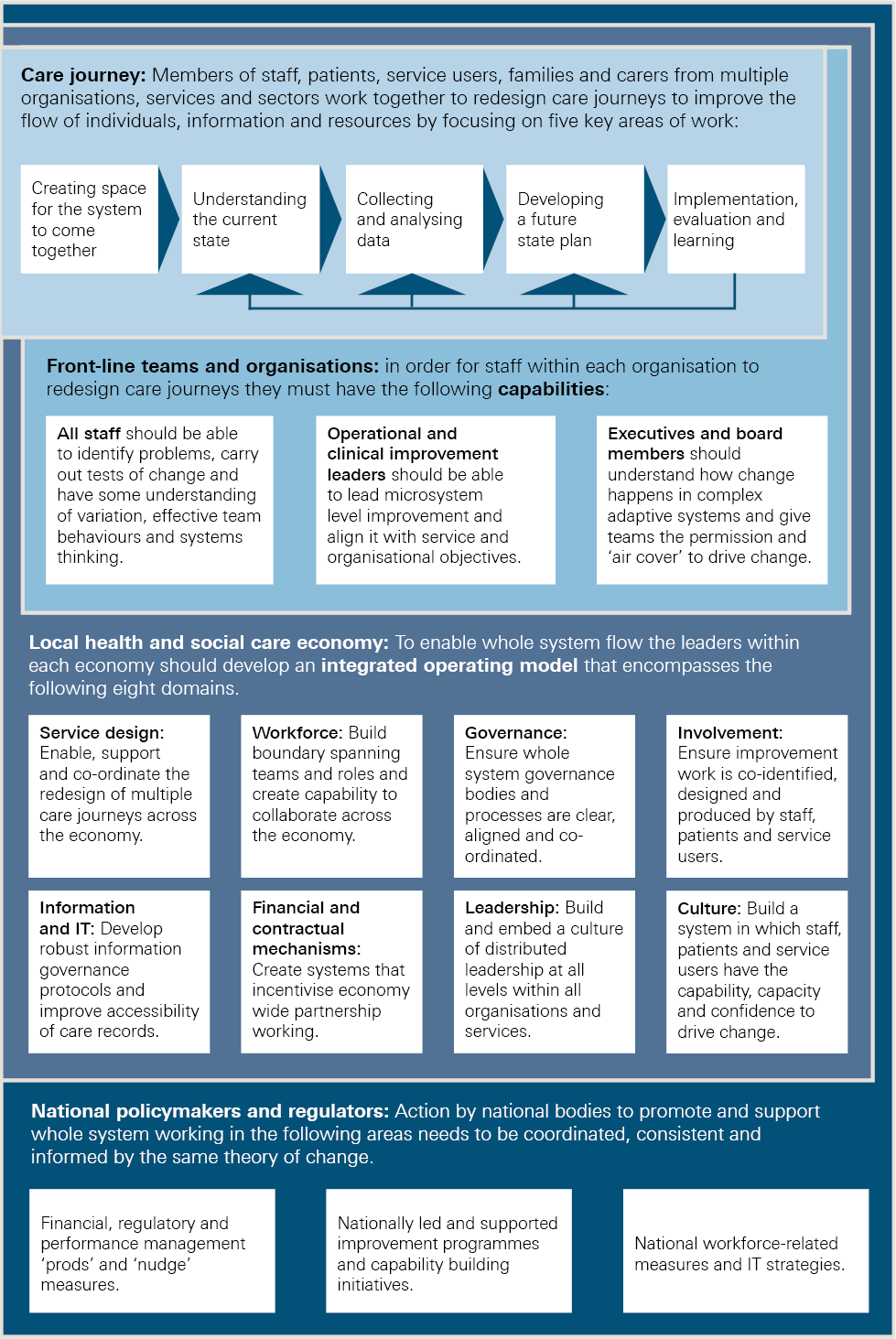
Care journeys
In looking to improve whole system flow, it is important for the work to be underpinned by a sound understanding of what it is like for patients and service users as they flow from one service to another. Anyone who requires care for acute or chronic conditions is likely to have a care journey that crosses multiple professional and sectoral boundaries in both community and institutional settings.
Focusing on the experiences of patients and service users will not only help to reveal examples of waste, delay and duplication within care processes, it will also ensure that priority is given to the aspects of care that matter most to those receiving it. After all, the overriding purpose of any effort to improve whole system flow should always be to provide an improved experience and better outcomes for patients and service users.
Getting care journeys to flow more smoothly at every point, so that patients and service users have a good experience, regardless of which team or service is providing their care, is a considerable challenge. As has already been noted, most efforts to improve flow have not attempted to tackle whole care journeys, but have concentrated on the in-hospital element. There is a pressing need to broaden the focus of attention to cover every team, service, profession and organisation that has a role to play in the care journeys of patients and service users.
Front-line team and organisational capabilities
The care journey level is the primary focus when thinking about improving flow, but it is also important to think about the contribution of each front-line team along that journey. Womack and Jones argue that for systems to operate effectively, each step in the process must be ‘capable’, so that it produces a good result every time.
If parts of the system are under-resourced or poorly designed, then well-meaning efforts to create flow may only lead to a slightly more joined-up collection of dysfunctional processes. For example, a hospital’s emergency department and wards may be operating effectively, but if social work support or community nursing teams are under-resourced or ineffective then waste and delays are inevitable. Similarly, efforts to strengthen out-of-hospital care might founder unless hospital pathways have been redesigned to prevent avoidable admissions, minimise length of stay and promote recovery. As the theory of constraints suggests, a chain is only as strong as its weakest link: movement along a process, or chain of tasks, will only flow at the rate of the task that has the least capacity.
This means that investment in continuous quality improvement at the team or unit level is vital. As well as having the right skills and resources, teams need to be able to work effectively alongside each other. For this to happen, teams at each part of the care journey ideally need to understand the same improvement language, and have experience of using similar improvement methods and tools. A shared understanding of what the system is and what the teams are collectively trying to achieve is also key. Experience among those that have developed successful approaches to integrating care shows that the co-location of staff from different disciplines and agencies can be helpful in breaking down cultural barriers.
It is also important to recognise that an understanding of improvement methods and tools at team level is not enough in itself to secure meaningful change., It has to be accompanied by willingness and capacity to spend time studying the system and identifying the constraints preventing effective flow. Understanding what matters to patients and service users, and focusing on how to improve their experiences, is also critical. Change programmes that focus largely on the spread and uptake of tools and techniques will often only achieve minor process improvements that are hard to sustain. The improvement journey of Winona Health in the US, which is explored in Case study 4, illustrates this point well. Winona’s information approach has shifted from one that was largely focused on tools and projects in its early years, to one that now focuses on ‘deep cultural change’ across the organisation and understanding what matters most to patients and the wider community.
Any attempt to improve whole system flow across an entire local health and social care economy needs to be underpinned by an effective infrastructure for collaboration. Financial incentives and contracting arrangements, information governance, service models and workforce challenges all need to be tackled. These issues cannot be addressed successfully by local system leaders without attention being paid to leadership, culture and the effective engagement of staff, patients, service users and communities. Failure to tackle them will inevitably frustrate efforts to improve the flow of patients, service users, staff, information and resources across organisational and sectoral boundaries.
As things stand now, the barriers to effective collaboration across organisational boundaries probably outweigh the enablers. At a time of severe financial pressures and mounting demand, many organisations and services are, perhaps understandably, more focused on dealing with their own immediate crises rather than the needs of the entire local health and social care economy. When opportunities for collaborative working among system leaders do emerge, it is not uncommon for the conversation to be dominated by structural and governance issues, rather than the deeper question of how to improve the relationship between the processes and teams within the economy.
Part of the problem is that emerging partnerships are often unable to dedicate sufficient time and resources to make the most of their collaboration. Participants hardly ever get the chance to get to know each other before embarking on a series of formal meetings and negotiations. Yet informal conversations are often crucial in building strong, trusting relationships and in surfacing concerns and potential obstacles at an early stage. Having the right skills to collaborate with others or to facilitate collaboration is essential: good intentions alone are not enough.
To achieve genuine whole system flow, local health and social care economy leaders need the capability and capacity to collaborate effectively and focus on the key issues this report has already described.
National system change levers
In what is still a highly centralised health and social care landscape, national bodies across the UK have a pivotal role to play in creating the right conditions for local change and helping to maintain its momentum over time. The activities they undertake tend to fall into three categories:
- First, national bodies have the ability to ‘direct, prod, or nudge’ local organisations into change through the financial, regulatory or performance management levers at their disposal.
- Second, they can support change through nationally led programmes or by investing in local improvement and leadership capability. However, to date, rather more attention and resources have been expended, in England at least, on ‘exerting regulatory control than on supporting improvement’.
- The third way in which national bodies can influence change is through the national mechanisms governing the training, recruitment, employment and regulation of people who work in the health and social care system.
A key challenge for national bodies is to ensure that the levers they deploy are aligned. In England, for example, measures to promote whole system working through Sustainability and Transformation Plans (STPs) and new models of care have to be backed up with regulatory and performance nudges that are informed by a shared understanding of how to achieve change. Ideally, they should also be designed, planned and introduced in a joined up way. Action by national commissioners and support and oversight bodies (eg NHS England and NHS Improvement) needs to be in sync with the action taken by regulatory bodies (eg the Care Quality Commission) to monitor, regulate and inspect services. In some cases, national programmes are up and running before regulators have been able to develop a strategic response and turn it into a comprehensive and integrated set of activities. Meanwhile, measures that were developed for a different purpose and are now outdated – for example, the Payment by Results tariff system – need to be reviewed, as they could undermine the drive towards integrated working. Equally, action is required at national level to help address regional and sector-related staff shortages, as well as the high levels of staff turnover and reliance on temporary or agency staff, which could seriously impede local change strategies.
Crucially, national bodies across the UK have a responsibility to provide local system leaders with the time and space they need to deliver genuine transformation. At present, there is risk of a disconnect between an understandable focus from regulators on short-term performance and the long-term steps that health and social care economies need to take to deliver sustainable change. This question will be explored in more detail in Section 6.1.
Case study 1: The Flow Cost Quality programme
The Flow Cost Quality programme, which ran from 2010 to 2012, involved two trusts in England: Sheffield Teaching Hospitals NHS Foundation Trust and South Warwickshire NHS Foundation Trust.
The programme was set up to help the trusts examine their emergency care pathways and to develop ways in which capacity could be better matched to demand, thus preventing waste and poor outcomes for patients. Both trusts were encouraged to use a structured problem-solving methodology – the lean A3 improvement process – which is designed to enable teams to identify, frame and then act on problems and challenges. The process takes its name from the A3-sized problem-solving charts developed by engineers at Toyota. ‘A3 thinking’ has been described as being ‘the key to Toyota’s entire system of developing talent and continually deepening its knowledge and capabilities’. The approach encompasses a set of structured steps to:
- describe the scope of the issue or problem and the measures for improvement
- understand the current state from both the providers’ and customers’ perspectives
- collect and analyse data to better understand the nature of the problem
- develop a ‘future state’ plan with non-value adding activities being eliminated and a smoother flow established
- agree and implement a programme of improvement projects to implement that plan using a rapid cycle of ‘plan, do, study, act’ (PDSA) to test out potential improvements
- continuously monitor progress, evaluate results and feed back learning.
One version of an A3 working document, which is designed to be updated by teams after each iteration, is set out in Figure 4.
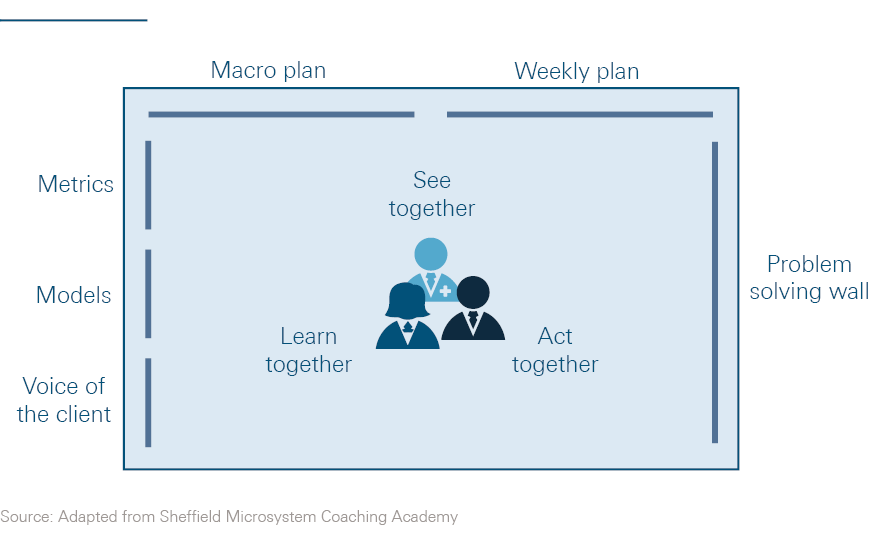
In Sheffield, there was an emphasis on bringing key stakeholders from across the pathway together in the same place to work collectively on identifying and solving problems. This was known as the ‘Big Room’ approach – or by the Japanese term ‘Oobeya’. The participants in each weekly meeting included clerks, secretaries and managers, as well as clinicians and allied health professionals from acute, primary, community and social care settings (see Figure 5).
Attendance was voluntary, and facilitators endeavoured to create an open, honest and collaborative atmosphere in which each individual, regardless of their position in the hierarchy, felt empowered to contribute on an equal footing. Attendees were also encouraged to see the Big Room as part of a process of continuous improvement, through which they would discover their way to a solution through small tests of change, rather than a discrete time-limited project geared towards implementing a pre-ordained solution.
The Flow Cost Quality team in Sheffield focused on the care of frail older people. They identified significant delays in patients being referred to hospital as an emergency by GPs and subsequent delays at each stage of the process. As a consequence, two-thirds of frail older patients arrived on the medical assessment unit after 6pm in the evening when there were fewer senior staff available to assess them. Most had to wait until the following morning to receive a review by a senior clinician.
The team implemented a range of changes to reduce batching and delays and to improve the quality of care. These included the introduction of a frailty unit, which brings together in one place all of the specialist medical, nursing and therapist staff who deal with frail older people. The team also developed an innovative model known as ‘discharge to assess’, which allows frail older patients to be discharged home as soon as their acute medical needs have been met. Within a few hours of the patient’s arrival at home, the trust’s community staff assess their continuing care, equipment and ongoing rehabilitation needs.
The team in South Warwickshire, meanwhile, worked on emergency care for all adult patients. As in Sheffield, they began by mapping processes and testing changes using a PDSA approach. Innovations included ways of matching consultant availability to variation in demand, and bringing senior clinical assessment closer to the start of the process. There was a particular focus on ensuring that support processes were capable and aligned in order to facilitate flow. For example, the number of same-day blood test results available on ward rounds was increased from less than 15% to more than 80%. Because of these up-to-date results, consultants were able to make quicker and safer clinical decisions for patients.
The Flow Cost Quality programme produced encouraging results in both trusts, which have been sustained over time. Moreover, the improvement approach underpinning this success has been spread more widely across the trusts and the local health and social care system.
In Sheffield, the ‘discharge to assess’ model – which began with a small test of change with one patient on one ward – has now been spread throughout the city’s hospital system. More than 10,000 patients have now been transferred out of the hospital into a service called ‘active recovery’, which is a health and social care collaborative aimed at ensuring that their needs are met and addressed in real time. This has resulted in a reduction in the length of time from completion of medical care to home support from 5.5 days to 1.2 days. The Big Room process, meanwhile, is now being used to help improve flow along a series of other care pathways within the city. It has also spread to Wales, where it has proven to be one of the most widespread and valued elements of the Welsh 1000 Lives Patient Flow programme.
South Warwickshire has reported a nine-point fall in mortality rates from 1.11 in 2011/12 to 1.02 in April 2015. Over the same period, the length of acute stay for all patients fell from 7.7 days to 6.2 days, while the reduction for patients aged over 75 was even greater – down by 3.1 from 12.6 days to 9.5 days. Crucially, this reduction in length of stay has not been accompanied by an increase in emergency readmissions. The trust has also managed to cut the proportion of patients who had to make more than three bed moves during their time in hospital from 14% to just 2% between 2011/12 and April 2015. It has also developed its own successful discharge to assess initiative, which is built on effective partnership working with local primary, community and social care providers.
Figure 4: The ‘A3’ chart (not necessarily on A3 paper)
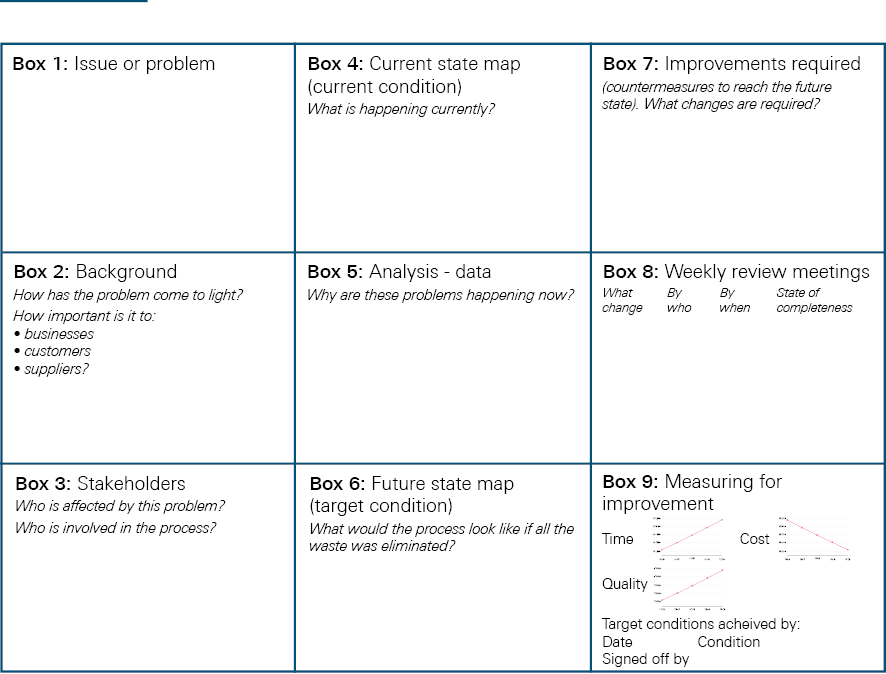
Figure 5: The Sheffield ‘Big Room’
** An effective health and social care system is one in which individuals are able to engage with services at a time and in a place that is appropriate to their needs and wishes. While each journey is different, it is possible to identify some common processes which are amenable to standardisation and can deliver improved flow.
†† The suite of programmes and guides on whole systems working that were developed by the NHS Modernisation Agency and the NHS Institute for Innovation and Improvement, highlighted in Section 1.1, are good examples.
‡‡ For example, by 2012, Sheffield had achieved a 37% increase in patients who could be discharged on the day of admission or the following day with no increase in the readmissions rate. The trust also reported a decrease of in-hospital mortality for geriatric medicine of around 15%. Further results can be found on pages 34-39 of Improving patient flow. www.health.org.uk/publication/improving-patient-flow
§§ For a description of how to use the A3 chart, see pages 16-17 in the Health Foundation report, Improving patient flow: how two trusts focused on flow to improve the quality of care and use available capacity effectively. www.health.org.uk/publication/improving-patient-flow
Care journeys
Redesigning care journeys
Anyone who has been a patient or service user, or supported a family member through an episode of illness, will know that we do not have a perfectly designed health and care system. At times it feels like it is for patients, service users and families themselves to ‘join the dots’ and make connections between agencies, rather than being supported to do so by the system. This is a reflection of the fact that the system has typically not been ‘designed’ at all. It has evolved over time in various ways, dependent on local history and circumstance. This also puts considerable stress and burden on members of staff, who need to make sense of ill-defined, fragile and often chaotic systems while managing the workload associated with them.
Ideally, in every care journey there would be a chain of interconnected processes, which have been deliberately designed and managed to meet the needs of patients and service users and to maximise flow and reduce waste, delays and duplication. It should be clear who has responsibility – both for managing the overall process and for the clinical management of each patient or service user. This would help ensure an appropriate and effective flow of information and resources.
In their book Lean solutions, Jones and Womack argue that many of the same disciplines and methods that have yielded improved quality and productivity in manufacturing can also transform the outcomes and experience of consumers in complex service environments such as health care. They set out the following principles of ‘lean consumption’ from the customer’s viewpoint:
- Solve my problem completely.
- Don’t waste my time.
- Provide exactly what I want.
- Deliver value where I want it.
- Supply value when I want it.
- Reduce the number of decisions I must make to solve my problems.
In the health and social care context, we should also add ‘engage me as a full partner in my own care’, with a view to ensuring that efforts to improve the quality of care are co-identified, co-designed and co-produced by those providing and using services.
In recent years, the level of time and resources given to capturing the opinions and experiences of patients and service users about their care has grown appreciably: surveys, online feedback and focus groups are now commonplace in health and social care. The use of patient shadowing techniques and observation of patient and professional engagement is also on the rise. But it is still unusual to find examples of service redesign projects that have been shaped and driven from the start by patients or service users, operating as active and equal participants in the change process., Given that all services, unlike goods, demand some form of interaction between those providing them and those using them, and as such are ‘co-produced’, there is a pressing need to address this deficit.
The Health Foundation’s Flow Cost Quality programme was a concerted attempt in the NHS to address the challenges identified by Jones and Womack. The programme set out to improve patient flow along the urgent and emergency pathway in two NHS foundation trusts in England (see Case study 1). Much of the learning from the programme is highly relevant for communities wishing to tackle the topic of improving flow on a genuinely whole system basis. It demonstrates that a combination of lean approaches, strong system leadership and broad stakeholder engagement can be employed to reshape health and social care services and deliver sustained productivity gains and improved patient outcomes and experiences.
However, there are additional challenges that need to be addressed when attempting large scale change across multiple settings and stakeholders in local health and social care economies. These are discussed in Section 3.2.
Using a structured approach to improve flow
As described in Case study 1, the A3 problem-solving process was one of the key methods used by Sheffield and South Warwickshire to help them analyse their systems and develop tests of change as part of the Flow Cost Quality programme. As well as helping the teams to understand the root cause of problems and test solutions, it proved to be a powerful method for changing the beliefs and behaviours of those involved. It can be adapted for use on a whole system basis by addressing five key areas of work:
- Creating space for the system to come together
- Understanding the ‘current state’
- Collecting and analysing data
- Developing a ‘future state’ plan
- Implementation, evaluation and learning.
Key area 1: Creating space for the system to come together
The system described in Figure 1 gives an example of the various stakeholders in England that could be involved in providing diagnosis, treatment, care and ongoing support. A wide range of professionals employed by a multitude of agencies need to work together effectively in patients and service users’ own homes, in other community settings, and in a range of institutions including care homes, hospitals and inpatient mental health units. Some service providers will have daily contact with a few other agencies, but none are likely to see the totality of the system and how its different elements interconnect.
Making the system visible to itself is no easy task. Box 1 explores some of the methods that have been used to understand flows across organisations. Box 4 overleaf describes the process that has been set up in Wigan with a view, among other things, to giving system leaders the time and space to focus on care integration.
Box 4: Wigan Integrated Care Partnership Board
Wigan Borough established an Integrated Care Partnership (ICP) Board in 2016. This draws together key statutory partners including Wigan Council, Bridgewater Community Healthcare NHS Foundation Trust (the community services provider), 5 Boroughs Partnership NHS Foundation Trust (the mental health provider), Wrightington, Wigan and Leigh NHS Foundation Trust (the local acute hospital), Wigan Clinical Commissioning Group (CCG) and GP representatives from five geographically based primary care clusters that cover the whole community. These partners are committed to working together to provide more joined-up services for the local population.
There has been early recognition by the ICP Board that they need to engage with a much wider range of partners. Consequently, a stakeholder forum is being established to encompass education, housing, the criminal justice system, the ambulance service, and voluntary and community organisations, as well as other primary care providers such as dentists, pharmacists and opticians. The council already has a number of well-developed mechanisms for engaging citizens in its work, both individually and collectively, and these are to be used as the partnership seeks a new deal with local people, through which the council, businesses and residents work together to improve the borough. A key element of this work is an increased focus on wellness and prevention, as described in Case study 3.
Many communities have similar arrangements to Wigan for drawing together partner organisations. However, there is a risk that they fail to reconcile the competing perspectives, values and assumptions of the partners, and are unable to develop a shared view of the problem to be addressed. The use of a structured method such as the A3 can help guard against this by creating a common vision, goals and approach to improvement. In this way the system not only becomes ‘visible to itself’ but is aligned towards a shared purpose.
The value of these methods hinges, as we have stated, on the time, resource and commitment that participating members are prepared to invest in them. Building trust between people working in different organisations and professions takes considerable time and effort. Each participant needs to approach the exercise with a degree of humility – they must recognise that no single organisation has the capacity, insight or authority to solve a system-wide challenge on its own. This is particularly important in the health and social care world, where historic resource, power and prestige imbalances between organisations and professions can make it difficult to ensure that each participant enters the collaborative process on an equal footing. Highlighting the unique expertise and knowledge that each participant brings to the process, and the particular challenges they face in their part of the system, can help in this respect. It gives each organisation the opportunity to demonstrate that many of the challenges they face are more entrenched and multi-faceted than their partners may have realised, and that they cannot be solved simply with more resources or by a technical fix.
Ensuring that participants have the necessary skills to maximise the impact of any collaboration is also crucial. These skills include the ability to make connections between your own work programmes and strategic priorities, and those of others; a willingness to operate in networks that do not have clear rules; and a capacity to identify and strengthen shared values. However, these attributes have not always been given the priority they deserve in the training and recruitment practices of health and social care organisations. Yet, in an increasingly interconnected and interdependent world, they are essential skills for the health and social care workforce – a necessity, not a luxury.
Key area 2: Understanding the ‘current state’
A key step in moving towards improving whole system flow across an entire health and social care economu is to understand what is happening at present. There are a variety of approaches that can be used to achieve this, including process mapping, hand-off charts and collecting data on waits, delays, turnaround times and other process measures.
As well as these ‘technical’ tools, this phase may also include an assessment of the economy’s cultural and infrastructural readiness for change, without which any process of service redesign will have limited impact. This assessment should start with an open and honest conversation among the organisation leaders in each health and social care economy about the financial and workforce pressures they are facing, and any emerging challenges that could end up taking time and resources away from the process of change. Identifying these barriers at an early stage, as well as any major capability gaps within the economy, is an important part of the change journey. But the conversation should not focus purely on the system’s deficits: every organisation, however troubled, will possess assets that can be usefully deployed and shared.
None of this is straightforward. It takes time for individual organisations to map their assets and deficits and even more time for the economy as a whole to take stock of what has been identified and what the implications are. It is important for local leaders to have sufficient time to come together, and to build the trust and understanding necessary to have detailed and frank conversations about the current state of their local health and social care economy.
These issues are explored more fully in Section 5, which looks at the eight key enablers underpinning effective whole system flow. It highlights the fact that the multiple levels of the organising framework set out in Figure 3 impact on each other and need to be addressed simultaneously in a complex real-world context.
Engaging patients and service users and their families and carers directly at this stage can also be very powerful. Womack and Jones suggested a version of process mapping undertaken from the customer’s perspective to create a lean consumption map.84 This shows waste and non-value added time expended by patients and service users and their families and carers, not just by service providers. It can generate important insights into key interactions in their journeys through the system. Addressing these can greatly improve outcomes as well as experience. The lean consumption map is likely to reveal considerable waste and duplication, which is hard to justify to those on the receiving end of service delivery. It creates an agenda for action and builds the will to make change happen.
Key area 3: Collecting and analysing data
Process mapping will identify a range of obstacles and challenges to achieving a smooth flow of patients, service users, staff, information and resources across the system. More in-depth analysis will provide a deeper understanding of the root causes of problems and help identify potential solutions that can then be tested.
Many communities lack the capability needed for this sort of analysis, especially when seeking to link quantitative and qualitative data from a variety of sources, encompassing health and social care. Some providers have invested heavily in expert data analysis units dedicated to supporting teams leading improvement work at the micro and meso system levels. However, they are the exception rather than the rule. In some organisations, a great deal of data are being generated but not translated into actionable knowledge or effective organisational responses. Often analysts’ time within the NHS is taken up with routine data reporting requests from external organisations.
Investment in analytical skills will be a critical enabler in improving whole system flow. Box 1 describes some of the methods that can be used to understand flows across organisations which could be exploited by skilled analysts.
Key area 4: Developing a ‘future state’ plan
As the current state becomes better understood at a sufficiently granular level of detail, partners will build an increasingly strong grounding to work on together to generate ideas for improvement. Often, health care organisations embark on major change programmes through the creation of a comprehensive blueprint that is imposed top-down using a programme management approach. Such a linear approach has significant limitations in the world of partnership working across a complex system.
The work of Paul Plsek and others on complex adaptive systems suggests that a more successful approach may be to generate a high-level vision and to establish a few guiding ‘simple rules’., These rules should be flexible enough to give local change agents the licence to adapt them to fit their own context. Creating a permissive working culture geared towards harnessing the ‘natural creativity’ and ‘skills and capacities of individuals in the system’ is also important. There should also be a focus on developing joint solutions to problems in which all parts of the system have a shared stake and responsibility.,
In relation to flow, some simple rules might include principles such as intervening early to prevent deterioration, ensuring that the right senior decision makers are available on a timely basis, building multidisciplinary and multi-agency teams, and making sure that the right information and resources are always accessible.
Key area 5: Implementation, evaluation and learning
Implementation is never an easy phase in any change programme. This is especially so in a complex multi-agency environment. In many cases, the process will involve a series of ‘bite sized’, microsystem-level improvement projects. Within each of these, an emphasis on collaborative reflection and shared attention to emerging outcomes can indicate what is working well and what is in need of further attention. It is essential that such projects are carefully aligned and coordinated by organisation and system leaders: first, to ensure that key staff and resources, such as improvement coaches and data analysts, are not stretched too thinly at any one time; and second, to ensure that activities are consistent with organisational and economy-wide objectives and that there is sufficient ownership of them at every level. Effective strategic oversight and coordination is also needed to ensure that piecemeal solutions – or worse still confusing or conflicting practices that could undermine system safety – are not implemented and embedded by different teams in different parts of the same economy.
In short, microsystem-level initiatives need to be supported by wider organisational and local health and social care economy changes if they are to be impactful, integrated, safe and sustainable. Again, this emphasises the interdependency between the multiple levels of the model proposed in this report. The need to engage front-line teams while at the same time redesigning care journeys across boundaries and putting in place system-level enablers is what makes establishing whole system flow a ‘wicked problem’.
A wide range of techniques may be adopted to support the implementation phase, including aspects of large-scale change methodology and experience-based design, which facilitates the deep involvement of patients, service users, carers and families. The use of rapid tests of change rather than more traditional programme management helps to focus teams on overcoming obstacles and secures quick wins that build momentum – although compliance with the principles underpinning the PDSA approach varies considerably. To help bring together the work, there is an opportunity to use the Big Room approach to establish a learning culture across the system as a whole.
There are few instances in the UK of this type of whole system redesign. One interesting example comes from the north east of England, which grew out of the work led by the former strategic health authority on a ‘North East Transformation System’ (NETS). Case study 2 shows how partner organisations in Darlington worked together to redesign dementia services to achieve improved flow across boundaries and to tackle serious quality issues.
Case study 2: Darlington Dementia Collaborative
In early 2009, five organisations responsible for providing health and social care services in Darlington agreed to collaborate to deliver large-scale change and to improve the flow of patients and service users across organisational boundaries and improve the care they were able to deliver.
The Darlington Dementia Collaborative, which had support from the start from the chief executives of the five organisations, was underpinned by a commitment to continuous improvement. One of its aims was to determine whether a consistent approach to improvement would work across organisational boundaries. As two of the organisations were already using a method based on the Virginia Mason system (see Box 2), the collaborative agreed to use this method as the basis of a training programme for senior staff across all organisations. The programme included:
- training and support in the use of lean methodologies, improvement in quality and the elimination of waste for people working on the front line
- lean methodology awareness training for senior members of staff
- competency assessment in the application of lean tools and techniques
- five-day rapid process improvement workshops and process mapping events for ‘point kaizen’ transformation in specific areas/departments/wards.
The Collaborative focused its efforts on the implementation of the then recently published National Dementia Strategy. Over a 12-month period, it reported a range of process improvements, including:
- a reduced lead time for patients to be seen by liaison psychiatry from 5 days to 1.6 days
- a reduced length of stay on the elderly medical ward at Darlington Memorial Hospital from 14.3 days to 10.2 days – achieved without an increase in readmission rates
- a 24% reduction in A&E attendances and a 17% reduction in acute admissions among four care homes involved in a rapid process improvement workshop to pilot a new way of working.
Staff feedback was also positive, reporting that the Collaborative had helped to strengthen relationships, improve communication and reduce silo working between the participating health, social care and care home providers. New ways of working have also emerged as a result of the Collaborative, such as mistake-proofing systems and processes, and staff huddles.
The model used in Darlington has now been applied by other dementia collaboratives in Harrogate, South Tees and North Tees.
Tackling failure demand
When AQuA – an NHS health and care quality improvement organisation – conducted its rapid review into whole system flow (see Appendix 1), many of the stakeholders it consulted emphasised the need to prevent people flowing into the system unnecessarily. Any redesign of care journeys needs to start ‘upstream’ and invest in wellness and prevention to reduce failure demand and help people live healthy lives.
Earlier in this report, we gave John Seddon’s description of the concept of failure demand – the demand that arises from failure to provide a service or to provide it in a timely or effective fashion. Seddon has consulted in a variety of sectors, including the commercial services sector and public sector environments. He suggests that up to 40% of the work of employees in such sectors can be taken up by failure demand. This might involve dealing with queries or complaints as a result of a defective or incomplete response to a customer request. It may also involve the need for more intensive intervention because a service situation deteriorates due to the lack of an early, effective response.
Many policymakers and health and social care managers recognise this as an enormous challenge (see Box 5). For example, many frail older people fail to receive at home the early intervention they need to treat a minor infection or illness, so they deteriorate and need admission to hospital. Once in the hospital environment they can quickly lose their ability to live independently, requiring an extended stay in hospital, and potentially a stay in residential care, which could have been avoided.
Box 5: Tackling failure demand in Scotland
Driven by a desire to design services in Scotland around what matters to people, Healthcare Improvement Scotland is developing a method to detect and understand the ‘source’ of the failure demand often created in health and social care.
This area of focus has emerged from support being provided to one of the new health and social care partnerships within Scotland and through a systems mapping process that took an ‘outside-in’ view of the integration of health and social care systems. This proposed programme of work is in the early design phase and has the following aims:
To help partnerships understand the interconnectedness of their health and social care system, including how actions taken in one part of the system (eg: to save money) can result in unintended consequences in another part (eg: increasing overall costs or adversely affecting outcomes for service users).
To help partnerships get a better understanding of where the failure demand is currently presenting in the system and to use that knowledge to ensure that redesign and/or investment is focused at the source of this failure demand, rather than the part of the system where the failure demand presents.
Case study 3: The ‘Wigan Deal’ for adult social care and wellbeing
Like many local authorities, Wigan Council has faced unprecedented reductions in government funding of its services over the past five years. Between 2011/12 and 2015/16, Wigan Council had to reduce the cost of services by more than £90m. During that period, adult social care and the council’s health functions lost £25m from its budget. In response to this, the council put in place a reform programme targeting delivery of savings at scale while at the same time improving outcomes for service users.
Stuart Cowley, Director of Adult Social Care and Health for Wigan Council, describes the approach as ‘simple but profound’. The underpinning principle is to reduce people’s dependence on traditional health and social care services and to support them to have greater choice and control, as well as increased connections with resources within their local communities.
Council staff have been through an innovative ‘deal’ training programme to help them rethink the way they relate to those who use their services. They are encouraged to hold ‘different conversations’ with residents to better understand individual needs and strengths, gifts and talents, rather than taking a traditional deficit-based approach. The ‘know your community’ strand of work focuses on developing community capacity and connecting people with needs to community-based solutions. Finally, a ‘standard work’ on ‘developing new ways of working’ has given the workforce the permission and support to be innovative and creative in return for a pledge to be positive, accountable, and embrace new ways of working.
The council has identified more than £8m in permanent revenue savings through delivering the Deal for adult social care and wellbeing. Hundreds of new-style care packages have been put in place. Meanwhile, front-line staff have greater knowledge and awareness of community provision, coupled with a willingness to move away from costly and prescriptive traditional services.
Wigan reports that there has been: increased investment in early intervention, reducing the dependence on long-term social care; a redesigned reablement service; and a fundamental review of daycare services, reducing the number of physical daycare centres from 14 to 6 across the borough. The council now has hundreds of case studies of residents whose lives have been changed by the ‘deal’ approach. It has reported that residents are registering higher levels of satisfaction in relation to their experience of council services, while at the same time the cost of many of the care packages has been cut by up to 50%.
The newly established Wigan Integrated Care Partnership Board (see Box 4) will be considering how this innovative approach can be extended to a wider range of health and care services wrapped around GP-led primary care teams. The aim is to stop people flowing into the system unnecessarily by providing more effective support for them to live independently.
Failure demand represents a poor outcome and experience for patients and service users. It also signifies the poor use of the limited resources at society’s disposal. It is important to redesign services so that patients and service users flow more smoothly through the system when an acute intervention is needed, but it is equally important to intervene early to prevent people flowing unnecessarily into the system in the first place.
There have been a number of policy and service responses to this challenge:
- First, investment in population health measures aimed at wellness and prevention.
- Second, an emphasis on shared decision making with patients (there is evidence that where clinicians and patients work together to reach an informed view on treatment options, patients will often choose less resource-intensive options than those recommended by professionals).,,
- Third, the NHS England programme to improve care for patients with long-term conditions aims to reduce failure demand by introducing risk stratification and case finding to target those patients most at risk. It aims to meet their needs through integrated community teams and promoting supported self-management of patients’ conditions.,
In local government and the voluntary, community and social enterprise sector, a similar approach known as asset-based community development has also been used. This involves identifying the resources patients and service users have – both themselves and within their community – that will enable them to live healthy and fulfilled lives and reduce their reliance on support from professionals. Patients and service users and professionals then work together as equals to co-produce services and outcomes.
The borough of Wigan, whose integrated care organisation was described in Box 4, has been working to develop such an approach, with a strong emphasis on wellness and prevention. This has taken the form of a new ‘Deal for adult social care and wellbeing’ (see Case study 3), and is now extending into other areas, including population health and integrated working between health and social care.
None of this is easy to do. As the discussion of the key areas of work shows, there are significant barriers to overcome. Addressing these challenges requires action at the front line as well as at the local health and social care economy and national levels. The following sections describe in more detail the opportunities, actions and enablers at these levels.
Front-line team and organisational capabilities
Building improvement capability within organisations
Improving flow requires organisations to build internal capability in problem-solving, data analysis and improvement methods. The two sites involved in the Health Foundation’s Flow Cost Quality programme, Sheffield and South Warwickshire, both trained front-line members of staff and leaders in improvement tools and techniques. They found that such skills were best learned in ‘real time’ as people ‘worked on the work’. A further programme, led by Sheffield, has now been put in place to enable other teams to develop the necessary capability to improve flow along care pathways (see Box 6).
The value of investing in capability building is borne out by evidence from other sectors where significant quality and productivity gains have been made by using operational excellence approaches such as lean. Toyota, for example, invests heavily in training all staff in continuous quality improvement methods and adopts a coaching style of leadership that empowers operators to solve their own quality problems. The literature on highly effective health care organisations shows that the best of these invest in training all staff in quality improvement methods and develop a leadership style that empowers staff to solve their own problems.
Engaging people working in corporate services and middle managers in quality improvement is as critical as engaging front-line clinicians. Equally, boards need to be as interested and engaged in clinical quality as they are in their organisations’ financial performance. Their attitude towards quality is important.
In lean systems, improvement activity at the level of the team or work unit is known as ‘point kaizen’ (see Case study 2). Activities of this type, such as ‘5S’ (a method for ensuring that the workplace is safe, clean and orderly and ready to play its part in flow) are seen as key building blocks for ‘flow kaizen’ – the redesign of end-to-end product pathways. The NHS Institute’s Productive Ward programme and the NHS Modernisation Agency’s ‘see and treat’ approach in A&E departments were examples of point kaizen applied in a health care setting. These team- or unit-level improvement activities deliver more limited results on their own than an approach which seeks to improve every step of the patient’s journey, but they are a necessary part of improving flow across an organisation or system.
Recent papers by the Health Foundation and The King’s Fund describe how providers in the US, Sweden and the UK that have taken an organisation-wide approach to improvement have delivered significant and sustained gains in performance. Another example, featured in Case study 4, is Winona Health, a provider organisation based in Minnesota in the US. The skills needed at every level of an organisation for such a transformation are also summarised in Box 7.
Box 6: Sheffield Microsystem Coaching Academy’s Improving Flow programme
The aim of the Improving Flow programme is to learn how to apply team coaching skills and improvement science at care pathway level in order to improve patient flow through a health care system (see Figure 6). It builds on learning from the Flow Cost Quality programme and the Sheffield Microsystem Coaching Academy (MCA), both of which have been supported by the Health Foundation. The programme is a one-year course aimed at developing coaches with the skills to work across care pathways. The key elements are:
- monthly face-to-face teaching sessions
- experiential learning – participants co-coach a care pathway team in pairs over the course of the programme and beyond
- subgroup support with an assigned faculty leader
- monthly progress reports from coaches with feedback and guidance from the flow faculty
- an online communication platform including pages to submit work and feedback
- training in quality improvement basics
The Improving Flow programme curriculum follows the established Assess, Diagnose, Treat, Review framework used in the Sheffield MCA, as well as a new pathway assessment tool focusing on the 5 V’s – Value, inVolve, Visualisation, eVidence and Vision – and the Big Room concept.
Twelve care pathway teams from Sheffield, South Warwickshire and Royal United Hospitals Bath are involved in the first cohort of the programme, which got underway in October 2015. A further cohort will begin in January 2017.
Figure 6: The flow roadmap
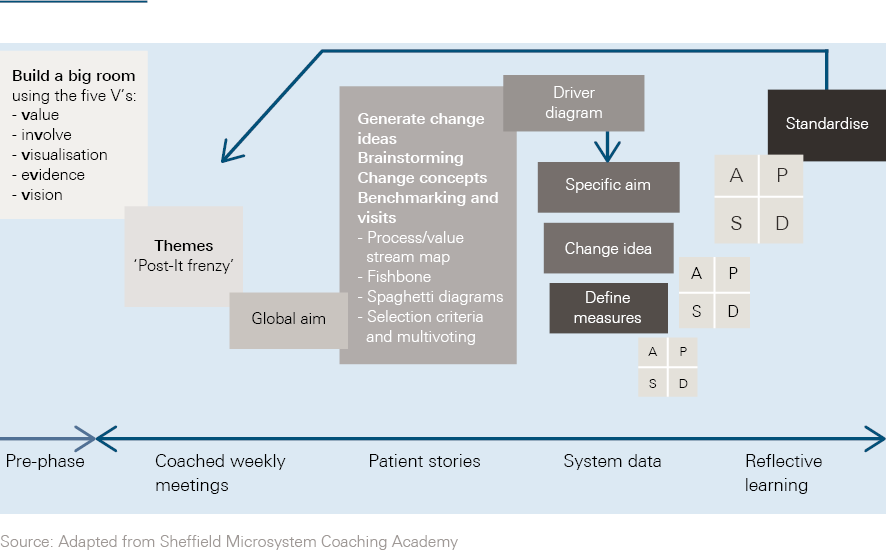
Case study 4: Winona Health Transformation programme, Minnesota, US
Winona Health is an award-winning integrated health care provider, employing 1,100 staff. Its initial efforts to implement lean for quality improvement were primarily project or tool focused, and it began a ‘deep dive’ into lean as an organisational transformation initiative in January 2008. Speaking eight years later, its president and chief executive officer, Rachelle Schultz, said ‘I can’t imagine facing the issues of health care today without the structure, philosophy, and tools of lean. Transformation work is about deep culture change and a leader needs a solid framework that combines all of those factors.’
In applying lean philosophy and processes in 2008, the organisation looked at the health system from a patient and community perspective and identified six key value streams. Winona also took steps to improve the alignment of finance, information, and clinician work flows.
The Big Room process is at the heart of Winona’s transformation strategy. This room and its processes have been continually evaluated and improved since it was put in place over five years ago. These processes are replicated through the value streams and cascaded to each department’s focus board. To connect the work of the organisation at each level, Winona uses the Hoshin Kanri (X-matrix) process. Standard methods and tools are used throughout the organisation and the aim is for there to be a clear line of sight between Winona’s strategic goals and all transformation activity at the front line.
Winona’s leaders state that embedding this new approach into the health care delivery system and organisational strategy deployment has required senior leaders to unlearn previous methods and techniques and learn lean leadership methods. This involved an uncomfortable shift from a traditional management position – where they had ‘earned the right to be autonomous’ in decision making and methods of strategy deployment – to a new and unknown role as a coach, mentor, and teacher within a health care system. It took several years for this new approach to become embedded into everyday practice.
The organisation partnered with a university in the early days to help build internal capability for continuous system improvement for leaders and managers. Teams were then supported to learn through doing improvement activities relevant to their work area. However, it became apparent that this was not enough in itself to achieve organisational transformation or deliver improvements that could be sustained over time.
Building the improvement infrastructure to support lean methods was accomplished through hands-on training and leaders being given opportunities to work outside their respective operational roles in the continuous systems improvement department for six months. This in turn supported Winona Health’s efforts to develop the capability and capacity to deploy training for improvement work across the organisation. Today, a lean leadership development curriculum, aimed at developing leadership across the organisation, is compulsory training.
Health care organisations that adopt a deliberate approach to building an overall system and culture for improvement are in the minority. There are even fewer places where this is happening across an entire local health and social care economy. However, one example is Jönköping County in Sweden, which has created a training academy known as Qulturum that brings together staff from across their whole system to learn improvement skills and work together to transform services.
Set up in 1999, Qulturum – which means ‘meeting place for quality and culture’ – has been designed to allow staff to learn together using a common improvement language. Qulturum supports system-wide and team-based improvement projects linked to the county council’s strategic aims, one of which is to improve flow and cooperation across the system. By 2008, 4,000 of Jönköping’s 9,000 staff had received training and support from Qulturum, and more than 800 measurable improvements had been reported by the county council. In Jönköping, the mantra is that ‘everyone has two jobs: to do your job and to improve your job’. Figure 7 below, drafted by Paul Batalden, encapsulates Jönköping’s approach to this concept.
Figure 7: Developing a change culture
Another example is the District Health Board for Canterbury in New Zealand. In Christchurch in 2007, the main hospital of the board regularly entered ‘gridlock’, with patients facing long waits for an emergency admission. Furthermore, the levels of growth in hospital activity were recognised to be unaffordable. Local leaders adopted an integrated, one-system approach, aiming to deliver the ‘right care in the right place at the right time by the right person’ (see Figure 8). The overarching vision was that services should enable people to take more responsibility for their own health and wellbeing, and that they should be supported to stay well in their own homes and communities for as long as possible.
Figure 8: Integrated health and social services in Canterbury, New Zealand
Underpinning this approach was a significant investment in providing staff with the skills they needed to make improvements. An interlocking suite of training and development programmes was created – Xceler8, Particip8 and Collabor8. More than 1,000 staff were trained through these programmes. They were then supported to improve the quality of work of their own team and were engaged in a wider effort to redesign overall care journeys.
Canterbury’s approach contributed to: a reduction in the number of people entering care homes; fewer cancelled admissions; and the provision of better, quicker care without the need for as many hospital visits. By 2010/11, a financial deficit had also been turned into a surplus.
One regional example of collaborative working to invest in improvement capability can be found in the north west of England. Since 2010, AQuA has been working to support its members in the region to strengthen the skills and knowledge of quality improvement at each level of their organisation. Box 7 provides a summary of the key skills identified by AQuA through this work and by the Health Foundation from an analysis of its improvement programmes.,,
Box 7: Key improvement skills required at each level of an organisation
All staff within an organisation should:
- be able to set goals, identify problems and carry out tests of change
- have a basic understanding of variation, statistics and methods of data collection
- have a grasp of improvement theory, systems thinking and effective team behaviours
- be willing and able to collaborate with other teams and professionals, and operate in networks
- be ready to put the needs of patients and carers at the heart of the change process.
Operational and clinical improvement leaders should:
- be able to lead microsystem-level improvement and apply systems theory
- be proficient in technical improvement skills and be able to make effective use of data analysts’ skills and time
- ensure that improvement activities are aligned with service and organisational vision and objectives
- be skilled in working collaboratively with other leaders with different goals and ways of working
- ensure that team members have the time, skills and permission to improve the aspects of care that matter most to patients and carers
- have the skills and motivation to co-produce change with patients and carers and ensure that their assets and strengths are used effectively.
Executives and board members* should:
- have an understanding of how change happens in complex adaptive systems
- work to develop and embed a culture of distributed leadership within their organisation, which gives clinical and operational leaders the licence and support to drive change
- build improvement capability within the organisation in a systematic way
- work with other organisation leaders to create space and time for collaboration at each level of their organisation
- provide ‘air cover’ for front-line teams working on improvement
- ensure that all team-level improvement is aligned and coordinated.
* A useful further resource for board members is NHS Scotland’s recently published guide: Quality improvement and measurement: what non-executive directors need to know. Available from www.gov.scot/Resource/0049/00492311.pdf
Wrightington, Wigan and Leigh NHS Foundation Trust worked with AQuA to develop its first 20 ‘quality champions’. The trust now has more than 200 such champions, each leading a significant quality improvement project. The trust has blended training in quality improvement methods with a concerted approach to staff engagement and has reported significant improvements, both in quality of care and in staff motivation and morale. Similarly, Aintree University Hospital NHS Foundation Trust is developing its own system for improvement known as AQUIS (the Aintree Quality Improvement System), which is a blend of improvement skills training provided by AQuA, in-house expertise on ‘human factors’, and ‘listening into action’ – a programme focusing on staff engagement.
A number of the vanguard sites and emerging accountable care organisations in the English NHS are beginning to consider how to build whole system improvement capability. This will be a critical step as they seek to improve the smooth and effective flow of individuals, information and resources across their communities. By training front-line staff and leaders in improvement methods, these systems will create the building blocks for the design and management of flow. They will also develop a common language and culture that will support staff from different professions and agencies to work together to improve care.
Creating a climate in which people working at the front line have the time, support and, above all, permission to improve the aspects of care that matter most to patients and service users can also help organisations recruit and retain staff and maintain their morale. Organisations with established improvement capability-building programmes that aim to empower staff to improve care in this way will often point to improved staff survey scores when considering the impact of their investment.
Action to build capability at the team level and within and across organisations is a critical enabler to improved system-wide flow. However, having an improvement method and a will to improve are not enough in themselves. There remain significant barriers at the local health and social care economy level that must also be tackled. These obstacles are both technical (financial, workforce and information-related challenges) and cultural (requiring new approaches to leadership, governance and engagement). Section 5 explores how these barriers can be addressed.
‡‡‡ See the glossary for details of the Hoshin Kanri (X-matrix) process.
§§§ In Sweden, a typical county health system includes primary care clinics, specialised medical services, rehabilitation facilities, and pharmacies.
¶¶¶ Paul Batalden is Professor Emeritus of Paediatrics at The Dartmouth Institute of Health Policy & Clinical Practice at Dartmouth Medical School. He also co-founded the Institute for Healthcare Improvement (IHI) in the US in 1991. He teaches about the leadership of improvement of health care quality, safety and value at Dartmouth, IHI and the Jönköping Academy
Local health and social care economy enablers
Enabling greater integrated working between local organisations
In all parts of the UK there is increased emphasis on health and social care organisations working together to tackle the growing quality and productivity challenges that all systems are facing and also to ensure that care is ‘genuinely co-ordinated around what people need and want’.
In England, this is reflected in the development of new multi-organisation care models, as envisaged in the Forward View and the requirement for NHS commissioner and provider organisations to develop longer-term, system-wide plans across newly established sustainability and transformation plan (STP) footprints. To ensure that organisational boundaries do not get in the way of change all organisations within each footprint will be held accountable for keeping within an area wide spending limit.
In Scotland, the integration of health and social care systems in April 2016 has created a significant opportunity to embed a whole system philosophy geared towards enabling people to live longer, healthier lives at home. With this aim in mind, steps are now being taken to link health and social care data to enable a better understanding of flow across the entire system. Meanwhile, a portfolio of improvement programmes – Living Well in Communities – has been launched to support people to spend more time living well at home or in a homely setting. This initiative connects a range of stakeholders , including health and social care partnerships, housing associations, third sector organisations and private sector social care providers.
In Wales, the creation in 2009 of Local Health Boards that bring together primary, secondary and tertiary care planning and delivery functions was driven in part by a desire to enable integrated working. In Northern Ireland, meanwhile, Integrated Care Partnerships have been set up to provide the infrastructure needed to underpin effective cross-sectoral, multi-disciplinary relationships.
Efforts that improve the flow of patients, service users, information and resources across these place-based systems of care could be the engine that drives real transformation in the use of resources, the quality and reliability of care, and, crucially, the experience of patients and service users. However, well-meaning attempts to redesign services across pathways will run the risk of failure unless a number of barriers are tackled by leaders within local health and social care economies.
There is experience local leaders can draw on. For example, between 2011 and 2014, AQuA and The King’s Fund worked in partnership to develop an Integrated Care Discovery Community in the north west of England. The aim was to accelerate the development of effective integrated health and social care systems while at the same time growing a new cadre of system leaders. As part of this work, AQuA identified eight enablers of effective integrated whole system working, which are described in this section. It is AQuA’s experience that these are critical to the success of redesigning care journeys to improve flow.
AQuA’s eight enablers of whole system working
1. Service design
This may involve the macro configuration of services – for example, the development of multispecialty community providers or primary and acute care systems. It includes more detailed redesign of service pathways, which are key to ensuring that individuals receive the right care, at the right time, in the right place. Innovations such as ‘discharge to assess’, described in Case study 1, offer examples of how new forms of service design can enable better flow across the system.
2. Workforce
This includes the design of new job roles, the development of integrated multidisciplinary teams and the cultivation of the necessary skills and capacity among people working at the front line to collaborate effectively across teams and organisations. In Wigan, which is one of the Integrated Care Discovery Community members, the council has developed a number of new job roles as part of the Deal for adult social care and wellbeing (see Case study 3). These aim to help residents navigate the system more effectively and to connect them to resources already available in their communities. The creation of job roles that span traditional organisational boundaries is likely to be a key enabler for improved flow.
3. Information and information technology
Information governance restrictions are often cited by front-line practitioners as one of the greatest obstacles to effective multi-agency working. To guard against possible breaches of data protection laws, some organisations have put in place highly restrictive information governance rules. Perceived differences in information governance practice between local authorities and NHS providers have also made organisations and professionals reluctant to share information about patients and service users. There is a pressing need to develop robust protocols to handle these issues while at the same time accelerating the move towards more readily accessible shared care records in order to improve continuity of care, enable faster and safer clinical decision making and improve the patient and service user experience.
4. Financial and contractual mechanisms
The current Payment by Results system in the English NHS can create barriers to innovative service redesign involving primary, secondary and community care organisations. The original intent of the tariff-based payment system was to maximise hospital-based elective procedures to tackle long waiting times. Although Payment by Results has been repeatedly adapted in light of changing priorities, it can still have the unintended adverse consequence of financially penalising hospitals for service redesigns aimed at reducing admissions.
Resource imbalances between different sectors can lead to bottlenecks developing in the flow of patients and services between services as hard-pressed teams and units struggle to cope. Many local authorities have severe funding pressures, and the impact this has had on social care in some areas has led to inevitable delays in discharging patients from hospital. Innovations in financial and contracting systems to tackle this include the development of capitation-based (per head) payment arrangements, and prime contractor or alliance contracting models to incentivise greater partnership working and to avoid hospital admission through earlier and more appropriate intervention.
These harder-edged enablers, which focus on the ‘anatomy of integration’, are ones on which system leaders most usually concentrate. However, the work of AQuA and The King’s Fund recognised that the ‘physiology of system working’ – the softer, but not easier, enablers outlined below – are equally critical.
5. Governance
Local communities often have a confusing myriad of boards, committees and working groups to support multi-agency working. The presence or absence of particular agencies from key meetings can lead to significant power differentials and can impede effective partnership working. Manchester City Council and its NHS partners, as part of the Living Longer, Living Better programme, fundamentally reframed their governance arrangements to create more coherence and stronger partnerships at the city and locality level. Ensuring that system leaders have sufficient time and space to come together and build relationships, as described in Section 3.2, is also crucial.
6. Involvement
The degree to which staff, patients, service users and residents are involved in decision making and are full partners in service redesign is a marker for the maturity of wider partnership working. As described in Section 3.1, it is important that efforts to improve the quality of care are co-identified, co-designed and co-produced by those providing and using services. Ensuring that patients and service users are active participants at every step of the change process will help to make sure redesigned services reflect and prioritise the needs and aspirations of patients, service users and the wider community.
7. Leadership
The skills and leadership style needed to climb an institutional career ladder may not be the same as those which enable success in a messy, complex multi-agency environment. In this world, there is a limit to what can be achieved through a traditional top-down style of leadership. What is needed is a distributed form of leadership that enables all teams to share responsibility for building support for change and then planning and delivering it. As Ron Heifetz put it: ‘an executive team on its own cannot find the best solutions, but leadership can generate more leadership deep in the organisation’. The fact that many of the most impactful improvement programmes in health care have emerged from professionals in the middle of the system, who then secure buy-in from their senior leaders, highlights the value of embedding a culture of distributed leadership across every system.
8. Culture
Building a learning culture in which staff, patients and service users have the capability, capacity and confidence to work together to identify problems and carry out tests of change makes it much easier to put in place the new service models and workforce designs that will be key to improving whole system flow. In thinking about change, it is also important to spend time reflecting on the lessons from previous local improvement and transformation efforts. Whatever the challenge, it is highly likely that at least one local team, service or organisation will have tried to tackle it at some point in the recent past. Learning from what worked well, as well as what failed to embed, is a necessary part of the change process. Moreover, identifying and building on familiar and trusted improvement ideas and practices is a good way for system leaders to show that they value the workforce’s existing improvement skills and experience. It also helps to ensure a sense of continuity. After all, successful adaptation is as much a process of conservation as it is of reinvention.
At present, only a minority of local health and social care economies in the UK have a purposefully designed way of operating across organisations that incorporates all eight of these enablers. Yet without concerted action in these areas, together with a coordinated approach to redesign care journeys and engage and develop front-line teams as described in Sections 3 and 4, local health and social care economies will find it extremely difficult to design and embed whole system flow.
It is a challenging task. But the growing emphasis – right across the UK – on enabling greater collaboration between organisations, sectors and professions and more place-based working has created an important window of opportunity. The interest in many parts of England in setting up accountable care organisations and the integration of health and social care in Scotland are just some of the developments that could be exploited to accelerate progress towards effective and sustainable whole system flow.
**** See glossary for details of these models.
National system change levers
The role of policymakers and regulators in improving whole system flow
Local leaders can do much to identify thestrengths and weaknesses of their local health and social care economy in relation to each of the eight enablers set out in Section 5.1. They can put in place development plans to build on assets and tackle barriers.
However, there is also an important role for policymakers and regulators in creating the conditions for effective whole system flow., As highlighted in Section 2.5, much depends on the ability of national bodies to develop and align an interlocking and coherent set of financial, regulatory and workforce measures and policies. Steps by national commissioners to promote greater collaboration between organisations, professions and sectors through vehicles such as the New Care Models programme in England need to be mirrored by reciprocal action among regulators. The Care Quality Commission’s emerging Integration, Pathways and Place programme, which has already produced some prototype place-based quality of care reports, is a welcome move in this direction.
Action on these macrosystem-level factors has to be accompanied by an appreciation that system-wide change is invariably a long, difficult process. Richard Bohmer has described the task of leading change at scale in health care as a slow, prolonged process of hard, repetitive work based on the gradual rebuilding of local operating systems. He has pointed out that many of the organisations and systems around the world that have attracted the most interest and attention, such as Intermountain in the US, embarked on their improvement journeys a decade or even several decades ago.
It is a change narrative that does not sit easily with the natural rhythm of the policy world, which is informed by much shorter electoral cycles. A key challenge for policymakers, therefore, is to ensure that the leaders of each local health and care economy have sufficient time and headspace to engage in system-wide change. At the very least, local leaders need to be given every opportunity to align medium-term objectives – such as those associated with the delivery of the Forward View in England – with local ambitions for large-scale, long-term transformation work.
There also needs to be a closer configuration between the practice of improvement and the principles that influence its commissioning, measurement and reporting. It is now widely recognised that the most successful whole system change programmes in health and social care rely on the gradual redesign of services through repeated tests of change. Most organisations would accept the need to, as Steven Spear put it, ‘discover our way to the right answer’ through a multidisciplinary process involving multiple tests of change, rather than ‘think our way to the right answer’. Moreover, many of the most successful improvement projects are driven by a desire to improve the experience of patients and service users, rather than the productivity or efficiency of the service.
Yet this approach is at odds with the prevailing discourse of public sector reform, with its ‘emphasis on speed, efficiency, product, task or outputs’. Instead of looking at how to foster the behaviours, skills, relationships and infrastructure that would help to create an environment that is conducive to change, the reform debate at national level is largely focused on the ‘solutions’ that successful systems have developed, and how they can be replicated at pace.
The nature of this debate could act as a barrier to meaningful whole system change. As John Seddon has pointed out, change programmes that are conceived primarily in order to deliver productivity savings rarely achieve the impact intended. It is good systems knowledge and design, he said, coupled with a focus on the user, that create the conditions in which process and quality improvements and productivity gains become achievable.
Consequently, the focus at national level needs to be on supporting local health and social care economies to find better ways of working together over the long term to deliver the ‘triple aim’ of improved health, improved quality of care and improved use of collective resources.
†††† Richard Bohmer is a clinician and management academic. He was on the Faculty of Harvard Business School between 1997 and 2015 and has been the Director of Clinical Quality Improvement at the Massachusetts General Hospital.
Bringing it all together
Developing a joined-up strategy to improve whole system flow
The absence of a smooth, effective flow of patients, service users, information and resources is all too apparent on a daily basis to those encountering health and care services. An inability to transfer inpatients back home as soon as their medical needs are met, or patients having to explain why they are seeking help to multiple people when they call or visit a service, are just a couple of examples of the delays and duplication that frustrate patients, service users and members of staff.
Attempts to improve flow to date have tended to focus on only a part of patients’ and service users’ care journeys, normally one including a hospital admission. There is a pressing need to look beyond the hospital and to give attention to every team, service and organisation that patients and service users encounter. Only by looking at whole system flow will it be possible to deliver the type of far-reaching and sustained improvements in quality and efficiency, as well as patient and service user experience, now expected of each health and social care economy.
Achieving this will require a joined-up development strategy operating at multiple levels. At the care journey level, the tools and techniques of lean provide helpful insights as to how to tackle bottlenecks in the flow of patients and service users between services and remove waste, delays and duplication. For this work to be successful, however, local health and social care economies also need to invest in the improvement skills and capacity of people working at the front line so that teams and work units are capable of continually improving the quality of the work they do. Local leaders must identify and address the barriers to effective whole system working that exist locally. At the same time, national bodies need to create an environment which is conducive to long-term change and the development of learning cultures among health and social care organisations.
This is a complex task. It will not be achieved easily. To deliver it successfully will require vision, determination, resilience and a significant degree of both humility and curiosity. However, the prize – in terms of better quality of care, better care health and better use of increasingly scarce resources – is immense.
Conclusions
Too many patients, service users, families and carers in today’s health and social care system are frustrated that services do not seem to talk to each other. This can cause people unnecessary delays and anxiety, and can lead to avoidable spells in hospital or in institutional care. In the worst cases, it leads to people experiencing avoidable harm and suffering.
Too many front-line staff have too much to do with too few resources. They are constantly firefighting and engaging in wasteful work as a result of poorly designed processes and endemic silo working. This is both stressful for them and has an impact on quality of care.
Too many organisation leaders lack the time and resources needed to build the type of relationships with their counterparts necessary to tackle wicked system-wide problems. Too often, leaders are required, or expected, to start delivering integrated solutions before they have had the chance to really understand the values, ways of working and expectations of neighbouring organisations, or to discuss how, and to what end, they could work together. Shortcutting the process of developing relationships and a shared vision can limit future progress.
Improving the flow of patients, service users, staff, information and resources across the health and care system has enormous potential to improve this situation and deliver a better experience and better outcomes for patients, service users and members of staff, with more effective use of scarce resources.
To achieve improved flow it is important to look at all assets, resources and services within the local health and social care economy, not just those that are delivered by health or social care organisations.
A key goal of any initiative to improve whole system flow should be to prevent individuals flowing into the care system unnecessarily (known as failure demand), through greater investment in wellness and prevention.
More effective ways of working across professional, organisational and sector boundaries need to be developed. At the heart of this process should be a focus on the needs of the people who live and work in each area, rather than the interests of the health and social care organisations based there. To ensure this happens change should be co-identified, co-designed and co-produced by the people providing services and the people they serve.
Concepts and practices from other sectors, such as lean process redesign, and simulation and modelling, have the potential to significantly improve the flow of people, information and resources across local health and social care economies. However, they need to be carefully adapted to fit the local context. Furthermore, it is important to recognise that technical expertise is not enough to drive change; the quality of relationships within and between teams and services, a readiness and capacity to collaborate across boundaries, and the ability of leaders to create a culture of discovery and learning within their organisations matter just as much, if not more.
There is a growing appetite across the UK for greater integration and collaboration between organisations, professions and sectors. But the challenges involved in doing so should not be underestimated. For any local health and social care economy, it will be a long, hard process. To give themselves the best possible chance of success, each economy needs to adopt an integrated, multi-level approach: one that combines a focus on the redesign of care journeys with an emphasis on building the capability of teams to drive and embed change, as well as concerted action on the key system-wide enablers that underpin successful integration.
Policymakers and regulators have an important role to play in creating an environment that is conducive to long-term change and the development of learning cultures in which staff, patients and service users have the capability, capacity and confidence to work together to identify problems and carry out repeated tests of change.
Recommendations
Drawing on evidence discussed in this report we recommend the following steps to improve the flow of patients, service users, information and resources across local health and social care systems.
Health and social care providers
- Make whole system flow a key corporate objective and ensure that this is reflected in all forward planning documents, organisational development plans and quality strategies.
- Develop an improvement capability building plan that aims to create the will, skills, data systems and culture needed at each level of the organisation. The plan should ensure that all types of staff (corporate and middle managers as well as front-line clinical and support staff) are exposed to key improvement approaches and tools.
- Ensure that staff have sufficient time, space and encouragement to participate in system mapping, analysis and redesign processes and activities, and consider facilitating this through the Big Room process.
- Ensure that all board members and directors receive an introduction to quality improvement, whole system flow and how change happens in complex adaptive systems.
- Review financial and performance management arrangements with the aim of incentivising flow, collaboration and effective team working.
- Work together to explore new models of collaboration such as integrated care organisations or accountable care partnerships and ensure that they are grounded by a focus on work to support improved flow.
Local health and social care economy leaders
- Put in place health and social care economy level enablers and tackle barriers to whole system flow (as described in Section 5).
- Work together to explore new models of collaboration such as integrated care organisations or accountable care partnerships and ensure that they are grounded by a focus on work to support improved flow across primary, secondary, community and social care sectors.
- Promote a place-based approach to partnership working, which puts the interests and needs of residents ahead of those of local organisations. It should also emphasise the co-identification, co-design and co-production of services to meet genuine demand and the needs and aspirations of patients, service users and the wider community.
- Commission on a whole system basis using end-to-end pathways and explore use of new financial models such as capitated (per head) budgets.
- Ensure a holistic approach to commissioning to meet the mental and physical health needs of each local population.
Regional bodies
- Regional NHS Leadership Academies and the higher and further education sector should encourage the development and dissemination of learning about effective flow management from other sectors, including manufacturing and logistics.
- In England, Sustainability and Transformation Plan Networks should ensure that the improvement of whole system flow is a key feature of new care models as these are developed. Time and resources should also be set aside to develop a shared future vision and language that extends beyond single institutions and pathway segments.
- Support organisations such as academic health science networks (AHSNs) in England, Healthcare Improvement Scotland, Public Health Wales or the proposed Improvement Institute in Northern Ireland to develop and deploy improvement capability to enhance whole system working.
Policymakers and regulators
- Recognise that improving whole system flow requires long-term focus and investment, and work towards aligning short- and medium-term planning and programmes with a long-term approach.
- In England, support the NHS vanguard sites to make the improvement of whole system flow a key feature of new care models.
- Tackle the barriers to effective system working inherent in existing financial frameworks and workforce models.
- Incentivise and support an increase in improvement, data analysis and simulation and modelling capability at local level.
- Commission further research to better understand the relative impact of in-hospital and out-of-hospital constraints on whole system flow.
- Incentivise and support the development of systems leadership skills (particularly at board level), collaboration skills and new ‘boundary spanning’ job roles.
- Promote multi-agency working across entire health and social care economies by prioritising the identification of collaborative practice during organisational inspection visits and the development of place-based reports.
- Support the independent evaluation of efforts to improve whole system flow in order to inform future practice.
Glossary
|
Accountable care organisation (ACO) |
An organisation that brings together a number of providers to take responsibility for the cost and quality of care for a defined population within an agreed budget. ACOs take many different forms, ranging from fully integrated systems to looser alliances and networks of hospitals, medical groups and other providers. ACOs emerged in the United States and they build on a much longer history of integrated care systems such as Kaiser Permanente. In England, ACOs have attracted interest as one way of overcoming fragmented responsibility for the commissioning and provision of care in the NHS. |
|
Alliance contract model |
A model that allows a set of providers to enter into a single arrangement with a commissioner to deliver services. Commissioners and providers are legally bound together to deliver the specific contracted service, and to share risk and responsibility for meeting the agreed outcomes. As such, they should be incentivised to innovate and identify efficiencies across the system, rather than solely within their organisation. The alliance is reliant on high levels of trust across its relationships. Members collectively govern the alliance through a leadership board with agreed terms of reference. |
|
Batching |
A batch system is where one action is done to multiple items or people at the same time before the next step in the process begins. In health care typical examples include the ‘batching’ of multiple blood samples for processing at the same time by a lab, or the ‘batching’ of patients to be seen during a consultant’s ward round. |
|
Big Room approach |
An approach, also known by the Japanese term ‘Oobeya’, which involves a regular standardised meeting of an improvement team. It takes place within a dedicated project room in which all the project information is displayed. Participants use the visual information to monitor data and progress, discuss issues, share experiences and agree next steps. The Big Room process offers an environment for real-time decision making that engages all relevant stakeholders. It can be used to help identify improvements to individual health care processes, with reference to their wider system impact, and then implement them successfully. It was developed by Toyota and is used by other manufacturing companies (including NASA, Boeing and Unipart) for managing new product development in highly complex, worldwide supply chains. |
|
Bottleneck |
Any resource or step in a process whose capacity is less than the demand placed on it. |
|
Capacity and demand management |
A means of addressing variations between demand and capacity in a system. Often delays and inefficiencies in the health care system are not the result of excess demand or the shortage of resources. Instead, the key issue is a mismatch between when capacity is available (ie staff, machines and equipment) and when demand presents to a service (ie the number of patients or service users requiring access to the service). If variations in demand are taken into account in capacity plans, this ensures that there is surplus capacity or ‘slack’ in the system to adjust for hourly, daily and seasonal changes in demand. |
|
Capitated payment |
A payment given to a provider or group of providers to cover the majority (or all) of the care provided to a target population, such as patients with multiple long term conditions, across different care settings. The regular payments are calculated as a lump sum per patient. If a provider meets the specified needs of the target population for less than the capitated payment, they will generate a financial gain. |
|
Failure demand |
The demand caused by failure to do something or do something right for patients and service users. The term was first coined by John Seddon, an occupational psychologist and organisational change expert, to describe the rapid growth in the volume of phone calls to banking call centres in the 1980s. He argued that this growth in demand was not an indicator of banks’ success but the result of their failure to deal effectively with customers’ queries when they first contracted them. A range of approaches to identify and address failure demand in public services have been developed by policymakers and local system leaders across the UK. |
|
Flow |
The progressive movement of people, equipment and information through a sequence of process steps. In health care, ‘flow’ generally denotes the flow of patients between staff, departments and organisations along a pathway of care. |
|
Hand-off mapping |
A method for understanding the flow of patients, service users, staff, information and resources from point A to B to C to D, etc. The objective of hand-off mapping is to eliminate hand-offs and process steps that aren’t needed so that information and processes flow through the fewest number of value-adding steps. |
|
Hoshin Kanri (X-matrix) process |
A one-page strategic plan for an organisation that includes all goals, strategies, strategic projects (initiatives) and owners. Its purpose is to encourage ownership of work at all levels of an organisation. |
|
Human factors |
The environmental, organisational and job factors, and human and individual characteristics which influence behaviour at work in a way that can affect health and safety. A simple way to view human factors is to think about three aspects – the job, the individual and the organisation – and how they impact people’s health and safety-related behaviour. |
|
Kaizen |
The Japanese word for continuous improvement. In lean systems, improvement activity at the level of the team or work unit is known as ‘point kaizen’. This is usually targeted specifically at one bottleneck and performed by a small team over a few days. Activities of this type are seen as key building blocks for ‘flow kaizen’ – the redesign of end-to-end product pathways. |
|
Lean |
A quality management system that draws on the way some Japanese car manufacturers, including Toyota, manage their production processes. The approach focuses on five principles: customer value; managing the value stream; regulating flow of production (to avoid quiet patches and bottlenecks); reducing waste; and using ‘pull’ mechanisms to support flow. Using ‘pull’ means responding to actual demand, rather than allowing the organisational needs to determine production levels. |
|
Outside-in |
An approach that is underpinned by the belief that customer or service user experiences and values are central to the success of an organisation. As a result the organisation prioritises service user engagement and focuses on improving the quality of their experiences. An ‘inside-out’ approach on the other hand is one informed by the belief that organisational success is driven by the organisation’s internal assets and capabilities. |
|
Place-based systems of care |
An approach that presupposes a shift from a ‘fortress mentality’, whereby health and social organisations look to secure their own individual interests, towards place-based ‘systems of care’ in which they collaborate with other local providers to address the challenges and improve the health of the populations they serve. |
|
Prime contractor model |
A model that allows the commissioner to contract with a single organisation (or consortium) which then sub-contracts individual providers to deliver care. The commissioner retains overall accountability for the commissioned services, while the prime contractor holds each of the sub-contractors to account individually. The prime contractor takes responsibility for designing a delivery model and patient pathway that will most effectively meet the terms of the contract. It uses the terms of the sub-contracts to stimulate and incentivise the necessary behaviours and performance it wishes to see across other providers. |
|
Process mapping |
A tool used to chart each step of a process. It is commonly used to map the pathway or journey through part or all of a patient’s health care journey, and supporting processes. Process mapping is extremely useful as a tool to engage staff in understanding how the different steps in a process fit together, which steps add value, and where there may be waste or delays. |
|
Queuing theory |
An approach that enables the analysis of waiting lines in any setting where there is a mismatch between the demand for a service and the service’s capacity to meet that demand. Queueing theory has been applied to a range of service industries including banks, airlines, and telephone call centres as well as emergency services. In health care, queueing models can be useful in identifying appropriate levels of staff, equipment and beds as well as in making decisions about resource allocation and the design of new services. |
|
Standard work |
A detailed definition of the most efficient method to produce a product (or perform a service) at a balanced flow to achieve a desired output rate. It breaks down the work into elements, which are sequenced, organised and repeatedly followed. |
|
Supply chain management |
A way of managing a network of interconnected organisations involved in the ultimate provision of product or service packages required by end-users – from point of origin to point of use. |
|
System |
A construct or collection of different elements that together produce results not obtainable by elements alone. The elements, or parts, can include people, hardware, software, facilities, policies and documents; that is, all things required to produce system-level results. In health care, outcomes are often the results of work done by many in different parts of a system and therefore result from the whole rather than any individual elements. Some systems are simple and others are complex with features whose interactions are continually changing. The level of complexity is dependent upon the number of potentially interacting elements, their interdependence, and the degree of their heterogeneity. Complicated systems can generally be understood and controlled; complex systems less so. |
|
Systems thinking |
A way of thinking used to address complex and uncertain real world problems. It recognises that the world is a set of highly interconnected technical and social entities which are hierarchically organised and produce ‘emergent behaviour’, which is more than the sum of individual behaviours. It focuses on the way that a system’s constituent parts interrelate and how systems work over time and within the context of larger systems. |
|
Theory of constraints |
A theory based on the idea that a chain is only as strong as its weakest link. It recognises that movement along a process, or chain of tasks, will only flow at the rate of the task that has the least capacity. The approach involves: identifying the constraint (or bottleneck) in the process and getting the most out of that constraint (since this rate-limiting step determines the system’s throughput, the entire value of the system is represented by what flows through this bottleneck) recognising the impact of mismatches between the variations in demand and variations in capacity at the process constraint. |
|
Toyota 3P method |
A three step method (the 3Ps being production, preparation, process) developed by Toyota in order to reduce product development time and drive down start-up costs. In health care, the 3P method has been used to inform the design and delivery of new services and facilities. The design process, from the development of an outline vision through to the production of a final detailed design, is underpinned by lean principles. |
|
Upstream and downstream |
In the context of health and social care, ‘upstream’ refers to services that patients or service users will typically encounter at an early stage in their care journey ie primary care services, or to services designed to prevent ill-health ie public health services. ‘Downstream’ usually refers to the secondary or tertiary care services that patients or service users engage with at a later stage in their care journey. |
|
Value stream mapping |
A value stream is defined as all the actions required to bring a particular service or product, or combination of them, to the customer or service user. Value stream mapping is an improvement technique derived from lean production. It is used in health care to visualise an entire process or system and the flows of patients, service users, information and resources within it, with a view to identifying, analysing and eliminating waste. |
|
Variation |
The way in which the performance of a process changes over time. There are fluctuations in all processes over time (eg, day-to-day, week-to-week, month-to-month). This variation occurs naturally and should be expected. In health care services sources of ‘natural variation’ include the times of day that emergency patients arrive in hospital, the differences in symptoms and diseases that patients present with, and staff skills and motivation. However, much of the variation that occurs in health care is ‘artificial variation’ caused by the way services are organised and delivered: sources include the working hours of staff, how staff leave is planned, the availability of equipment, and the way elective admissions are scheduled. These all vary and will have a major impact on the flow, cost and outcomes of a process. Steps to understand and eliminate this artificial variation will help to ensure that services do not react unnecessarily or inappropriately to natural variation. |
|
Wicked problem |
A problem that cannot be tackled successfully through a linear, analytical approach. It is multi-causal, unstable, socially complex, and rarely sits within the responsibility of one organisation. There is usually no single, definitive solution to a wicked problem. |
|
Wider determinants of health |
The impact on health of a person’s age, sex and hereditary factors, individual lifestyle factors, social and community networks, living and working conditions (for example; education, training and employment, health, welfare services, housing, public transport and amenities), and general socio-economic, cultural and environmental conditions. |
Appendix 1: Research and engagement approach
To inform the content of this report, AQuA and the Health Foundation undertook a range of stakeholder engagement and desk-based research activities in 2015/16.
Health Foundation’s stakeholder engagement and research exercise
In the summer of 2015, the Improvement Team at the Health Foundation carried out 15 in-depth interviews with leading academics, policymakers and system leaders working in the UK with expertise in improving flow and complex systems change. The aim of this exercise was to explore the structural, cultural and workforce-related barriers and enablers to whole system flow and to identify systems that have succeeded in improving flow across multiple services or organisations.
This engagement exercise was supplemented by desk-based research to extract and distil the learning from the following:
- Health Foundation-supported programmes and programme scoping exercises, specifically:
- The Flow Cost Quality programme in Sheffield Teaching Hospitals NHS Foundation Trust and South Warwickshire NHS Foundation Trust, 2010-12
- The Improving Flow coaching programme in Sheffield, South Warwickshire and the West of England, 2015 onwards
- The GenerationQ leadership programme, 2010 onwards
- The Health and Social Care Communities scoping project: 70 senior stakeholders were engaged and 2,000 pages of written responses to a consultation exercise were received, 2012
- Health Foundation learning reports, policy reports, evidence scans and evaluations on flow, large-scale change, networks and communities, and the context for improvement. Key publications include:
- A clear road ahead: creating a coherent quality strategy in the NHS, 2016
- Context for successful quality improvement, 2015
- The habits of an improver, 2015
- Head, hands and heart: asset-based approaches in health care, 2015
- What’s getting in the way? Barriers to improvement in the NHS: Evidence scan, 2015
- Constructive comfort: accelerating change in the NHS, 2015
- Building the foundations for improvement, 2015
- Safer Clinical Systems: evaluation findings, 2014
- Perspectives on context, 2014
- Effective networks for improvement, 2014
- Skilled for improvement? Learning communities and the skills needed to improve care, 2014
- Improving flow across organisations and pathways: Evidence scan, 2013
- Improving patient flow, 2013
- Overcoming challenges to improving quality: lessons from the Health Foundation’s improvement programme evaluations and relevant literature, 2012
- Cross-sector working to support large-scale change: Evidence scan, 2012
AQuA’s 90-day development cycle
Between January and March 2016, AQuA undertook the following research and analysis activities as part of a wider 90-day development cycle that was set up to inform its emerging Improving Whole System Flow offer in 2016/17:
- A review of the published peer-reviewed evidence and grey literature on whole system flow within health and social care and other public and private sector settings.
- Discussions with key policymakers, regulators, commissioners and improvement bodies at regional and national level across the UK.
- Discussions with AQuA’s 70 member organisations and local authorities in north-west England.
- Workshops with experts in complex system change.
- Learning visits to health and social care providers with experience of improving flow across organisations.
- A review of the learning from AQuA-led publications and programmes with a focus on integrated care and flow, such as:
- Leading in complex systems: 10 learning points for developing multi-agency leadership teams, 2016
- System leadership: lessons and learning from AQuA’s Integrated Care Discovery Communities, The King’s Fund, 2014
Appendix 2: NHS Scotland – achieving an integrated health and social care vision
The Scottish government’s 2020 vision for health and social care is to enable everyone to live longer, healthier lives at home or in a homely setting. This vision is underpinned by the National Health and Wellbeing Outcomes, which recognise the contribution that is required from a wide range of public, independent and third sector services in Scotland if this vision is to be realised.
The integration of health and social care systems across Scotland in April 2016 creates significant opportunities to overcome previous barriers to change. Integration will also enable health and social care data to be linked to support a greater understanding of the entire system.
Developing an understanding of what matters to people who use integrated health and social care services, how people ‘flow’ through or use services and how they are connected, is critical to planning and commissioning. Whole systems flow is a term often used to describe how people and systems interact within hospital settings to the point of discharge back home. However, the focus of this work recognises that home is best, and for people living within communities, a new and different language is required to define how locality based resources flow around a person within their own home and community.
Integrated systems of care
The number of people aged over 75 in Scotland is projected to increase by almost 60% by 2033 and people in this age group make up 40% of Scotland’s high-resource individuals (HRIs). Scotland’s HRIs are derived from analysis of linked individual-level data for inpatient and day-case admissions, new consultant-led and A&E outpatient attendances, and community prescribing (comprising 78% of total hospital expenditure and 90% of community prescribing expenditure). The HRI cohort comprises approximately 2% of the population but accounts for 50% of the mapped expenditure and three-quarters of all unplanned in-patient bed days, including acute, mental health, community and geriatric long stay. There is also significant turnover in the HRI cohort from one year to the next (24% remain in the top 2% for two consecutive years). There is, therefore, compelling reason to focus on the pathways these high-resource individuals follow in order to develop new pathways of care that improve outcomes.
Community-based services that anticipate need and respond quickly to prevent admission to hospital are required. Understanding what matters to people who use or need to access health and social care services may be critical in preventing, for example, unplanned admission to hospital and a potential for a delay in discharge. This demand that is created and presents within acute hospital settings may be caused by a failure to do something or do something right or different at an earlier stage when that individual was still in their own home – ie: failure demand. Understanding what causes an unplanned admission that results in a delayed discharge (the source or cause of that failure demand) is critical to understanding how health and social care systems are interconnected.
Driven by a desire to design services around what matters to people, Healthcare Improvement Scotland is developing a method to detect and understand the ‘source’ of the failure demand often created in health and social care.
This area of focus has emerged from responsive support being provided into one of the new health and social care partnerships within Scotland and through a systems mapping process that took an ‘outside-in’ view of the integration of health and social care systems.
This proposed programme of work is in the early design phase and aims to:
help partnerships to understand the interconnectedness of their health and social care system, including how actions taken in one part of the system (eg: to save money) can result in unintended consequences in another part (eg: increasing overall costs or adversely affecting outcomes for service users)
help partnerships get a better understanding of where the failure demand is currently presenting in the system and to use that knowledge to ensure that service redesign and/or investment is focused at the source of this failure demand rather than the part of the system where the failure demand presents.
Supporting the delivery of the 2020 vision
A number of pre-existing delivery programmes are already addressing whole system flow in Scotland. These are focused on tackling delayed discharge of patients from hospital, which presents a continuing challenge to delivering the 2020 vision. Tackling the root causes of problems is essential if the vision is to become a reality. As part of its approach to address this challenge, the Scottish government has established three programmes designed to have an impact on systems that may ultimately result in a delayed hospital discharge.
The Whole System Patient Flow programme contains a number of workstreams, some generated from local initiatives, but also including collaboration with the Institute for Healthcare Optimization (IHO). The programme draws upon IHO Variability Methodology® and ‘classic queuing theory’ to describe and achieve ‘optimal flow’. Four territorial health boards have well-established projects; a further six (of a total of 14) have completed a Scottish Patient Flow Assessment and are starting their own pilot projects.
The Unscheduled Care improvement programme is focused around achieving the four-hour emergency access standard across NHS Scotland through six essential actions. The 6EA improvement programme is designed to improve flow across the emergency care pathway by focusing on delivery of safe and effective care for every patient, every time. The programme adopts a collaborative approach underpinned by measurement for improvement and other QI approaches. Its building blocks involve six high-level themes that are managed individually and collectively. Since the programme’s inception, NHS Scotland measurement data show significant improvement within NHS Scotland and significant positive diversion from published data from England, Northern Ireland and Wales. The essential actions are:
- clinically focused and empowered management
- capacity and patient flow realignment
- patient rather than bed management
- medical and surgical processes arranged for optimal care
- appropriate services across seven days
- caring for patients in their own home, focusing on how care can shift from the hospital to more appropriate community-based services.
Focusing on this whole system approach has improved flow for more than 40,000 people this year; long waits of 8 and 12 hours have improved significantly, by 92% and 100% respectively.
Living Well in Communities is a portfolio of improvement programmes that aims to support people to spend more time living well at home or in a homely setting. This work involves engagement with a range of stakeholders across the health and social care landscape, including health and social care partnerships, housing associations, third sector organisations and private sector social care providers. Targeted improvement support is being provided in a number of areas, including:
- pathways for high-resource individuals
- frailty and falls in the community
- anticipatory care planning
- intermediate care and reablement
- the Buurtzorg model of care delivery.
Healthcare Improvement Scotland is building on these early delivery programmes by establishing delivery and advisory groups drawing in others with knowledge and expertise in this area. It will also seek to learn from work by academics and organisations that have developed expertise around flow, both nationally and internationally.
References
- Health Foundation. Flow Cost Quality programme. Available from: www.health.org.uk/programmes/flow-cost-quality (accessed 27 September 2016).
- Health Foundation. Safer Clinical Systems programme. Available from: www.health.org.uk/programmes/safer-clinical-systems (accessed 27 September 2016).
- Health Foundation. Improving patient flow: How two trusts focused on flow to improve the quality of care and use available capacity effectively. London: Health Foundation; 2013. Available from: www.health.org.uk/publication/improving-patient-flow (accessed 27 September 2016).
- Silvester K, et al. Timely care for frail older people referred to hospital improves efficiency and reduces mortality without the need for extra resources. Age and Ageing. 2014; 43: 472–7.
- House of Commons Health Committee. Urgent and emergency services. Second Report of Session 2013–14. HC 171; 2013. Available from: www.publications.parliament.uk/pa/cm201314/cmselect/cmhealth/171/171.pdf (accessed 27 September 2016).
- NHS England. Transforming urgent and emergency care services in England. Appendix 1 – Revised Evidence Base from the Urgent and Emergency Care Review. November 2013.
- Allcock C, et al. Constructive comfort: Accelerating change in the NHS. London: Health Foundation; 2015. Available from: www.health.org.uk/publication/constructive-comfort-accelerating-change-nhs (accessed 27 September 2016).
- Advancing Quality Alliance (AQuA). 2016-17 Prospectus.
- Bradbury E, et al. Leading in complex systems: 10 learning points for developing multi-agency leadership teams. Sale: Advancing Quality Alliance (AQuA); 2016. Available from: www.aquanw.nhs.uk/resources/integration/Leading-in-Complex-Systems-10-learning-points-for-developing-multi-agency-leadership-teams.pdf (accessed 27 September 2016).
- Health Foundation. Improving patient flow across organisations and pathways. Evidence scan No. 19. London: Health Foundation; 2013. Available from: www.health.org.uk/publication/improving-patient-flow-across-organisations-and-pathways (accessed 27 September 2016).
- Lord Carter of Coles. Operational productivity and performance in English NHS acute hospitals: Unwarranted variations. London; 2016. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/499229/Operational_productivity_A.pdf (accessed 27 September 2016).
- Monitor. Improving patient flow: Evidence to help local decision-makers. London: Monitor; September 2015. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/499229/Operational_productivity_A.pdf (accessed 27 September 2016).
- NHS England. Safer, faster, better: Good practice in delivering urgent and emergency care. A guide for local health and social care communities. London: NHS England; August 2015. Available from: www.nhs.uk/NHSEngland/keogh-review/Documents/safer-faster-better-v28.pdf (accessed 27 September 2016).
- NHS Scotland. A route map to the 2020 Vision for Health and Social Care. Edinburgh: NHS Scotland; 2013. Available from: www.gov.scot/Resource/0042/00423188.pdf (accessed 27 September 2016).
- 1000 Lives. 1000 Lives Plus and the NHS Agenda – Lessons from systems thinking. Improving Healthcare White Paper Series – No. 2. February 2011. Available from: www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/Systems%20Thinking%20-%20English%20%28FINAL%29.pdf (accessed 27 September 2016).
- Department of Health. Unscheduled Care Task Group overview. Available from: www.health-ni.gov.uk/topics/health-policy/unscheduled-care (accessed 27 September 2016).
- 1000 Lives. The Patient Flow programme. Available from: www.1000livesplus.wales.nhs.uk/flow (accessed 27 September 2016).
- NHS Scotland Quality Improvement Hub. Whole System Patient Flow Improvement Programme. Available from: www.qihub.scot.nhs.uk/quality-and-efficiency/whole-system-patient-flow.aspx (accessed 27 September 2016).
- Lewis R, Edwards N. Improving length of stay: What can hospitals do? London: Nuffield Trust; 2015. Available from: www.nuffieldtrust.org.uk/sites/files/nuffield/publication/improving-length-of-stay-for-web.pdf (accessed 27 September 2016).
- Karakusevic K, Understanding patient flow in hospitals, Nuffield Trust 2016. Available from www.nuffieldtrust.org.uk/sites/files/nuffield/publication/understanding_patient_flow_in_hospitals_web_1.pdf (accessed 25 October 2016)
- Kreindler S, Six ways not to improve patient flow: a qualitative study, BMJ Qual Saf 2016;0:1–7. Available from http://qualitysafety.bmj.com/content/early/2016/07/27/bmjqs-2016-005438.full.pdf+html (accessed 25 October 2016)
- Marmot M. Fair society, healthy lives. The Marmot Review 2010. Strategic review of health inequalities in England post-2010. London: The Marmot Review; 2010. Available from: www.gov.uk/dfid-research-outputs/fair-society-healthy-lives-the-marmot-review-strategic-review-of-health-inequalities-in-england-post-2010 (accessed 27 September 2016).
- Naylor C, et al. Bringing together physical and mental health: A new frontier for integrated care. London: The King’s Fund; 2016. Available from: www.kingsfund.org.uk/publications/physical-and-mental-health (accessed 27 September 2016).
- NHS Institute for Innovation and Improvement. Improvement Leaders’ Guide, Improving flow process and systems thinking, 2005. Available from www.nhsiq.nhs.uk/media/2594828/ilg_-_improving_flow.pdf (accessed 28 September 2016).
- Archived web content from the NHS Modernisation Agency http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/Browsable/DH_4991386 (accessed 27 September 2016).
- NHS Scotland, Patient Flow in Planned Care: Admission, Discharge, Length of Stay and Follow-Up, The Scottish Government, 2007. Available from: www.gov.scot/Resource/Doc/197953/0052905.pdf (accessed 21 October 2016)
- Pourdehnad J, Bharathy G. Systems Thinking and Its Implications in Organizational Transformation. Proceedings for the 3rd International Conference on Systems Thinking in Management, Philadelphia, May 2004.
- Ham C, Alderwick A. Place-based systems of care: A way forward for the NHS in England. London: The King’s Fund; 2015. Available from: www.kingsfund.org.uk/publications/place-based-systems-care (accessed 27 September 2016).
- NHS England. Five Year Forward View. London: NHS England; 2014. Available from: www.england.nhs.uk/ourwork/futurenhs/ (accessed 27 September 2016).
- Humphries R, Galea A. Health and wellbeing boards: One year on. London: The King’s Fund; 2013. Available from: www.kingsfund.org.uk/publications/health-and-wellbeing-boards-one-year-on (accessed 27 September 2016).
- Vize R. The revolution will be improvised: Stories and insights about transforming systems. Systems Leadership Steering Group, 2014. Available from: http://publicservicetransformation.org/resources/collaborative-leadership/906-the-revolution-will-be-improvised-stories-and-insights-about-transforming-systems (accessed 27 September 2016).
- Senge P, et al. The necessary revolution: How individuals and organizations are working together to create a sustainable world. Crown Business; 2010.
- Dixon-Woods M, Baker R, Charles K, et al. Culture and behaviour in the English National Health Service: Overview of lessons from a large multimethod study. BMJ Quality & Safety 2013; 1-10.
- Bolden R, et al. Reframing, realignment and relationships: Interim evaluation of the first place-based programmes for Systems Leadership: Local Vision. Bristol: University of the West of England; 2015. Available from: http://eprints.uwe.ac.uk/27933/ (accessed 27 September 2016).
- Cady S, et al. The change formula: Myth, legend, or lore. OD Practitioner, 2014;46(3): 32–9.
- APS Group Scotland. Commission on the future delivery of public services. 2011. Available from: www.gov.scot/resource/doc/352649/0118638.pdf (accessed 27 September 2016).
- Mitchell J. The emerging Scottish model: Avoiding everything becoming nothing. What Works Scotland; February 2015. Available from: http://whatworksscotland.ac.uk/wp-content/uploads/2015/02/WWSthinkpiece-emerging-Scottish-model.pdf (accessed 27 September 2016).
- Seddon J. Freedom from command & control: A better way to make the work work. Vanguard Consulting Ltd. 2003.
- Senge P, Hamilton H, Kania K. The dawn of system leadership. Stanford Social Innovation Review, 2015.
- Sutton S, Dixon-Woods M, Tarrant C. Ethnographic process evaluation of a quality improvement project to improve transitions of care for older people, BMJ Open 2016;6.
- Womack J, Jones D. Lean thinking: Banish waste and create wealth in your corporation. Simon & Schuster; 1996.
- Dixon-Woods M, et al. Safer Clinical Systems: Evaluation Findings. Learning from the independent evaluation of the second phase of the Safer Clinical Systems programme. London: Health Foundation; 2014. Available from: www.health.org.uk/publication/safer-clinical-systems-evaluation-findings (accessed 27 September 2016).
- SAASoft, 6M Design. Available from: www.saasoft.com/6Mdesign/ (accessed 27 September 2016).
- Scottish government. Basic Building Blocks general guidance document. Available from: www.gov.scot/Publications/2016/06/9826 (accessed 27 September 2016).
- Baboolal K, et al. How efficient can an emergency unit be? A perfect world model. Emergency Medicine Journal, 2012;29(12):972–7.
- Crilly T, Plant M. Reforming emergency care: Primary Care Trust power in action research. Health Services Management Research, 2007;20(1):37–47.
- AnyLogic. Simulation of Maternity Ward Operations. Available from: www.anylogic.com/case-studies/simulation-of-maternity-ward-operations (accessed 27 September 2016).
- Klein MG, Reinhardt G. Emergency department patient flow simulations using spreadsheets. Simulation in Healthcare, 2012; 7(1):40–7.
- NHS Institute for Innovation and Improvement. The Handbook of Quality and Service Improvement Tools. NHS Institute for Innovation and Improvement, 2010. www.nhsiq.nhs.uk/media/2760650/the_handbook_of_quality_and_service_improvement_tools_2010.pdf (accessed 27 September 2016).
- NHS Scotland Quality Improvement Hub. Value Stream Mapping. Available from: www.qihub.scot.nhs.uk/knowledge-centre/quality-improvement-tools/value-stream-mapping.aspx (accessed 27 September 2016).
- Ryan A, et al. STEPS: Lean thinking, theory of constraints and identifying bottlenecks in an emergency department. The Irish Medical Journal, 2013;106(4):105–7.
- Ford AL, et al. Reducing door-to-needle times using Toyota’s Lean manufacturing principles and value stream analysis. Stroke, 2012. Available from: http://stroke.ahajournals.org/content/43/12/3395.abstract (accessed 27 September 2016).
- Allder S, Silvester K, Walley P. Understanding the current state of patient flow in a hospital. Clinical Medicine, 2010; 10(5):441–4. www.ncbi.nlm.nih.gov/pubmed/21117373 (accessed 27 September 2016).
- Lin D, Patrick J, Labeau F. Estimating the waiting time of multi-priority emergency patients with downstream blocking. Health Care Management Science, 2014; 17(1): 88–99.
- Litvak E, Green Vaswani S, Long M, Prenney B. Managing variability in healthcare delivery. Chapter in Institute of Medicine Workshop Summary: Lowering Costs and Improving Outcomes. 2010.
- Fillingham D. Lean healthcare: Improving the patient’s experience. Chichester: Kingsham Press Ltd; 2008.
- University of Hull. Evaluation of 1000 Lives Patient Flow Programme. Unpublished report to the Health Foundation.
- Ryckman F, et al. Cincinnati Children’s Hospital Medical Center: Redesigning perioperative flow using operations management tools to improve access and safety. In E. Litvak (ed). Managing patient flow in hospitals: Strategies and solutions. Joint Commission International; 2009.
- Institute for Healthcare Improvement. Improving patient flow: The Esther project in Sweden. Available from: www.ihi.org/resources/Pages/ImprovementStories/ImprovingPatientFlowTheEstherProjectinSweden.aspx (accessed 27 September 2016).
- Deming W. Out of the crisis. MIT Press; 1982.
- James B, Savitz L. How Intermountain trimmed health care costs through robust quality improvement. Health Affairs, 2011;30(6):1185–91.
- Florida hospital saves 5.3 M dollars by adopting principles of lean manufacturing. Performance Improvement Advisor, 2005; 9(1):10–11.
- Smith C, et al. Re-engineering the operating room using variability methodology to improve health care value. Journal of the American College of Surgeons, 2013;16(4):559–68.
- Pelly N, Zeallear B, Reed M, Martin L. Utilizing integrated facility design to improve the quality of a pediatric ambulatory surgery center. Paediatric Anaesthesia, 2013; 23(7): 634–8.
- Kenney C. Transforming health care: Virginia Mason Medical Center’s pursuit of the perfect patient experience. Florida: CRC Press; 2010.
- Plsek P. Accelerating health care transformation with Lean and innovation: The Virginia Mason experience. Florida: CRC Press; 2013.
- Kaplan G. Seeking perfection in healthcare. In Batalden P (ed). Lessons learned in changing healthcare… and how we learned them. Canada: Longwoods; 2010.
- Health Foundation. Reducing harm to patients. Briefing. London: Health Foundation; 2014. Available from: www.health.org.uk/publication/reducing-harm-patients (accessed 27 September 2016).
- IHO Variability Methodology. Available from: www.ihoptimize.org/what-we-do-methodology.htm (accessed 27 September 2016).
- NHS Scotland Quality Improvement Hub. Unscheduled Care, 6 Essential Actions. Available from: www.qihub.scot.nhs.uk/quality-and-efficiency/unscheduled-care.aspx (accessed 27 September 2016).
- Institute for Healthcare Improvement (IHI). The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston: Institute for Healthcare Improvement; 2003. Available from: www.ihi.org/resources/pages/ihiwhitepapers/thebreakthroughseriesihiscollaborativemodelforachievingbreakthroughimprovement.aspx (accessed 27 September 2016).
- Spear S. Reinventing healthcare delivery. London: Health Foundation; 2012. Available from: www.health.org.uk/publication/reinventing-healthcare-delivery (accessed 27 September 2016).
- NHS Institute for Innovation and Improvement. Theory of constraints. Available from: www.nhsiq.nhs.uk/media/2760650/the_handbook_of_quality_and_service_improvement_tools_2010.pdf (accessed July 2016).
- Thistlethwaite P. Integrating health and social care in Torbay: Improving care for Mrs Smith. London: The King’s Fund; 2011. Available from: www.kingsfund.org.uk/publications/integrating-health-and-social-care-torbay (accessed 27 September 2016).
- Radnor Z, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Social Science & Medicine, 2012;74(3):364–71.
- Seddon J, O’Donovan B. An exploration into the failure of ‘lean’. Vanguard Consulting; 2015.
- Dixon J, Warburton W. NHS funding in England: money’s too tight to mention. BMJ, 2016; 354:4204.
- Care Quality Commission (CQC). How CQC is supporting the development of new care models. London: CQC; 2016. Available from: www.cqc.org.uk/sites/default/files/20160720_new_care_models_statement_of_intent.pdf (accessed 27 September 2016).
- Appleby J, et al. Payment by Results: How can payments systems help to deliver better care? London: The King’s Fund; 2012. Available from: www.kingsfund.org.uk/publications/payment-results-0 (accessed 27 September 2016).
- Buchan J, Seccombe I, Charlesworth A. Staffing matters; funding counts: Workforce profile and trends in the English NHS. London: Health Foundation; 2016. Available from: www.health.org.uk/publication/staffing-matters-funding-counts (accessed 27 September 2016).
- Shooks J. Managing to learn: Using the A3 management process. Cambridge MA: Lean Enterprise Institute Ltd; 2008.
- Downes T. Improving patient flow, experience and efficiency. Presentation to IHI International Forum on Quality and Safety in Healthcare, 14 April 2016.
- Emergency Care Improvement Programme. South Warwickshire’s whole system approach transforms emergency care. Case study 2016. Available from: www.ecip.nhs.uk/uploads/files/1/Resource/Case%20Studies/ECIP%20South%20Warwickshire%20Case%20Study%20FINAL.pdf (accessed 27 September 2016).
- Womack J, Jones D. Lean solutions: How companies and customers can create value and wealth together. Simon & Schuster; 2005.
- Robert G, et al. Patients and staff as codesigners of healthcare services. BMJ, 2015;350:g7714.
- Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Quality & Safety in Health Care, 2006;15:307–10.
- Batalden M, et al. Coproduction of healthcare service. BMJ Quality & Safety, 2015;0:1–9.
- Deeny S, Steventon A. Making sense of the shadows: Priorities for creating a learning healthcare system based on routinely collected data. BMJ Quality & Safety, 2015; 24:505–15.
- Vincent C, Burnett S, Carthey J. The measurement and monitoring of safety. London: Health Foundation; 2013. Available from: www.health.org.uk/publication/measurement-and-monitoring-safety (accessed 27 September 2016).
- Zimmerman B, Lindberg C, Plsek P. Edgeware: Insights from complexity science for health care leaders. V.H.A. Incorporated;1998.
- Plsek P, Greenhalgh T. The challenge of complexity in health care. BMJ, 2001;323: 625-8.
- Best A, et al. Large-system transformation in health care: a realist review. The Milbank Quarterly, 2012;90(3): 421–56.
- Dixon-Woods M, Pronovost P. Patient safety and the problem of many hands. BMJ Quality & Safety, 2016;25:485-8.
- Bevan H, Plsek P, Winstanley L. Leading large scale change: A practical guide. NHS Improving Quality; 2014. Available from: www.nhsiq.nhs.uk/media/2589218/leading-large-scale-change-part-1.pdf (accessed 27 September 2016).
- Taylor M, et al. Systematic review of the application of the plan–do–study–act method to improve quality in healthcare. BMJ Quality & Safety, 2013; 0:1–9.
- Hunter D, et al. A mixed-methods evaluation of transformational change in NHS North East. Health Services and Delivery Research, 2014;2(47).
- Tees, Esk and Wear Valleys NHS Foundation Trust; County Durham and Darlington NHS Foundation Trust; Darlington Borough Council; County Durham and Darlington Community Health Services; NHS County Durham and Darlington.
- Department of Health. Living well with dementia: A national dementia strategy. London: Department of Health; 2009. Available from: www.gov.uk/government/publications/living-well-with-dementia-a-national-dementia-strategy (accessed 27 September 2016).
- Coulter A. Implementing shared decision making in the UK: A report for the Health Foundation. London: Health Foundation; 2010. Available from: www.health.org.uk/sites/health/files/ImplementingSharedDecisionMakingInTheUK.pdf (accessed 27 September 2016).
- Coulter A, Collins A. Making shared decision-making a reality: No decision about me, without me. London: The King’s Fund; 2011. Available from: www.kingsfund.org.uk/sites/files/kf/Making-shared-decision-making-a-reality-paper-Angela-Coulter-Alf-Collins-July-2011_0.pdf (accessed 27 September 2016).
- Ahmed N, et al. Person-centred care: from ideas to action: Bringing together the evidence on shared decision making and self-management support. London: Health Foundation; 2014. Available from: www.health.org.uk/publication/person-centred-care-ideas-action (accessed 27 September 2016).
- Department of Health. QIPP workstreams. Long term conditions. London: Department of Health; 2011. Available from: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/Healthcare/Qualityandproductivity/QIPPworkstreams/DH_115448 (accessed 27 September 2016).
- NHS England. Enhancing the quality of life for people living with long term conditions – The House of Care. London: NHS England. Available from: www.england.nhs.uk/house-of-care/ (accessed 27 September 2016).
- Rippon S, Hopkins T. Head, hands and heart: asset-based approaches in health care: A review of the conceptual evidence and case studies of asset-based approaches in health, care and wellbeing. London: Health Foundation; 2015. Available from: www.health.org.uk/publication/head-hands-and-heart-asset-based-approaches-health-care (accessed 27 September 2016).
- Liker J. The Toyota way: 14 management principles from the world’s greatest manufacturer. McGraw Hill; 2004.
- Bevan H. How can we build skills to transform the healthcare system? Journal of Research in Nursing 2010; 15 (2) 139-148. Available from: http://jrn.sagepub.com/content/15/2/139.abstract (accessed 2 November 2016)
- Health Foundation. Celebrating shared purpose: Improvement stories from nine teams who have aligned corporate and clinical teams as part of a large-scale improvement project. London: Health Foundation; 2015. Available from: www.health.org.uk/sites/health/files/THF%20Celebrating%20Shared%20Purpose%20AW%20v2_0.pdf (accessed 27 September 2016).
- Pannick S, et al. Beyond clinical engagement: A pragmatic model for quality improvement interventions, aligning clinical and managerial priorities. BMJ Quality & Safety, 2016;25:7 16-25.
- Tsai T, et al. Hospital board and management practices are strongly related to hospital performance on clinical quality metrics. Health Affairs, 2015; 34(8):1304–11.
- NHS Institute for Innovation and Improvement. Releasing time to care: the productive ward. Available from: www.nhsiq.nhs.uk/media/2789272/pw_learning_and_impact_review_full_report.pdf (accessed 28 September 2016).
- NHS Modernisation Agency. The spread of ‘See and Treat’. Research into Practice. Summary report 11. Department of Health; 2004. Available from: www.qualitasconsortium.com/index.cfm/reference-material/service-transformation/the-spread-of-see-treat/ (accessed 27 September 2016).
- Jones B, Woodhead T. Building the foundations for improvement. London: Health Foundation; 2015. Available from: www.health.org.uk/publication/building-foundations-improvement (accessed 27 September 2016).
- Ham C. Reforming the NHS from within: Beyond hierarchy, inspection and markets. London: The King’s Fund; 2014. Available from: www.kingsfund.org.uk/time-to-think-differently/publications/reforming-nhs-within (accessed 27 September 2016).
- MCA. What is the Sheffield Microsystem Coaching Academy? Available from: www.sheffieldmca.org.uk/sheffields-approach (accessed 27 September 2016).
- MCA. The journey of a microsystem team. Available from: www.sheffieldmca.org.uk/the-journey-of-a-microsystem-team (accessed 27 September 2016).
- Region Jönköping County, Qulturum – Center for Learning and Innovation in Healthcare. Available from: (accessed 27 September 2016).
- Baker G, et al. Jönköping County Council: High-performing healthcare systems: Delivering quality by design. Longwoods Publishing; 2008.
- Gozzard D, Willson A. Quality, development and leadership: Lessons to learn from Jönköping. Improving Healthcare White Paper Series – No. 4; 1000 Lives; 2011.
- Timmins N, Ham C. The quest for integrated health and social care: A case study in Canterbury, New Zealand. London: The King’s Fund; 2013. Available from: www.kingsfund.org.uk/publications/quest-integrated-health-and-social-care (accessed 27 September 2016).
- Advancing Quality Alliance (AQuA). Building improvement capability. Available from: www.aquanw.nhs.uk/membership/building-capability.htm (accessed 27 September 2016).
- Gabbay J et al, Skilled for Improvement? Learning communities and the skills needed to improve care: an evaluative service development. London: Health Foundation, 2014. Available from www.health.org.uk/sites/health/files/SkilledForImprovement_fullreport.pdf (accessed 2 November 2016)
- Lucas B, Nacer H, The habits of an improver: Thinking about learning for improvement in healthcare. London: Health Foundation, 2015. Available from www.health.org.uk/sites/health/files/TheHabitsOfAnImprover.pdf (accessed 2 November 2016)
- Hardacre J et al What’s leadership got to do with it? Exploring links between quality improvement and leadership in the NHS. London: Health Foundation, 2011. Available from www.health.org.uk/sites/health/files/WhatsLeadershipGotToDoWithIt.pdf (accessed 2 November 2016)
- Wrightington, Wigan and Leigh NHS Foundation Trust. Annual Report and Accounts 1 April 2014 – 31 March 2015. Available from: www.wwl.nhs.uk/Library/Trust_Board/Annual_Report/WWL_Annual_Report_14-15%20Repot.pdf (accessed 27 September 2016).
- Aintree University Hospital NHS Foundation Trust. Quality Strategy – Aintree Quality Improvement System, Report Board of Directors, 29 July 2015. Available from: www.aintreehospital.nhs.uk/media/1247/board-of-directors-meeting-july-2015.pdf (accessed 27 September 2016).
- NHS England. The forward view into action: New care models: support for the vanguards. London: NHS England; 2015. Available from: www.england.nhs.uk/wp-content/uploads/2015/12/acc-uec-support-package.pdf (accessed 27 September 2016).
- Dawson J, West M. Summary of key research findings from the NHS staff survey. 2016. Available from: www.nhsstaffsurveys.com/Caches/Files/ST15%20NHS%20Staff%20Survey%20summary%20of%20research%20findings.pdf (accessed 27 September 2016).
- NHS England and NHS Improvement, NHS Operational Planning and Contracting Guidance 2017-19. Available from www.england.nhs.uk/wp-content/uploads/2016/09/NHS-operational-planning-guidance-201617-201819.pdf (accessed 25 October 2016)
- Health Improvement Scotland iHub ‘Supporting health and social care’. Living Well in Communities. Available from: http://ihub.scot/a-z-programmes/living-well-in-communities/ (Accessed 27 September 2016).
- Lewis M, Integrated care in Wales: a summary position, London Journal of Primary Care, 2015; 7(3), 49-54. Available from: www.ncbi.nlm.nih.gov/pmc/articles/PMC4494466/ (Accessed 25 October 2016)
- Integrated Care Partnerships: Health and Social Care, Interim Impact Report 2016. Available from www.hscboard.hscni.net/download/PUBLICATIONS/icps/more_about_icps/publications/icp-impact-report-aug-2016.pdf (Accessed 25 October 2016)
- Fillingham D, Weir B. System leadership: Lessons and learning from AQuA’s Integrated Care Discovery Communities. London: The King’s Fund; 2015. Available from: www.kingsfund.org.uk/publications/system-leadership (accessed 27 September 2016).
- Advancing Quality Alliance (AQuA). System integration toolkit: Domain guides and supporting information. AQuA; 2014. Available from: www.aquanw.nhs.uk/resources/integration/integrated-care-toolkit/Domain%20Guides%20and%20Supporting%20Information%20-%20April%202015.pdf (accessed 27 September 2016).
- Gilburt H. Supporting integration through new roles and working across boundaries. London: The King’s Fund; 2016. Available from: www.kingsfund.org.uk/publications/supporting-integration-new-roles-boundaries (accessed 27 September 2016).
- Caldicott F, Information: To share or not to share? The Information Governance Review, Department of Health 2013. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/192572/2900774_InfoGovernance_accv2.pdf (Accessed 25 October 2016)
- Addicott R. Commissioning and contracting for integrated care. London: The King’s Fund; 2014. Available from: www.kingsfund.org.uk/publications/commissioning-contracting-integrated-care (Accessed 27 September 2016).
- Chreim S, et al. Change agency in a primary health care context: The case of distributed leadership. Health Care Management Review, 2010;35(2):187–99.
- Heifetz R, et al. Leadership in a (permanent) crisis. Harvard Business Review, July/Aug 2009;62–9. Available from: https://hbr.org/2009/07/leadership-in-a-permanent-crisis (accessed 27 September 2016).
- Bohmer R. Presentation to the Nuffield Trust Summit. 4 March 2016. Available from:www.summit.nuffieldtrust.org.uk/agenda-2016/2016/3/4/session-6-opening-keynote-on-the-role-of-middle-management (Accessed 28 September 2016)
- West M, et al. Developing collective leadership for health care. London: The King’s Fund; 2014. Available from: www.kingsfund.org.uk/publications/developing-collective-leadership-health-care (accessed 27 September 2016).
- Harrison M, Kimani J. Building capacity for a transformation initiative: System redesign at Denver Health. Health Care Management Review, 2009;34(1):42–53.
- The King’s Fund. Accountable care organisations (ACOs) explained. Available from: www.kingsfund.org.uk/topics/integrated-care/accountable-care-organisations-explained (accessed 27 September 2016).
- Molloy A, Martin S, Gardner T, Leatherman S. A clear road ahead: Creating a coherent quality strategy for the English NHS. London: Health Foundation; 2016. Available from: www.health.org.uk/publication/clear-road-ahead (accessed 27 September 2016).
- Ham C, Berwick D, Dixon J. Improving quality in the English NHS: A strategy for action. London: The King’s Fund; 2016. Available from: www.kingsfund.org.uk/publications/quality-improvement (accessed 27 September 2016).
- Care Quality Commission. Coordinated care. Available from: www.cqc.org.uk/content/coordinated-care (accessed 27 September 2016).
- Bohmer R. The hard work of health care transformation. The New England Journal of Medicine, 2016; 375:709–11.
- NHS Confederation. Stepping up to the place: the key to successful health and care integration. London: NHS Confederation; 2016. Available from: www.nhsconfed.org/resources/2016/06/stepping-up-to-the-place-the-key (accessed 27 September 2016).
- Health Foundation. Quality improvement made simple: What everyone should know about healthcare quality improvement. London: Health Foundation; 2013. Available from: www.health.org.uk/publication/quality-improvement-made-simple (accessed 27 September 2016).
- Institute for Healthcare Improvement, The Triple Aim: Optimizing health, care and cost; 2009. Available from www.ihi.org/engage/initiatives/TripleAim/Documents/BeasleyTripleAim_ACHEJan09.pdf (accessed 2 November 2016)