Acknowledgements
Many people contributed to the ongoing design and delivery of Q and to the development of this report.
We would like to thank in particular the team at RAND Europe, the members who have provided comments for this report and Q’s country partners. Helen Crisp provided invaluable feedback on an early draft and Johanna Cronin managed the process and provided astute editorial input along the way. We would also like to thank all the Q members that make up the community, particularly all those who have contributed to the design of Q and delivery of ongoing events and activities.
Finally, we would like to thank the Q team and other Health Foundation colleagues for their involvement, support and advice.
RAND Europe evaluations of Q and Q Lab
RAND Europe was commissioned in 2015 to undertake a mixed-method developmental evaluation of the design phase of Q. RAND was subsequently selected to conduct a four-year evaluation of the implementation phase of Q and a separate evaluation of the first Q Lab project.
The evaluation has informed iterative changes in both Q and Q Lab as work has progressed and is used alongside data and direct member feedback collected by the Q team.
The final two years of the evaluation of Q will see increasing focus on understanding the potential impact of Q on the work of members and the wider health system.
Executive summary
Widespread change is needed to make the health and care sector fit for the future. Organisations need to be able to reduce waste and unhelpful variation, and develop new models of care while securing greater focus on prevention. Achieving sustained improvement in these complex areas requires significant change leadership capacity – people capable of diagnosing what’s needed locally, applying improvement methods and learning rapidly from elsewhere.
These changes will be delivered within an environment where resources are constrained. Therefore, it is imperative that the health and care sector makes good use of the improvement ideas and expertise that already exist in every part of the UK.
Yet the well documented delay in the adoption of innovation is symptomatic of a health and care system in which sharing across boundaries is often far more challenging than it should be.

What is Q and what does it offer?
Q is an ambitious initiative, designed to support and connect those leading change efforts and to enable a more joined-up approach to health and care sector improvement in the UK.
In 2015, in response to a recommendation in the Berwick Report, the Health Foundation worked with 231 people involved in improving health and care to understand what would help them to accelerate their work. Q is the result of this process.
Three years on from the co-design phase, more than 2,500 people have joined the community and Q has evolved into a multi-strand initiative, delivered in partnership with NHS Improvement and organisations from all the countries of the UK.
Figure 1: Key elements of Q in 2018
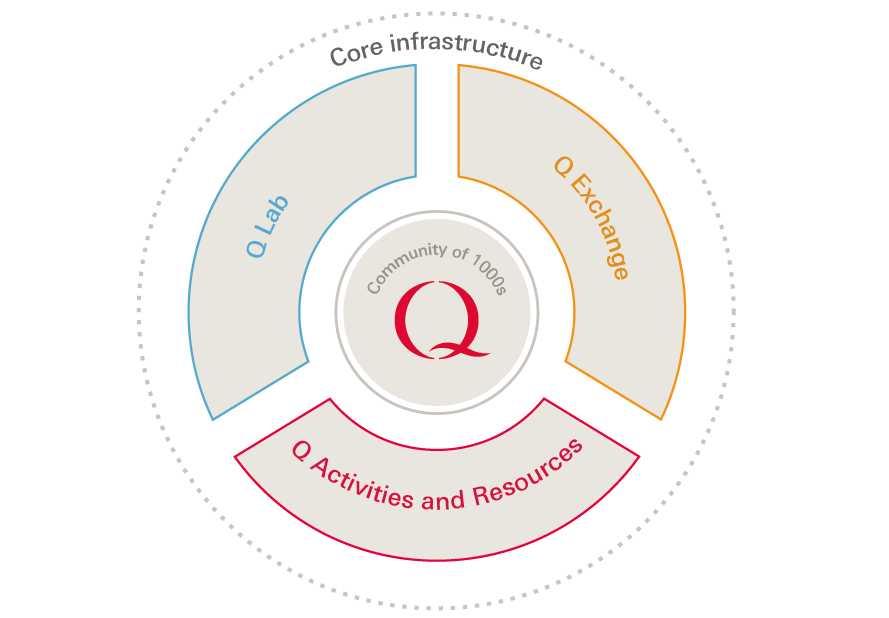
- Q’s core infrastructure attracts and connects people with improvement expertise.
- Q’s menu of activities and resources provides flexible development and networking opportunities.
- The Q Improvement Lab (Q Lab) brings together individuals and organisations from Q and beyond to make progress on a specific shared health and care challenge over 12 months.
- Q Exchange uses the collective intelligence of the community to identify and build on ideas for change. Members collectively select projects that show greatest potential to be funded, channelling funding to projects that can benefit service users and the system.
Through this interwoven and evolving infrastructure, Q aims to:
- Increase the visibility of those leading improvement efforts and the work they are doing.
- Equip members to better lead improvement work and more effectively develop the improvement capability of those around them.
- Create space for collaboration and conduits for spread to get the most from the ideas and improvement capacity available in the UK.
‘The combined workforce of the NHS is incredible, and there is almost always someone else who has been faced with the same challenge (or opportunity) and whose experience could help us, if only we could find them […] Q is a great way of facilitating these connections.’
Andrea Gibbons, Improvement Coach, Taunton & Somerset NHS Trust
Progress and learning to date
This report reflects the commitment of the Health Foundation and NHS Improvement to share progress and learning from this initiative as it develops. It accompanies the publication of the interim report of RAND Europe’s evaluation of Q and the report on the first Q Lab project (see Box 10). It summarises key messages of interest to a wider audience from the evaluation and data collected by the Q project team.
Growing Q
Q is growing rapidly and starting to give a picture of the range and location of people involved in improvement efforts. Members are from a range of backgrounds, from clinicians and quality improvement (QI) professionals to managers, researchers and policymakers, along with a small but growing number of patient leaders, charity sector professionals and staff from public services beyond the NHS.

Connecting and learning at scale
Fostering productive and creative connections is core to Q, informed by evidence that flexible networks support innovation and spread. The evaluations of Q and the Q Lab found that members are making useful connections they would have been unlikely to make otherwise. These connections are credited with improving personal resilience and enabling members to share practical learning that can in turn help organisations to avoid wasting time solving problems that have already been addressed elsewhere.
‘The real strength of Q is in its diversity. Q spans specialties and sectors, it’s UK wide and it feels like more of a movement than a top-down structure. People join because they feel passionate and want to connect and collaborate with others. Through Q, I’ve made connections with people in similar roles in parts of the UK facing similar challenges so we don’t have to reinvent the wheel.’
Dominique Bird, Head of Capacity & Capability, 1000 Lives Improvement, Public Health Wales
The aim is to offer practical and deep professional connections, that some members describe as having had a profound impact on how they work. As the community grows, increasing attention is being paid to enabling members to find people with similar interests, for example through the development of over 40 special interest groups.
‘Q enables us to see what improvement means in different sectors and gives us the ability to listen to others’ learning and spread word of our work.’
Esther Hall, Public Health Behaviour Change Lead, East Riding of Yorkshire Council
Q aims to offer a rich learning environment for those leading the complex work of improvement. Member feedback on Q’s programme of visits, community events and online resources is consistently positive. The flexible resources and activities provided through Q are intended to support peer learning between busy people. Q events are designed to be highly interactive to make the most of knowledge within the community, and Q’s tweet chats provide a virtual way for members and others to share thoughts on key texts on improvement. In parallel with Q’s directly provided activities, Q signposts members to other development opportunities and resources.
Collaborative change
The starting point for Q is supporting members with the work they are currently doing within their organisations. Significant initiatives have also been developed within Q to provide a platform for more focused change: Q Lab and Q Exchange.
The evaluation of the first Q Lab project found that the Lab has consolidated knowledge and insights on peer support as a topic, contributing to the evidence base and raising its profile. It has also created a community in peer support, giving Lab participants an opportunity to make enduring connections that supported them in their improvement work.
‘Q is here to help people share learning to improve the speed of adoption […] and to help crack some of the challenging things that haven’t been cracked before.’
Quote from RAND evaluation of Q
Q’s funding programme, Q Exchange, has seen impressive engagement in the early stages, with 181 project ideas posted online. Over 1,500 comments were posted during the initial phase, as part of this innovative model where the community support each other to improve project proposals. The projects selected with the help of the Q community are anticipated to provide a practical demonstration of the commitment to, and benefits of, collaboration.
Looking forward
Q has been designed as a long-term learning and improvement infrastructure. It responds to the insights from members during the co-design phase which highlighted the need for stable platforms that support collaboration between people working to improve care. As the number of Q connections, collaborations and change projects increases, so will the potential to further build the momentum behind Q and the numbers applying to join.
Q’s diversity of membership offers a unique mechanism for cross-sector collaboration and uptake of learning. Local and national initiatives focused on system priorities will increasingly be able to look to Q to help identify people with improvement expertise and to Q Lab, Q Exchange and a proposed insight panel to offer mechanisms for making progress on specific issues.
‘[The person I met through Q and I] found ourselves [operating at different ends of the UK] in parallel universes dealing with the same issues and shared practical information about how we were managing our issues within our teams… It’s been an invaluable professional relationship that’s allowed us to make real changes in our workplaces, and it’s honestly changed my working life.’
Ruth Jordan, Head of Continuous Service Improvement, Cardiff and Vale University

Growing Q
Making improvement expertise visible: why it matters
There are people leading work to improve services in every part of the UK health and care sector. The NHS has made concentrated efforts to build capacity within organisations and has reduced reliance on external consulting, with spending on consultancy falling from £422m to £263m between 2013/14 and 2016/17. The changes needed to make the health sector fit for the future require skilled capacity at local level, able to apply improvement methods and learn rapidly from what’s working elsewhere. And yet – perhaps unsurprisingly given the scale of the health and care sector – it is hard to know who has been trained in quality improvement, and how and where these skills are being applied.
With this in mind, before all else Q seeks to add value by making improvement work and expertise in the UK more visible. The publicly searchable online member directory for example, can help peers and system leaders find people who may be interested in supporting the delivery of service priorities.
Both the evaluation and Q member feedback to the team suggest that being recognised as part of a high-profile community helps individual members feel less isolated and offers public validation for their experience and commitment.
Who’s improving?
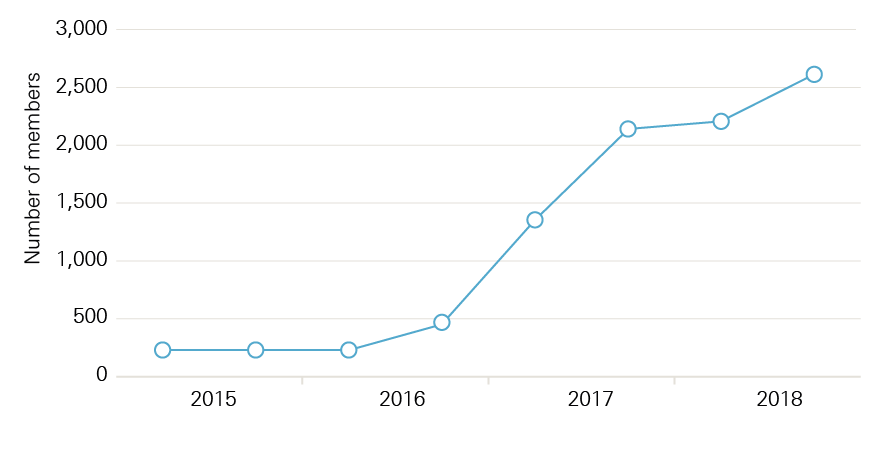
The rapid growth in the community illustrated in Figure 2 is testament to the large number of people with improvement expertise who are keen to boost and broaden what they do by working more collaboratively with others.
Figure 2: Growth of the Community from 2015–2018
‘I think, working in the NHS, it can be quite lonely sometimes. [At the Q Lab workshops…] you can kind of think out loud and explore new ideas and get support [… it] recharges your batteries, apart from anything else. The system can grind you down a little bit […] It’s good to get out of that environment a little bit and just get some ideas flowing and get some energy back.’
Quote from RAND evaluation of Q
Figure 3: Member location breakdown (primary area of work)
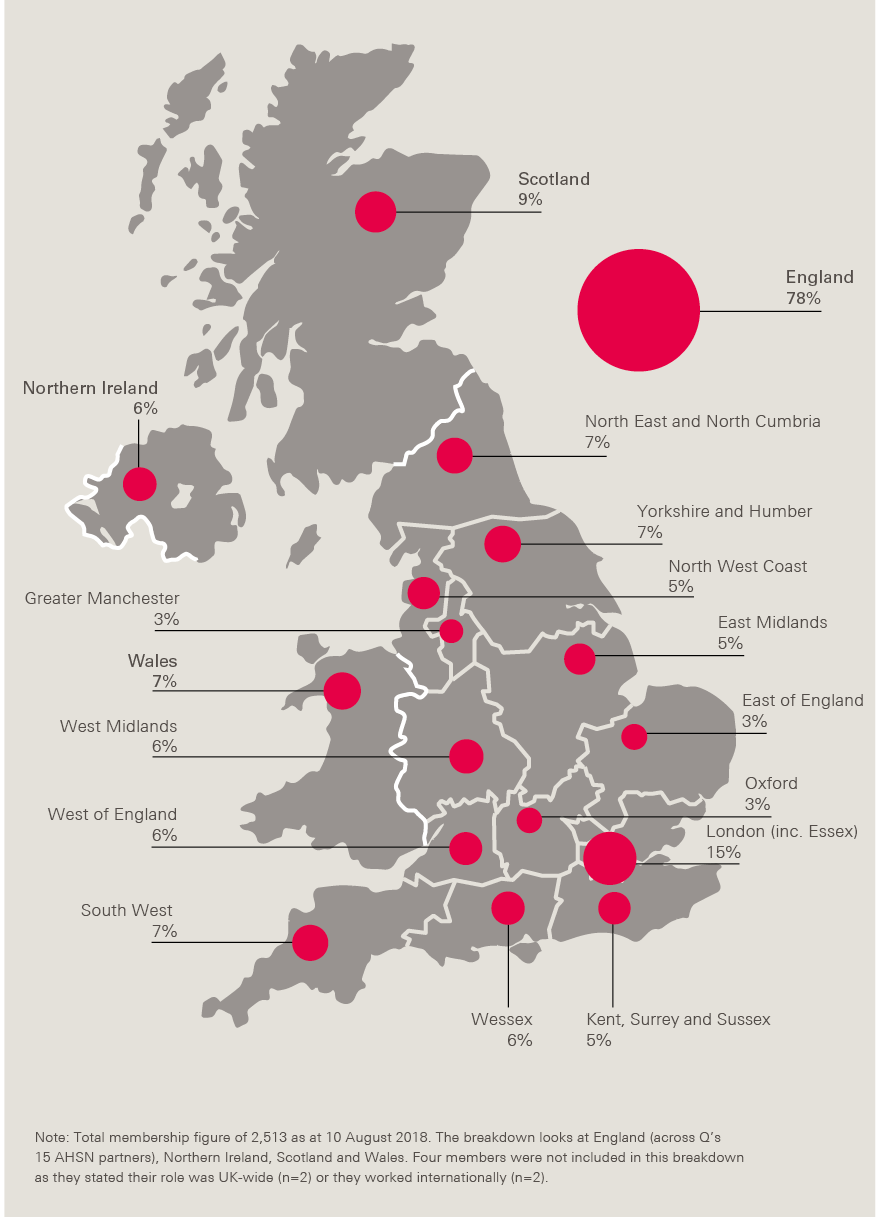
Q has attracted people from a wide range of backgrounds. 37% of members have regular contact with patients (see Figure 4) and the majority work in front-line health care organisations.
Since 2016, the Q community has seen a 4% increase in representation from the voluntary sector (5%). As at the start of July 2018, there were 59 (c.3%) members who identified being a patient leader as their primary role. There are also managers, policymakers and researchers. Figures 4 and 5 illustrate the demographic and sector diversity of the community, which the evaluation notes remained broadly consistent across recruitment rounds.
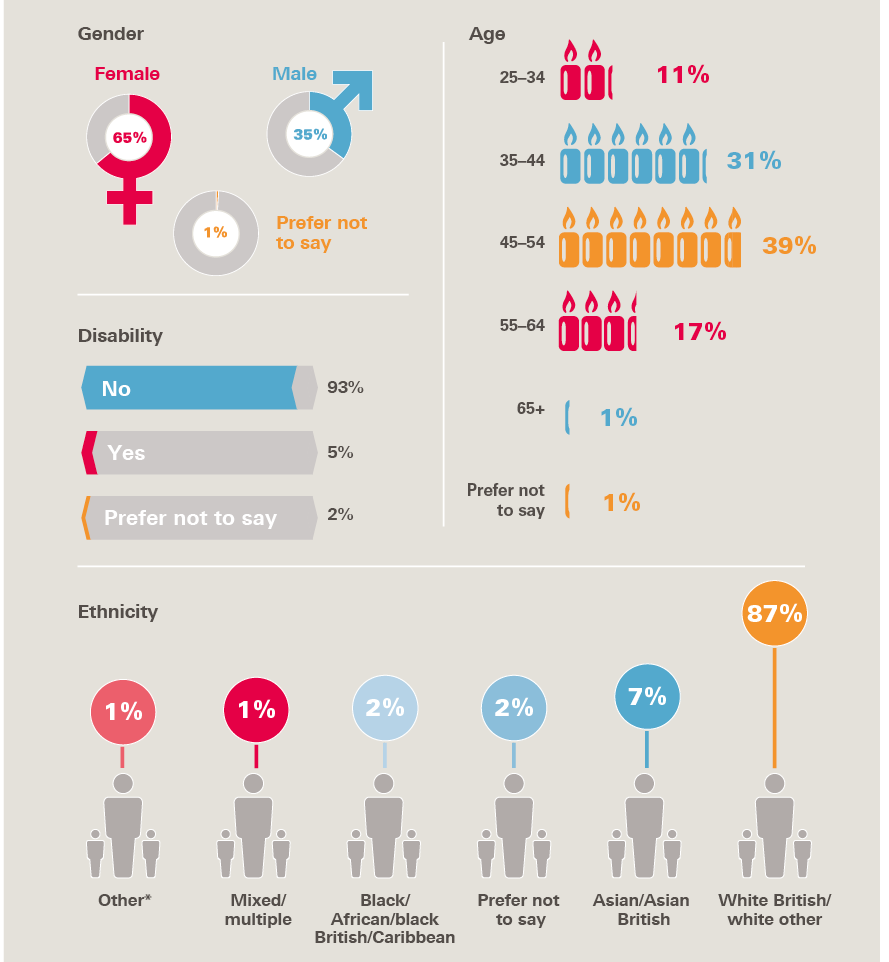
64% of the membership identify as female, broadly mirroring the gender make-up of the NHS workforce. A high proportion of members are aged between 35–54 years, likely reflective of the requirement to demonstrate significant experience of improvement to meet the selection criteria for Q (see Figure 6).
The current number of members in each part of the UK (see Figure 3) shows some interesting patterns, though this will not give a full picture of the number of people with improvement expertise in each area, as only some people will choose to join Q and the approach to recruitment has varied in different parts of the UK.
Following a regionally phased recruitment process in 2017, applications are now open on an ongoing basis to people from any part of the UK who feel they meet the criteria. As the number in the community continues to grow, and more is learned about the rich diversity of member backgrounds and experiences, Q will provide a valuable overview of who is leading improvement work.
Building a clearer picture of the improvement workforce in the UK should make it easier for organisations with responsibility for building improvement and leadership capability to plan and target development offers. It will also enable the Q team and partners to ensure that Q works to attract people from all backgrounds. The Appendix summarises the learning so far from the recruitment process.
‘I think [Q’s] got a really important and possibly essential role because it brings together people from all the disciplines and across the whole patient journey… a lot of the improvement work that I see is done in silos either within particular geographical areas or particular disciplines or interest groups.’
Quote from RAND evaluation of Q
Figure 4: Members’ face-to-face contact with patients
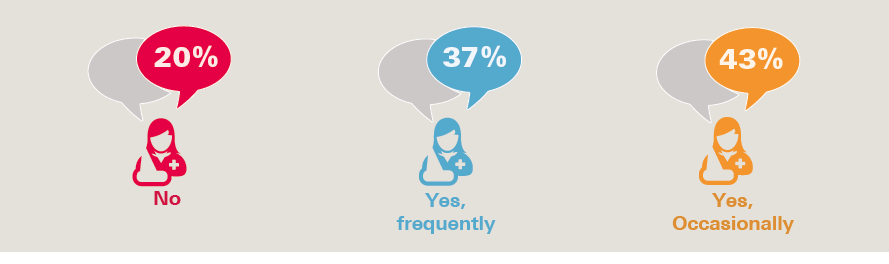
Figure 5: Members’ primary role and organisation
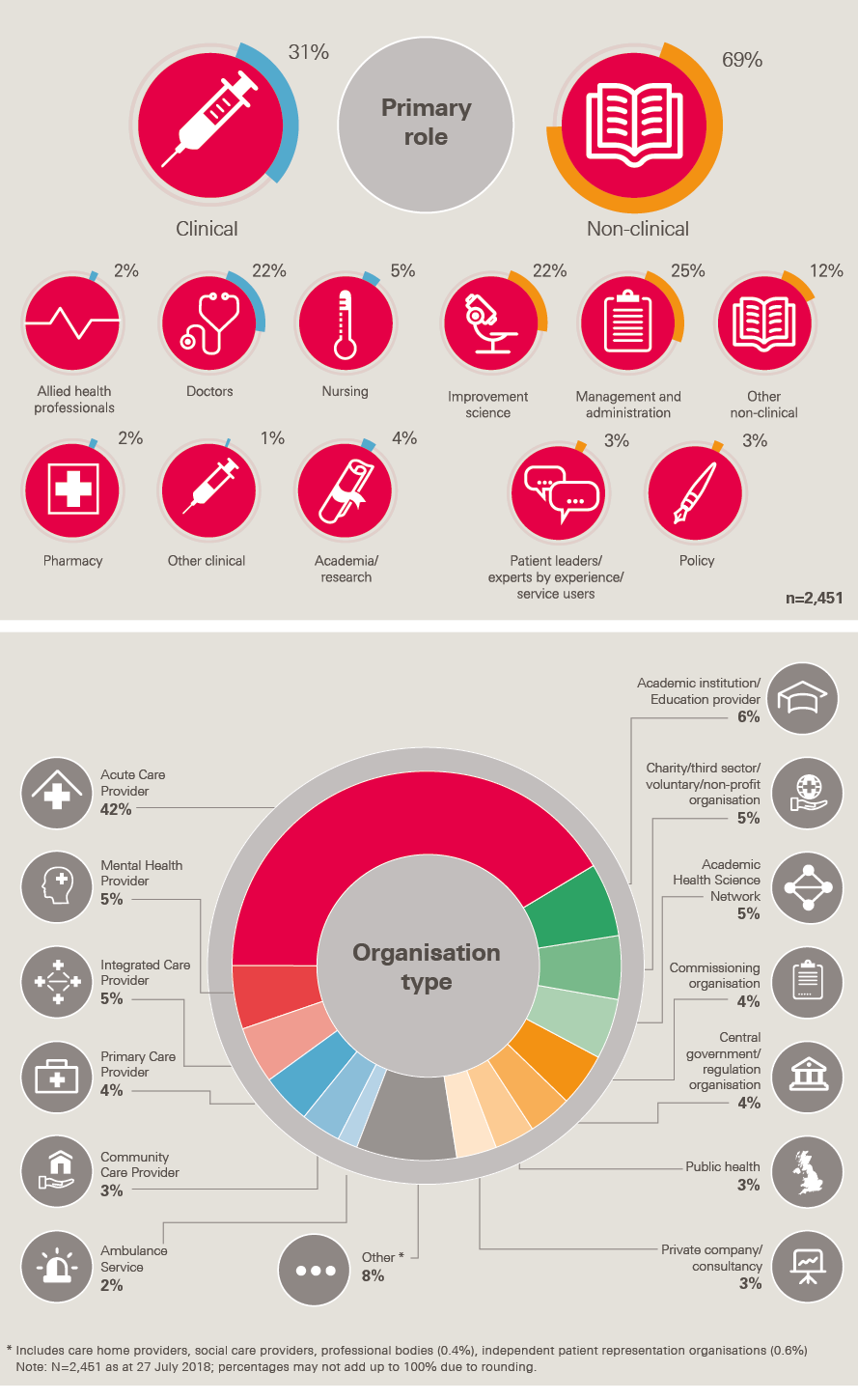
Figure 6: Demographic breakdown of members
Building a sustainable infrastructure for Q
The growth of Q over the last two years has not just been about attracting members. There has also been substantial work to establish an organisational infrastructure for Q, both centrally and regionally.
The central Q team at the Health Foundation has overseen the expansion of Q from a concept in development to a large community interacting with a range of activities and an evolving online space. The evaluation concludes that this scaling has been well managed, while highlighting the challenges of keeping a focus on reflective practice and devolved decision-making as the initiative evolves from co-design to large-scale delivery.
The evaluation examined the complexities of constructing coherent leadership arrangements for a community of thousands. The governance for Q needs to reflect the direct accountability Q has to its funders and the more diffused but real accountability to other partners and members on whose time and energy Q relies. In addition to developing the central oversight arrangements for Q, partners in three areas have been supported to pilot an innovative approach to community governance, based on Elinor Ostrom’s ‘commons’ concept.
Collaborative design with members has been core to the values and approach of Q to date, and will continue to be so, although the ways in which members are involved need to evolve as the community grows to include more use of online spaces, surveys and workshops on specific topics.

Connecting and learning at scale
Moving towards better-connected health and care improvement
The ability to make new connections is considered an important benefit of Q for many members. As well as people spontaneously finding new connections through the directory, or chance encounters, Q curates opportunities for members to connect face-to-face and online through national and local events and activities, Randomised Coffee Trials (RCTs) and Special Interest Groups (SIGs). These networking activities are underpinned by the Q website and communications activity, including the Q-municate monthly newsletter that includes profiles, blogs and member-generated content.
‘I started in QI before mental health had really grasped the concepts[,] and so learned by taking ideas from industry and elsewhere in health care and adapting them to work in my own area. This happened by necessity rather than design[,] but in Q this has really been at the heart of how it works and is in my view crucial to deliver accelerated learning for us all. At a local event, I [remember…] seeing an orthopaedic surgeon sitting next to a care home manager talking about improving support for the frail elderly. Q is helping make this way of working the norm.’
Helen Smith, Medical Director, Devon Partnership NHS Trust
Box 1: Randomised Coffee Trials (RCTs)
Around 200 Q members are currently signed up to Randomised Coffee Trials, which involves people being randomly matched each month with another Q member who has chosen to participate. They self-organise a 30-minute call or catch-up to discuss their work. 133 responses to a survey following each RCT reported the call had helped them generate new ideas, with 115 saying it led to collaboration with another colleague.
“The 30-minute call I had with a nurse from Morecambe was one of the most inspiring conversations I’ve had throughout my career – really inspiring stuff.” Hesham Abdalla
Figure 7 illustrates the scale at which Q has the potential to enable a more joined-up approach to improving health and care in the UK. In this analysis, collected through RAND Europe member surveys, members are represented by a circle, and a connection that at least one of the members reported as beneficial is represented by a line.
Figure 7: Q Community social network analysis (SNA) over time
7a: Connections at the start of the design phase
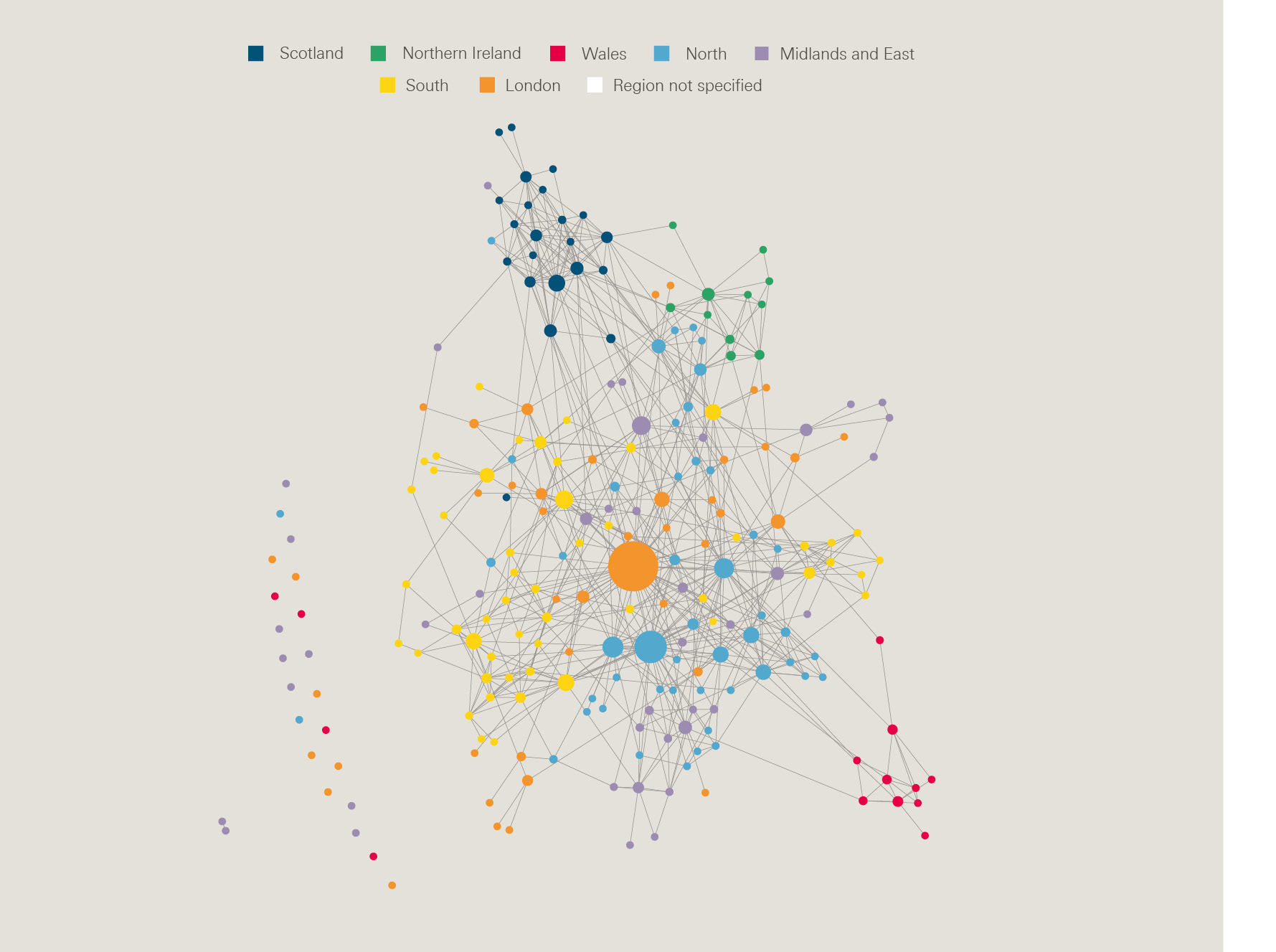
7b: Connections at the end of the design phase
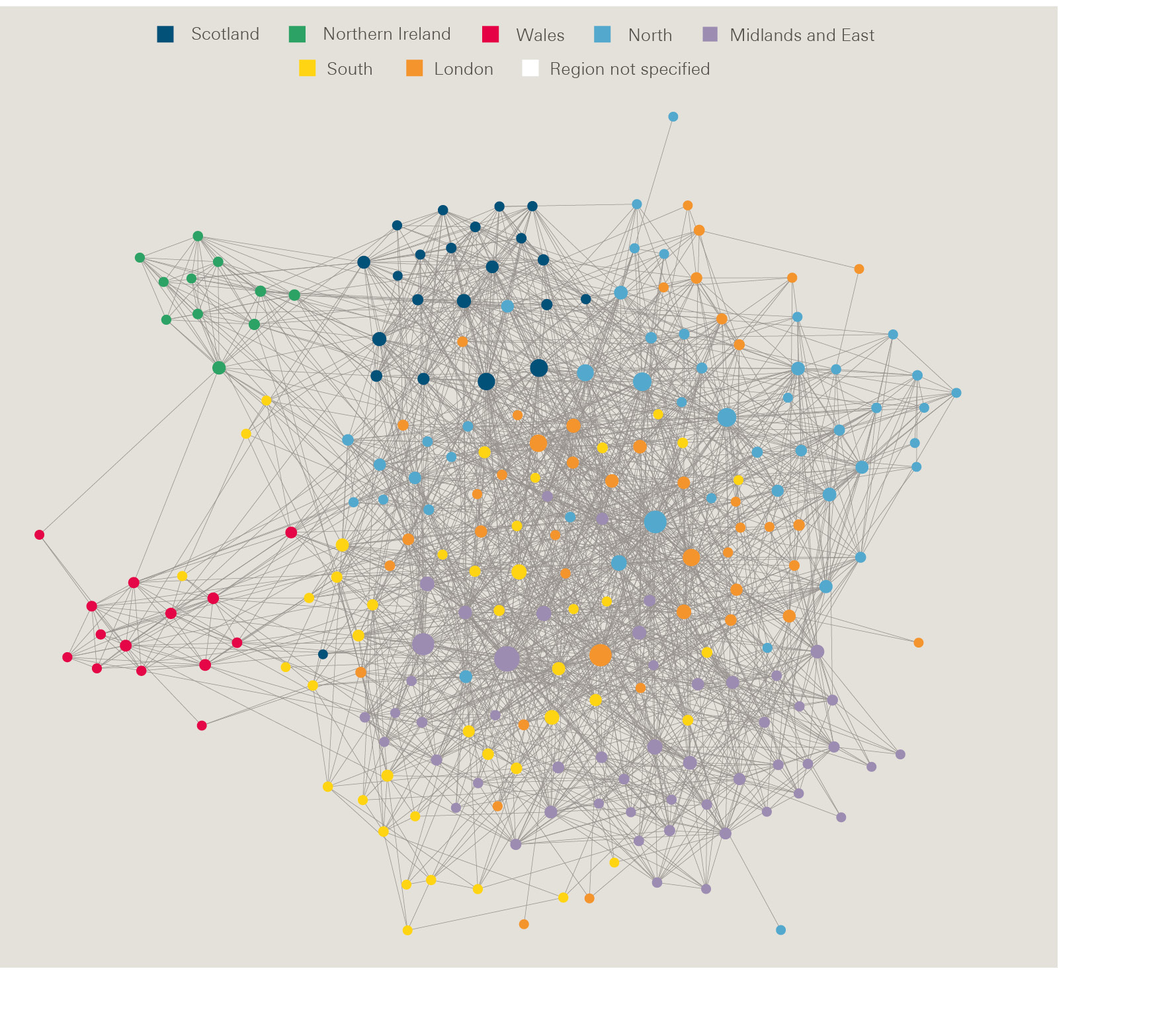
7c: Connections as of January 2018

Why does being better connected matter?
Research suggests that people who have strong social networks with others from beyond their organisational setting are more likely to have a successful track record of innovation and are more likely to experience follow-up approaches that allow them to access opportunities that are advantageous to them.
Members credit the connections they make as a result of Q with equipping them with new insights and skills, improving personal resilience and providing a fresh perspective, that enables them to better navigate different levels of the health and care system. These new connections are often described with a warmth and enthusiasm that suggests the deep value the links offer, with relationships described as ‘game-changing’ for those involved. The evaluation reflects on the potential for Q as a ‘home for improvers’ that supports members to become ‘more resilient, more mature and braver practitioners in a way that is likely to translate to tangible benefits for their organisations.’
Box 2: Case examples to illustrate the benefits connections made through Q bring
Disseminating Duty of Candour
A Q member who works for the General Medical Council described how Q has supported the development and dissemination of a duty of candour teaching programme for doctors. Through Q, the member became aware of an existing network and connected with others in the field. Together, they identified inconsistent training across hospitals. This network collaborated to develop a training programme to empower doctors to apply their knowledge of duty of candour in their practice. Over 200 members of staff have been trained and 95% of doctors have reported that they would use the resources in their work.
Life-changing professional relationships
Two members of the founding cohort described developing a relationship through Q that they report as being the most important professional relationship they have, helping them to work more effectively in their organisations and influencing how they work on a day-to-day basis. Having an external viewpoint provides them with fresh perspective on their own work. They also reflect on learning from different parts of the country which allows reflection on what works well and what could be different. This improves their understanding of system dynamics and encourages system-wide thinking.
Process mapping training
A Q member connected with another, more experienced, Q member who offered their expertise to facilitate a process mapping training event that explored how to improve an existing diabetes management programme. The connector felt that the input from this more experienced member improved the quality of the session and helped her to implement improvement techniques in their diabetes management programme. The collaboration also helped the facilitator to learn more about diabetes management and to make connections with GPs in the region.
The same Q member referred to a connection made with a member in Scotland, which led to a joint piece of work where they captured the global Twitter activity relating to antimicrobial resistance during World Antibiotic Awareness week. Although they had not met, they felt that virtual spaces like Twitter provided opportunities for members to connect, learn and share insights.
As illustrated in Box 2, members regularly share stories of being able to borrow ideas and inspiration from others, enabling them to shortcut or improve work that they are doing locally. This helps avoid wasted effort that comes from people solving problems that others have already addressed satisfactorily elsewhere – the ‘wheel reinvention’ identified as limiting the impact of improvement efforts. The Q team believes that if happening at scale, the ability to source advice from others doing similar work could represent a significant practical and resource-saving benefit to organisations, and play a role in speeding the effective adoption of new practices.
The evaluation notes that members interviewed identify that they would not have made the links they have without the existence of Q. The Q team hypothesizes that there are ways in which Q is nurturing connections that may offer greater prospect of enabling diverse, useful and lasting benefits to members than other mechanisms available. The attention that Q (and particularly the Q Lab) pays to cultivating an engaging environment in which diverse perspectives are valued and hierarchy is kept in the background, appears to enable connections that feel more personal and open. Q provides an inclusive shared mission and permission to reach out, together with multiple opportunities to connect with people over time, designed to foster genuinely useful connections that mature over time, which may not happen through individual events or conferences. Q does this on a larger scale and between more diverse groups than perhaps is feasible through more time-intensive training programmes.
‘I find it very hard to talk to people, and the idea of ‘making connections’ fills me with creeping dread. Despite this, through Q I’ve been able to talk about ideas with people who are doing interesting work locally. Q has given me some tools for creative problem solving and skills in presenting ideas to different audiences.’
Dan Beale-Cocks, Expert by Lived Experience, West of England
‘It was that relationship building, and [so that] actually I feel quite comfortable now contacting him. I think it’s something about […] feeling confident […] they’ll reciprocate and understand where you’re both coming from.’
Quote from RAND evaluation of Q
The evaluation evidences the impact that the connections formed through Q is having for individuals, although it is too early to judge the potential benefit for their organisations or more generally for improvement in the UK. As the community grows, a key priority will be ensuring that it is easy for Q members to find individuals or existing networks of people with similar interests and to ensure the opportunities for close personal connections aren’t lost.
Many of the benefits of connections made through Q are likely to be ‘below the radar’ of what can be detected centrally. Benefits may be relatively immediate or the outcome of these connections may take time to realise if opportunity for partnership comes months later. The Q team encourages Q members to see themselves as people who connect others in their organisation with knowledge and people who can help them – in these instances benefit may be several steps removed though nonetheless valuable. The diffuse nature of Q makes demonstrating the full value of the initiative difficult. However, the combination of large numbers joining Q and early evidence of benefits accruing to individual members suggests that in time Q can make a meaningful contribution to enhancing a culture of learning and improvement in the health and care sector.
‘I’ve had one or two people that I still work closely with […] that I don’t think I would have come into contact with without Q. [It] structure[s] contacts in a way that you potentially meet someone that you wouldn’t normally meet[,] but you do have common ground […] it certainly has facilitated, I think much better chances of finding someone you can actually take work forward [with.]’
Quote from RAND evaluation of Q
Box 3: Connecting on Twitter
While Q members overall often express a preference for connecting face to face, the Q Twitter account illustrates the potential for online engagement to mobilise knowledge and enable connections across a geographically dispersed community. The Q Twitter account has grown to around 9,000 followers – and a high level of engagement – in 18 months.
Twitter chats have emerged as a promising way to engage large numbers in discussion on a particular topic. Members participate by responding to questions or comments posted by the chat host and other Tweeters who have joined the session. Exchanges that happen on Twitter can be followed by using a designated hashtag during the hour chosen for the chat. Q has also hosted Twitter chats on artificial intelligence and scaling innovation.

‘Initially, I was a bit hesitant about joining the Q community but I’ve been encouraged by the spirit of the inclusiveness. In Northern Ireland, we need outward connections […] to make sure we are correctly confident of what we are doing well and aware of areas we need to improve on. One of the big challenges for improvement is to broaden its appeal and relevance. In the next 10–15 years I’d love to see the most sober leaders, such as the finance directors, routinely asking “How can we use improvement methods to address this problem?”’
Dr Mark Vignesha Roberts MPH FRCP, Clinical Director, HSC Safety Forum, Public Health Agency, Northern Ireland
Figure 8: Activities and resources

Flexible opportunities for learning and development
Increasing capability in change management and process improvement is a central aim of Q. By offering flexible ongoing professional development and peer support to people with established experience, Q seeks to equip members both to better lead improvement work and more effectively develop the improvement capability of those around them.
As illustrated in Figure 8, Q members have access to a range of learning opportunities and resources.
‘[What was positive about the Q community event was the] high level of energy and enthusiasm, the sense of pride that colleagues have in their impact, the genuine level of trust and benevolence, the supporting links to information, the publications, the feeling that collectively we can be the difference that the NHS needs, and the sense of being special.’
Quote from RAND evaluation of Q
As well as opportunities organised by the central Q team, Q members organise their own activities. Q’s 18 partner organisations across the UK also delivered networking events to coincide with new members who joined in 2017 and they continue to run a range of activities that support members in their improvement work. Box 4 highlights a few examples of this.
Box 4: Examples of local activities across the UK
Q Community Book Clubs
A Q book group was set up virtually, coordinated by several members across Scotland and England. This included a Tweet chat about the article Does Quality Improvement Improve Quality.
Health Improvement Manchester, in partnership with AQuA, has coordinated a book club that operates through face-to-face events. The club collaboratively selects texts that are relevant to improvement and hosts discussions that encourage members to share learning and consider how it can be applied in practice. Topics chosen include the habits of an improver, system thinking, resilience and creativity.
Improvement coaching programme
Three improvement coach workshops were delivered by the West of England AHSN. Members explored their perspectives on coaching, measuring team effectiveness and the role of the coach. The sessions also provided an opportunity for members to meet other improvement coaches. Attendees reported that they valued the balance between theory and practical exercises.
Behavioural insights workshops
At workshops organised by the Health Innovation Network and UCL Partners AHSNs, members were introduced to the concept of behavioural insights and explored how it can help influence decision-making in the health and social care context.
Masterclasses on measurement, strategy and networking
North East and North Cumbria AHSN hosted four masterclasses between July 2017 and February 2018. These explored measurement, strategy, networking and toolkits for improvement, with highlights captured on video.
Q Lab sessions
A local event for members and others interested in the Lab topic was held in Northern Ireland. People from all five health and social care trusts, as well as senior leaders such as the Chief Nurse and Deputy Chief Medical Officer, came together for a full day workshop to explore opportunities to improve and scale peer support services in Northern Ireland. When asked how helpful the workshop was for generating new ideas and perspectives on peer support the mean score was 4 out of 5.
Healthcare Improvement Scotland also organised an event for Q members to connect and collaborate, including running a session to share learning from the Q Lab.
The newsletter, website and Twitter account regularly signpost to members opportunities delivered by others, helping to encourage better use of the wide range of development offers available, ensuring Q makes a valuable contribution to the improvement landscape of which it is part.
The flexible ‘pick and mix’ nature of the Q learning and development programme is designed in response to the founding cohort identifying a wide range of development needs and that a lack of time is the most likely barrier to participation.
Underpinned by work with NHS Horizons to understand relevant learning theory, Q has developed a distinct approach to supporting development. Seeking to complement rather than duplicate the more structured training offers available elsewhere, Q specialises in providing opportunities that leverage peer learning and opportunities for people to make sense of expert content together. This recognises that often in improvement, evidence and best practice is only the start and people need to be able to explore how to adapt interventions to meet local circumstances if implementation is to be successful.
‘Learning is best understood as systemic and interwoven with the daily process of making change [or] learning comes through doing and, in particular, through doing with others in pursuit of shared aims.’
Given many Q activities started relatively recently, the longer-term benefits are yet to be evaluated. However, members rate Q activities highly and have reported that they have made a difference in their practice. Moving forward, the project team will continue to respond to member feedback and will seek to understand which activities provide the strongest benefit for members. There is work underway within Q and Q Lab to support deeper learning by developing a more structured learning and development framework to make it easier for people to understand which offers are most likely to be useful to them.
‘I find the [IHI subscription] very useful and use the resources a lot. I am progressing through the modules but finding time is quite difficult as work is so busy[.] I have used the learning to assist me in developing a measurement for improvement course which I run in-house.’

Collaborative change
Translating collective energy and insight into practical change
While there is broad enthusiasm for the potential of Q, there is also healthy challenge about what more Q can do to support change for service users and the health system. Given the pressures in the health and care sector, there is rightly significant focus for individuals on ensuring that the time invested in Q delivers real benefit for them and the services they deliver. One of the challenges with an initiative like Q is that it can be hard to make a direct causal link from the activities and learning members undertake to benefits for patients. This may account for the criticism and disengagement of a small minority of members, especially in the early days of establishing Q.
Q is designed to support members to deliver the core work they are doing to meet priorities agreed with their organisations. Q aims to extend the impact of other programmes and networks in the UK, rather than simply adding to the wealth of existing initiatives and requirements competing for the attention of those working in health and care. The examples of individual and small group connections and professional development described in the earlier sections of this report are supporting practical change as part of the day-to-day work of local organisations, and helping people identify and make links between existing initiatives.
Q is also increasingly creating space to initiate collaboration and change on a larger scale. As described in Box 5, Q supports a growing number of Special Interest Groups initiated by members.
Box 5: Member-led Special Interest Groups within Q
More than 40 Special Interest Groups (SIGs) have been set up online by members within Q, many with an aspiration to enable joined-up learning and collaboration between people working on a similar topic across the UK.
Topics covered by the groups include human factors, process visualisation in the NHS and primary care. While most of these groups are at an early stage of development, some have already built some significant momentum. For example, the Lean healthcare SIG has organised video conference calls to share case studies of successful implementations; the Closing the gap SIG held a video conferencing call with the Jönköping Academy; the Co-production SIG hosted a Twitter chat involving over 250 participants to gather feedback on new draft NIHR guidance; and the Radiotherapy quality SIG held a conference with 70 people.
Over time, Q aims to provide development and infrastructure for groups to enable them to accelerate and amplify their impact. Topic-focused networks may increasingly look to Q as a logical home, potentially avoiding the need for them to create their own online infrastructures from scratch. While significant design work will be needed, the aspiration is that the Q infrastructure evolves to offer spaces for focused activity combined with mechanisms for learning, and for people to flow easily between these spaces.
The 18 partners for Q are helping to embed Q within their regional infrastructure and aligning it with local priorities for improvement. Boxes 7 and 8 illustrate progress and insights from Q in Scotland and Wales.
‘We are trying […] to maximise the power of improvement by helping local Qs to find out who else is an improver in their organisation, their local STP and at regional level. Already we are seeing […] several organisations really start to build their own Q communities. In some parts of the West of England AHSN footprint we are beginning to see Q thinking emerging at STP level too, as local Qs work together to deliver QI training as part of the STP strategy.’
West of England Q Commons Stewardship Group
Q will be seeking to develop a fuller offer for people leading organisation and system change over the coming year, which is also expected to lead to increased use of Q to support strategic change.

Box 6: Q within provider organisations
Some organisations now have a significant number of Q members and are considering how best to support and ensure good use of Q members’ expertise and connections. The project team is aware of eight organisations that have established local Q groups – helping to ensure insights and skills gathered by Q members are shared with other staff and inform local work. For example, Newcastle Upon Tyne Hospitals NHS Foundation Trust’s quality strategy describes how the trust’s 23 Q members have come together to form a sustainable improvement collaborative within the organisation and how the organisation plans to encourage more to join, as well as looking to replicate elements of the Q model within their organisation.
As part of the evaluation RAND Europe examined Q member experience in Scotland. It found that Scotland’s improvement approach includes both ‘top-down’ and ‘bottom-up’ elements, with long-term investment and a culture of learning over time. This aligns with Q’s ambition for a more joined up and consistent yet flexible support structure for improvement across the UK. Q was identified as helping to connect ‘tribes’ that have developed within Scotland associated with particular programmes or approaches to improvement. A priority for Q in Scotland is to add further value to the well-established programmes in place, and for members to be clear about Q’s position within the Scottish context.
There is policy commitment in Scotland to using improvement methods across public services, with exciting work underway. Individuals interviewed by RAND highlighted the importance of tackling the ‘big ticket’ challenges of inequality and redesigning pathways to maintain the momentum behind improvement. As the reach and ambition of improvement activities extends, Q may have a helpful role to play in creating cross-boundary mechanisms for sharing and collaborating. There is also likely to be useful learning across different parts of the UK, with all countries seeking to achieve significant system change.
Box 8: The early influence of Q in Wales
In Wales, Q is enabling learning around how to embed improvement within organisations. Q members have supported each other by sharing examples of how QI teams are ‘contracted’ within their health boards and Q members are playing an instrumental role in helping to design and establish innovation hubs. Prompted by Q Exchange and Q Lab, links are being made between Q and programmes on repeat prescribing and peer support.
Methods learned through Q are being used at national and local events. This includes for example ‘speed consulting’ that supports peers to give each other advice on a problem they are grappling with. NHS Wales has also used a method learned through Q for developing different levels of maturity in an aspect of performance that supports peer sharing and ownership.
Over the coming years there will be increasing focus on ensuring national, regional and local initiatives can look to Q to enhance their work. This will help Q secure longevity and impact by being strategically connected to managerial and clinical priorities in the health and care sector. Box 9 describes what is currently available and provisional plans looking ahead.

Box 9: How Q supports national, regional and local initiatives
As part of the co-design phase of Q, members identified dozens of different initiatives underway to improve health and care, from work led by professional associations, clinical networks and charities to national and regional change programmes. Those delivering these initiatives can look to Q to:
- Find people with ideas and expertise that can help when developing or implementing change programmes.
- Provide time-efficient development and networking for those within central teams who meet the criteria to join Q.
- Raise the profile of their work, enabling initiatives to reach new members and make connections with any other similar activity underway elsewhere in the UK.
- Offer ways for Q members and others to collaborate online, for example through Special Interest Groups.
- Provide insights and methods that can be helpful when designing or delivering initiatives that involve many people.
Between now and mid-2019, as part of the development of a long-term operating model for Q, options for providing an enhanced package of support for existing initiatives will be developed. This could include all or some of the following elements as resources allow:
- Q Lab expertise and infrastructure to enable progress on identified complex issues.
- Opportunities to source insight from Q members on key issues in health and care that will be helpful to those delivering change.
- An infrastructure to galvanise attention and channel resource through Q Exchange: future rounds will test the potential for other organisations to contribute to the funding pot.
- An enhanced offer for groups that want to establish an infrastructure for networking and development linked to Q.
- Opportunities to use the network infrastructure of Q to support wider uptake of ideas and interventions.
In addition to supporting existing work, the Q team has centrally initiated two significant opportunities for members to work together on shared challenges: the Q Lab and Q Exchange.
Q Lab: making progress on complex challenges
The Q Lab provides a participatory and creative platform to bring together organisations and individuals from Q and beyond to make progress on a specific health and care challenge faced by many.
The Lab was conceived as part of the design phase for Q, recognising that it is often hard for those grappling with complex challenges in health care to access what’s already known and take the time to explore what offers greatest potential for sustainable change. The Lab has its own dedicated team, and there is the potential to develop a small network of 3–5 labs across the UK if the model lives up to the early promise of the pilot project on peer support (see Box 10).
Box 10: The first Q Lab project
The first Q Lab project looked at how to make peer support available to all those who need and want it. Over 200 people participated on a voluntary basis, contributing through workshops and an online space over 12 months.
Throughout the year-long process, the Lab pooled existing evidence and worked with participants to build a rounded understanding of the issue and identify opportunities and ideas for change. New insights were generated through a large-scale survey on how people make decisions about peer support and a grant has been awarded to support the development of a new evidence hub – an idea developed in collaboration with the charities National Voices, Mind and Positively UK.
The Lab’s learning is also being used by Q members who have submitted ideas to Q Exchange proposing practical ways to improve peer support. Further information about what has been achieved is available in a series of essays online. These essays tell the story of the Lab’s first year, describing the Lab approach and lessons learned. They also draw out the tensions and issues within peer support that often are not visible or are left unsaid, and make recommendations for taking this work forward.
The evaluation for the Lab found that irrespective of the participants’ expertise in the topic, most interviewees described how they gained a better understanding of the complexity of the peer support landscape, the multiple and diverse ways to deliver and commission peer support, and the challenges in accessing it.
‘I learnt a great deal and it really encouraged me to think from different perspectives about peer support.’
Quote from RAND evaluation of Q Lab
The evaluation concluded
‘The Q Lab […] makes a distinctive offer to the UK improvement landscape. It brings […] a multi-perspective and sustained exploration of the problem, creative stakeholder engagement within an effective and psychologically safe platform, and – in The Health Foundation – the branding of a trusted, independent and well-networked host. Its topic-specific and time-bounded nature creates focus and energy. Although each of these can be found elsewhere, their combination is powerful.’
Q Exchange: mobilising the community to support and select projects
Q Exchange (Figure 9) is an innovative pilot participatory funding programme for Q members that draws upon the collective intelligence of the Q community to identify projects that offer the greatest potential to benefit patients and the work that others are doing in the community.
The first stage involves members submitting ideas online, with others commenting to make connections with existing work and help bidders improve their proposals. The pilot saw over 180 ideas submitted and 1,500 comments shared. The final stage involves Q members selecting 15 winners from 25 shortlisted projects at an event. The significant engagement in the pilot suggests there is considerable appetite for more collaborative and iterative approaches to supporting improvement ideas.
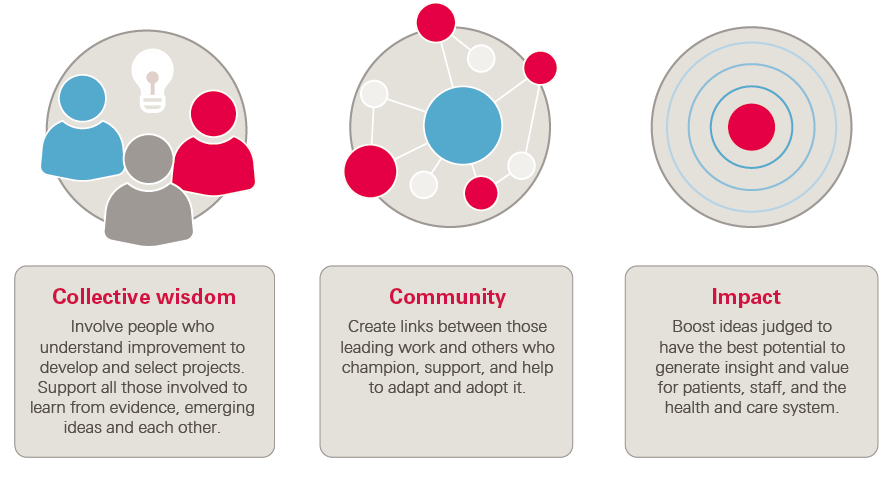
Figure 9: Q Exchange aims
It is hoped that through the process, the projects that are selected for funding with the help of the Q community will gather around them a set of supporters and potential future adopters, improving the prospect that investment in the initial idea will translate into successful and widespread uptake.
‘Q Exchange is definitely widening participation in QI, Q style, which is so exciting. And nurturing confidence, with those less confident about submitting bids encouraged to do so by their Q colleagues’.
Anna van der Gaag, Chair/Visiting Professor, University of Surrey

Conclusion: Where is Q now? Where next?
The value and experience of Q for members
Three years in, and with over 2,500 members and with a Twitter community approaching 10,000, Q has maintained its initial momentum, signalling the broad appeal of both what’s provided for members and the over-arching mission of a more joined-up approach to improvement across the UK.
A subset of members report that they are less actively engaged than they would like to be, suggesting they may be struggling to find the right ‘way in’ to Q or are yet to find opportunities that they are confident will help them achieve their priority objectives. A priority for those leading Q both centrally and locally will be to make it easier for members to navigate what’s available, with improved induction and clearer signposting. The Q website will see significant development over the year ahead, offering time efficient access to knowledge and people.
Q is voluntary, with no minimum level of engagement expected. Network theory suggests it is normal to have a relatively small proportion of all members who are proactively engaged at any particular point and there is more to learn about what will be reasonable to expect within Q. In order to increase engagement, the Q team recognises there is more to be done to help employers to understand the benefit that participation will bring.
45% of members in the first phase of recruitment reported having protected time to participate in Q activities, with some taking annual leave to attend events. This illustrates the restrictions on funding and time available for many groups of staff to participate in development activities, even when activities are free to attend. Operating in this context, Q needs to demonstrate that it offers practical and potentially resource-saving ways for organisations to access the expertise and ideas needed to deliver high quality, sustainable care.
Looking forward
Q has been conceived from the start as a long-term initiative, and over the coming months the central team and Q’s partners will lead a process to establish a funding and delivery model for Q fit for the long term. The aim is to deliver on the promise that Q becomes a stable platform that enables sustained momentum for improvement, despite the structural turbulence that often characterises the health and care sector. As described in Box 9, this will also explore ways Q can more explicitly and fully support work on priority issues.
Change at an increasingly ambitious scale
The major challenges facing the health and care sector in the decades ahead will require change at multiple levels. Arguably, the NHS is reasonably well structured to support change within individual institutions, such as acute hospitals. Far fewer mechanisms exist for the generation and exchange of knowledge between people, teams, organisations and sectors. This is particularly true when it comes to sharing knowledge about how best to design and iteratively improve processes of care. Q is designed to be an infrastructure that is flexible enough to support and help connect people doing the diverse range of work needed over the years ahead.
The outputs from Q Labs and Q Exchange are adding to a growing bank of tangible examples of Q enabling collaborative change. As Q attracts more people both at the front line and leading change at an organisational and system level, the scale and strategic significance of Q’s impact is likely to expand.
The evaluation includes examples that suggest Q adds value by providing a space where lessons are shared between people leading improvement to services – this is where ‘the rubber hits the road’ in terms of making a difference for those who use the health and care system. The learning from the evaluation and the insights from the Q team suggest that Q also has the potential to mature into a space that supports those engaged in more strategic work that seeks to transform care models and shift the focus to prevention.
Conclusion: ongoing learning and improvement
Ultimately, and as reflected in Q’s updated theory of change, the aim is that the improvement workforce in the UK becomes broader based and better supported, and that people leading improvement can operate more effectively across boundaries to understand what’s needed and speed uptake of what’s useful. Q seeks to bring together a critical mass of activity in individual local systems and on key topics, and in this way accelerate sustainable approaches to improvement all across the UK.
The potential of Q is only just starting to be realised. Learning, designing and delivering collaboratively with members and partners has been core to what has been achieved so far. This report, and RAND’s evaluation, reflects the generosity and passion that Q’s members and partners have brought to help establish and continually refine Q.

Appendix: Recruitment
The recruitment process
Reaching ‘first base’ by attracting and recruiting people to the Q community has been a major undertaking. The 48 organisations that nominated the founding cohort of Q members have continued to help promote Q and this evaluation pays credit to the collaboration between the central Q team and 18 regional partners who oversaw a near 10-fold increase in members between November 2016 and April 2018.
Some applicants found the process overly onerous, though others felt that the time spent considering why people want to join Q and what they would bring was important to build commitment. With each round of recruitment, incremental improvements were made in response to the evaluation and member feedback, with the current process reflecting a more substantial redesign and streamlining process.
‘I think that being part of a selection process means that you value membership more highly when successful. It requires more active rather than passive engagement with the opportunity.’
Quote from RAND evaluation of Q
In general, the recruitment process was seen as well managed and fair. Encouragingly, most unsuccessful applicants felt that they understood why they had been unsuccessful and would consider applying again.
Debate about recruitment criteria
Recruiting large numbers of people is not just an operational challenge. From the start, the fact that people need to apply to join Q has divided opinion. Following substantial debate and consultation in the design phase, applicants need to demonstrate experience of playing an influential role in efforts to improve health or care that spans more than one team and to demonstrate some reflection on approaches to change. The criteria are designed to include those supporting improvement from a range of professional or lay perspectives. Those operating at a local, regional or national level to create the conditions to enable front-line improvement work are also able to apply. Q is not just for those who have been part of improvement projects at the point of care.
While some feel that the participatory ethos of improvement is at odds with a selection process, there is a strong case, broadly accepted by many, that having an initiative that recognises those with established expertise is valuable. In this way, Q seeks to complement rather than compete with open networks that exist locally, and reflect the evidence that leading improvement successfully requires relatively advanced skills and knowledge. Given that peer learning is core to the appeal of Q, having a selection process appears important to establish a common baseline of understanding and shared language.
There has been particular interest and debate regarding the involvement of service users within Q. As part of the design phase of Q, workshops were held with people who identified as patients or patient advocates to explore the recruitment criteria. There was a targeted opportunity for patients to apply in 2016 and the peer support focus of the first Q Lab project helped to bring Q to the attention of people with long-term health needs. The Q team has developed a policy for working with patients in the community, and was selected to share the work Q has done on patient involvement as part of the International Forum on Quality and Safety in Healthcare in 2017.
As the Q community grows and it is possible to show how a growing number of people from different backgrounds, including patients, have been able to demonstrate they meet the criteria, there appears to be broader acceptance of the chosen selection process. The data being generated through Q can support further work about both how to attract more people to join Q from diverse backgrounds, and how to target development to ensure people have the opportunity to develop the skills and experience to meet the criteria. It is encouraging that Q Exchange has stimulated a number of project proposals focused on building the improvement skills of people with lived experience.
A priority for the next stage will be to more actively encourage and demonstrate how Q members are reaching out to support and develop others within their organisations, demonstrating how a community of people with established expertise can help catalyse widespread engagement in improvement.
Endnotes
- Garrod B, Exley J, Harte E, Minani C, Newbould J, Saunders and Ling T. An evaluation of the first phase of Q. RAND Europe; Cambridge; 2016. Available from: www.rand.org/content/dam/rand/pubs/research_reports/RR1500/RR1517/RAND_RR1517.pdf
- May T. PM speech on the NHS. London; Prime Minister’s Office, 10 Downing Street; 2018. Available from: www.gov.uk/government/speeches/pm-speech-on-the-nhs-18-june-2018.
- Keown O P, Parston G, Patel H, Rennie F, Saoud F, et al. Lessons From Eight Countries On Diffusing Innovation In Health Care, Health Affairs. 2014;33(9):1516. Available from: www.healthaffairs.org/doi/pdf/10.1377/hlthaff.2014.0382
- National Advisory Group on the Safety of Patients in England. A promise to learn, a commitment to act: Improving the safety of patients in England. London: The Stationery Office; 2013. Available from: www.gov.uk/government/publications/berwick-review-into-patient-safety
- For an overview of learning from the design phase of Q see O’Malley H and Pereira P. Building Q. London: Health Foundation; 2016. Available from: www.health.org.uk/publication/building-q
- Project team collected quote: https://q.health.org.uk/news-story/improvement-journey-andrea-gibbons/
- Ling T, Stewart K, Garrod B, Hocking L, Newbould J and Gendronneau C. Evaluation of the Second Phase of the Q Initiative 2016–2020: Interim Report. Cambridge: RAND Europe; 2018. Available from: https://www.rand.org/pubs/research_reports/RR2324.html
- Liberati E, Sim MPY, Pollard J and Ling T. Independent Evaluation of the Q Improvement Lab. Cambridge: RAND Europe; 2018. Available from: https://www.rand.org/randeurope/research/projects/q-improvement-lab-evaluation.html
- Greenhalgh T. How to Implement Evidence-Based Healthcare. Wiley-Blackwell; 2017.
- Q project team collected quote: qualitative feedback provided directly.
- For a description of special interest groups, see Box 5 on page 23.
- Q project team collected quote: https://q.health.org.uk/news-story/improvement-journey-esther-hall/
- Q project team collected quote: https://q.health.org.uk/news-story/member-story-ruth-jordan/
- Neville S. Health consultancy work under pressure as NHS seeks savings. 2018. Available from: www.ft.com/consultancy-health
- Q. Community Directory. 2018. Available from: https://q.health.org.uk/community/directory/
- Women 77% and men 23%. NHS Employers. Gender in the NHS infographic. 2018. Available from: www.nhsemployers.org/case-studies-and-resources/2018/05/gender-in-the-nhs-infographic
- Ostrom E, Dietz T, Dolšak N, Stern P C, Stonich S, Weber E U (eds). The drama of the Commons. Washington DC: National Academy Press; 2002.
- Q project team collected quote: qualitative feedback provided directly.
- Keen D. RCT data 08–05–18. Internal report. Unpublished; 2018.
- Rogers E M. Diffusion of Innovations. 5th ed. New York: Free Press; 2003.
- Arena M, Cross R, Sims J and Uhl-Bien M. How to Catalyze Innovation in Your Organization. MIT Sloan Management Review. 2017;58(4):38–48.
- Dixon-Woods M and Martin GP. Does quality improvement improve quality? Future Hospital Journal. 2016;3(3):191–194. doi: 10.7861/futurehosp.3-3-191.
- Q project team collected quote: https://www.health.org.uk/newsletter/power-q-hear-three-community-members?pubid=healthfoundation&description=july-2018&dm_i=4Y2%2C5RUKC%2CO2YM0A%2CMIQLD%2C1
- Q project team collected quote: https://www.health.org.uk/newsletter/power-q-hear-three-community-members?pubid=healthfoundation&description=july-2018&dm_i=4Y2%2C5RUKC%2CO2YM0A%2CMIQLD%2C1
- Stewart K, Hocking L, Newbould J, Garrod B, Gendronneau C and Ling T. Evaluation of the Second Stage of the Q Initiative 2016–2010: Interim Report [unpublished report]. Cambridge: RAND Europe; 2018.
- AHSN North East and North Cumbria. AHSN NENC Q Masterclasses [video]. 28 March 2018 [cited 2 August 2018]. Available from: https://youtu.be/EUP-8ZeIr2o
- Q Learning Theory – NHS Horizons for Q. Available from: https://public.huddle.com/a/rBdlean/index.html
- Albury D, Beresford T, Dew S, Horton T, Illingworth J and Langford K. Against the odds: Successfully scaling innovation in the NHS. 2018. Available from: www.innovationunit.org/projects/against-the-odds
- The Health Foundation. Summary of Q’s internal data. Internal report: unpublished; 2018.
- Q project team collected quote: qualitative feedback for evaluation of subscriptions.
- Q project team collected quote: provided by Anna Burhouse, Q member, on behalf of the West of England Q Commons Stewardship Group.
- Ling T and Hocking L. Q evaluation quarterly report: May 2018 [unpublished report]. Cambridge: RAND Europe; 2018.
- Q. Creative approaches to problem solving toolkit. 2018 [cited 27 July 2018]. Available from: https://s20056.pcdn.co/wp-content/uploads/2017/08/Q-community-CAPS-toolkit-2017.pdf
- Q project team collected quote: qualitative feedback provided directly.
- For a list of projects shortlisted for Q Exchange see: https://q.health.org.uk/get-involved/q-exchange/shortlisted-ideas/.
- The Health Foundation. Effective networks for improvement. London: The Health Foundation; 2014. Available from: www.health.org.uk/sites/health/files/EffectiveNetworksForImprovement.pdf
- Q’s Theory of change. Available at: https://q.health.org.uk/theory-of-change/
- Dixon-Woods M, McNichols S and Martin G. Overcoming challenges to improving quality. London: Health Foundation; 2012. Available from: www.health.org.uk/publication/overcoming-challenges-improving-quality
- Q. Frequently asked questions. 2018. Available from: https://q.health.org.uk/about/frequently-asked-questions/#criteria