Key points
- As the number of people with multiple health conditions grows, meeting their needs will be one of the biggest challenges facing the NHS. In 2006/07, one in 10 patients admitted to hospital as an emergency had 5+ conditions. In 2015/16, the figure was one in three.
- People with multiple conditions often have poorer quality of life, greater risk of premature death, and may need substantial NHS support. But the ability of the NHS to plan care that responds to these needs has been hampered by a lack of information about the conditions that people have and their existing patterns of care.
- To fill some of the gaps, we analysed data from 2014 to 2016 for 300,000 people in England. We considered 36 health conditions, including physical and mental health conditions, ongoing symptoms such as chronic pain, sensory impairment and substance misuse.
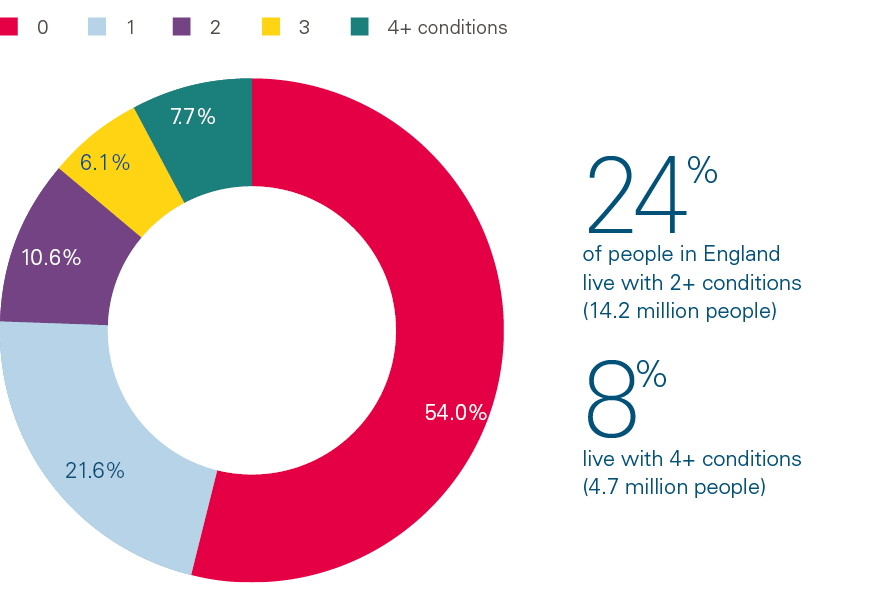
- We found that one in four adults had 2+ health conditions. This equates to approximately 14.2 million people in England with multiple conditions.
- People in disadvantaged areas are at greater risk of having multiple conditions, and are likely to have multiple conditions at younger ages. Around 28% of people in the most-deprived fifth of England have 4+ conditions, compared with 16% in the least-deprived fifth. In the least-deprived fifth of areas, people can expect to have 2+ conditions by the time they are 71 years old, but in the most-deprived fifth, people reach the same level of illness a decade earlier, at 61 years of age.
- Although having multiple conditions is often thought of as being related to old age, 30% of people with 4+ conditions are under 65 years of age, and this percentage is higher in disadvantaged areas. Improving care for people with multiple conditions requires action across the NHS and other sectors, not just services targeting elderly people.
- People with multiple conditions have multiple consultations and treatments. We found patients with 4+ conditions had an average of 8.9 outpatient visits across 2.8 different medical specialties. Over the study period, they visited their general practice 24.6 times (or once a month on average) and were prescribed 20.6 different medications. This compares with the 2.8 outpatient visits, 8.8 visits to the general practice, and 5.6 different medications for patients with one condition. However, people with multiple conditions did not seem to have significantly longer GP consultation times despite their more complex needs.
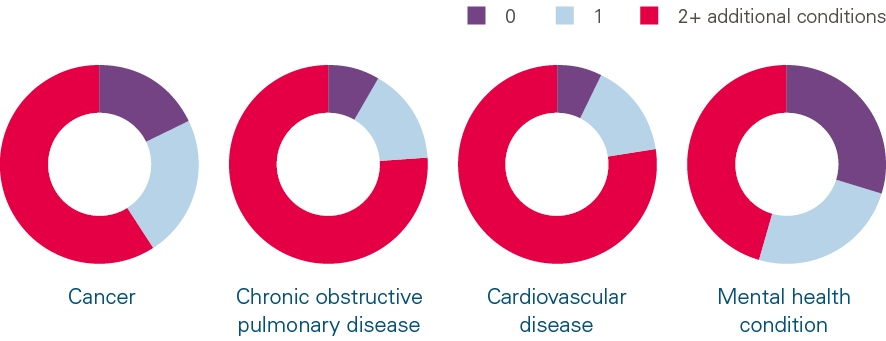
- Our analysis shows that 82% of people with cancer, 92% with cardiovascular disease, 92% with chronic obstructive pulmonary disease and 70% with a mental health condition have at least one additional condition. But clinical strategies to manage care often focus on single conditions.
- Care for those with 2+ conditions accounts for a large proportion of NHS costs, including over half of the costs of primary and secondary care, and three-quarters of the costs of primary care prescriptions. Over the next 5 years, the rising number of people with multiple conditions is projected to increase total hospital activity by 14% and costs by £4bn. Therefore, a sustainable NHS will need to improve both the quality and cost-effectiveness of care for people with multiple conditions.
- Given our findings, long-term planning for the NHS needs to have a clear focus on people with multiple conditions. We suggest six key steps to improve care for this group: supporting those with multiple conditions to live well; developing new models of NHS care for those with multiple conditions; resourcing the vital role of primary care; designing secondary care around those with multiple conditions; using data and sharing information to improve care for those with multiple conditions; and evaluating what works.
- To ensure that everyone has the best opportunity to live a healthy life, urgent cross-government action is needed to tackle the underlying causes of multiple conditions, along with investment in the public services that affect people’s health.
Introduction
The NHS faces a mismatch between demand and resources. This has led to year-round pressures on emergency departments and less visible, but very real, pressures on primary and social care. The extra £20.5bn promised by the government for the NHS in England, while substantial, is only what is required to maintain current levels of care. But demand and cost pressures are likely to increase over the next 5 years.
The increased demand is largely due to two factors: our ageing population and a rise in the number of people living with conditions such as diabetes, cardiovascular disease, and depression. Not only are more people living with health conditions, more people have multiple conditions. The number of people in England with 4+ conditions is predicted to double between 2015 and 2035. In many ways, this is good news: more people are surviving diseases like cancer, stroke and heart disease because of better treatment and therefore living longer. However, this means that people are living with these health conditions, as well as others that arise as they age. The effects of this change are evident across the health care system. For example, the biggest growth in emergency admissions has come from those with multiple conditions. In 2006/07, one in 10 patients admitted to hospital as an emergency had 5+ conditions. In 2015/16, the figure was one in three. Patients with multiple conditions stay longer in hospital and are more likely to be readmitted when finally discharged.
The effects of living with multiple health conditions can be profound. People with multiple conditions have poorer quality of life, difficulties with everyday activities, and greater risk of premature death.,,,, When people talk about the impact of their conditions on their daily lives, some report a loss of mobility, resulting in isolation. The demands of their conditions sometimes do not allow them to remain in work, leading to financial hardship and the loss of valued jobs and colleagues. This then exacerbates inequalities, with loss of income and worklessness contributing to further declines in health. There is a danger that, without action, worsening socioeconomic inequalities will further concentrate this trend among the most disadvantaged.
How has the health care system responded to the growing number of people with multiple conditions?
With the number of people with multiple conditions rising, the NHS has begun to recognise the importance of delivering care across traditional disease specialties and health and social care boundaries. Guidelines and care-quality indicators for the assessment and management of people with multiple conditions have been developed, and the need for research into better models of care for people with multiple conditions has been highlighted.,, Researchers and practitioners in many countries agree that health systems need new models to care for those with multiple conditions.
The responsibility for managing their conditions falls primarily on the individuals themselves. Some need to take multiple medications at certain times, or regularly monitor clinical indicators like blood sugar. Unsurprisingly, juggling the tasks needed to manage multiple conditions can feel like an overwhelming burden for some people. The Health Foundation has shown in its own research that people who are less able to effectively manage their health conditions require more care from the NHS., In planning the long-term future of the NHS, national programmes targeting specific conditions (such as cancer, cardiovascular disease or mental health) are important to improve care for patients with those conditions. But they need to be supplemented with a strategy that focuses action on multiple conditions, informed by better information about the needs of this growing group of people.
In this briefing, we describe what NHS care looks like for patients with multiple conditions. We also show what proportion of NHS resources is used to provide care for these patients. We argue that designing high-quality care for patients with multiple conditions should be an essential part of any NHS strategy – be it for primary, secondary, community, emergency, or integrated care. We emphasise that multiple conditions are a concern for all patients, not just elderly ones, particularly in deprived areas, and that having an additional condition can increase the complexity of a patient’s health needs and their need for support and treatment from the NHS.
The challenge of measuring multiple conditions
One challenge of researching multiple conditions is that there is no agreement on which, or how many, conditions should be considered. Logically, the longer the list of conditions of interest, the more people will be identified as having multiple conditions, leading to differing estimates of prevalence. We used a list of 36 conditions, selected because they lead to a significant need for treatment or have been linked to poorer quality of life, poorer functioning or greater risk of premature death (Box 1). The list includes long-term and recurring conditions (eg depression, diabetes) as well as risk factors (eg hypertension) and symptoms including chronic pain (which has been referred to as a painful condition,). The conditions are all recorded by GPs, and have been commonly used in recent studies in England.,
Box 1: List of 36 conditions used in this analysis
- Alcohol problems
- Other psychoactive substance misuse
- Anorexia or bulimia
- Asthma (currently treated)
- Atrial fibrillation
- Blindness and low vision
- Bronchiectasis
- Chronic kidney disease
- Chronic liver disease
- Chronic obstructive pulmonary disease (COPD)
- Constipation (currently treated)
- Coronary heart disease
- Dementia
- Depression, anxiety and other neurotic, stress-related and somatoform disorders
- Diabetes
- Diverticulosis
- Epilepsy
- Hearing loss
- Heart failure
- Hypertension
- Inflammatory bowel disease
- Irritable bowel syndrome
- Learning disability
- Migraine
- Multiple sclerosis
- New diagnosis of cancer within last 5 years
- Painful condition (on prescription-only pain medication)
- Parkinson’s disease
- Peripheral vascular disease
- Prostate disorders
- Psoriasis or eczema
- Rheumatoid arthritis, other inflammatory polyarthropathies and systematic connective tissue disorders
- Schizophrenia (and related non-organic psychosis) or bipolar disorder
- Stroke and transient ischaemic attack
- Thyroid disorders
- Viral hepatitis
Our analysis used a pseudonymised database of electronic health records, the Clinical Practice Research Datalink. We obtained approval for this study from an independent committee (ISAC protocol reference number 17_150RMn2). Individuals cannot be identified from these records and data confidentiality was maintained by our rigorous adherence to strict data-handling procedures in a secure data environment. More information on data security is available on the Health Foundation’s website.
We used a random sample of 300,000 patients registered with a GP, a sample large enough to carry out our study robustly, and which, from previous studies, we know is broadly representative of the population of England. For each patient in the dataset we counted the number of conditions that appeared in the primary care records on 1 April 2014, using published code lists. We then calculated the use of health services between then and 31 March 2016 (a 2-year period) and estimated the cost of these services for every patient in the sample.
Using this approach, we could estimate the total use and cost of their NHS care over a range of primary and secondary care services. This included hospital admissions, visits to emergency departments, outpatient appointments, primary care consultations and primary care prescriptions. Specialised commissioning, specialist mental health care and community care are not included in these records.
Our analysis uses a large linked dataset, with a comprehensive picture of conditions from primary care records, but there are limitations with our approach. In most cases, the dataset didn’t record the severity of the conditions, and we didn’t track how long the patient had the condition, or whether they developed additional conditions during the 2-year follow-up period. How long a patient has a condition might be important. For example, a person may have more interaction, and thus hospital and GP activity, with the NHS when they are first diagnosed than later in the course of their disease (eg for cancers).
How many people have multiple conditions?
Nearly one in four people in our sample had 2+ conditions (Figure 1), which corresponds to an estimated 14.2 million people in England., Around one in 12 people have 4+ conditions – an estimated 4.7 million people in England.
Figure 1: Percentage of people with 0, 1, 2, 3 and 4+ conditions
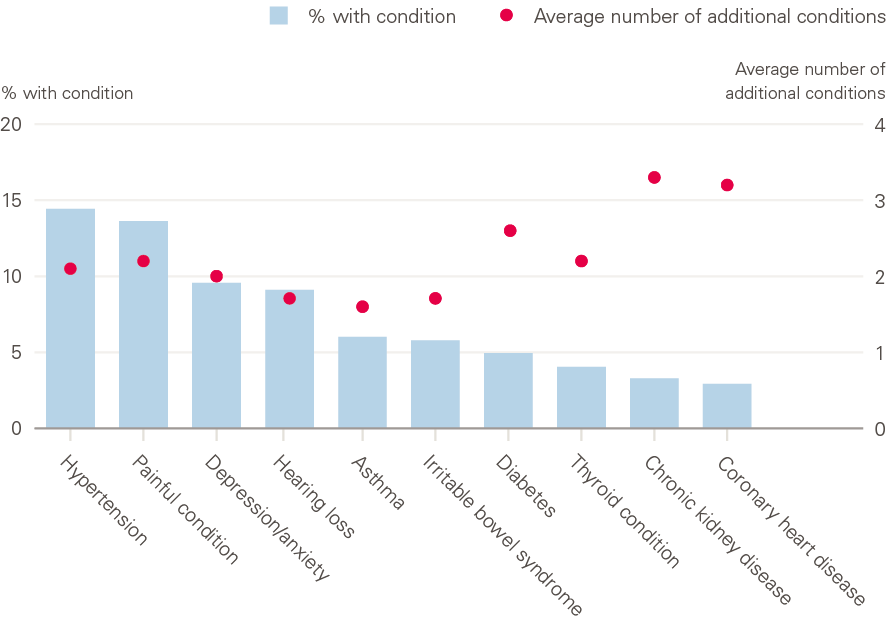
The most common conditions in our sample are shown in Figure 2. One in seven people had hypertension and one in eight had a painful condition. A person with hypertension had an average of 2.1 additional conditions and a person with depression or anxiety had 2.0 additional conditions. People with chronic kidney disease had 3.3 additional conditions.
There has been some interest in identifying clusters and combinations of multiple conditions that are associated with particularly poor outcomes for patients and increased demand on the health care system. Of the 36 conditions we included, some fall within the same body system – for example, coronary heart disease and hypertension. These might share underlying biological mechanisms and as a result there might be a common treatment approach. By contrast, conditions that are in different body systems, and treated by different specialists may be more complex to manage (eg depression and diabetes). An important limitation of our work is that we counted each condition as separate, even if it was related to another, and did not account for whether any might be concordant or discordant. Future work to describe the impact on people and on the NHS of having multiple discordant versus concordant conditions could help the NHS to plan services better.
Figure 2: Common conditions and average number of additional conditions
* This is an estimate is based on September 2018 figures of 59,297,331 patients registered at a GP practice in England. It is based on the estimated prevalence of 2+ conditions in each year of age but does not account for other characteristics that might be related to prevalence (eg gender, socioeconomic deprivation).
† People on 4+ prescription-only analgesics or 4 antiepileptics in the absence of an epilepsy diagnosis were defined as having a painful condition.
The importance of multiple conditions for priority conditions
The NHS has often focused resources and attention on single, important conditions such as cancer, cardiovascular and respiratory diseases, and mental health. This focus can achieve improvements in treatment and outcomes for patients, however failing to consider the impact of multiple conditions on patients with these conditions would be a mistake. Our analysis shows that 82% of people with cancer, 92% with cardiovascular disease, 92% with chronic obstructive pulmonary disease (COPD), and 70% with a mental health condition had at least one additional condition (Figure 3). The average number of additional conditions ranged from 1.8 for those with a mental health condition to 3.3 for those with COPD. In other words, for these patients, having multiple conditions is now the norm.
Hypertension and pain were the most common additional conditions in the four clinical conditions we looked at (Figure 4). For example, 40% of people with cancer also had hypertension and over 30% had a painful condition. This may reflect either causation (eg a cancer that causes pain) or the fact that these are common conditions in the population.
Figure 3. Average number of additional conditions for people with cancer, chronic obstructive pulmonary disease, cardiovascular disease, or a mental health condition
Although strategies to improve health care often have a single disease focus, future initiatives might need to consider the person’s additional conditions to reduce their treatment load and improve their outcomes. For example, people with heart disease are at higher risk of dying in the short and medium term if they have depressive symptoms, compared with those who do not. Appropriate treatment for depression might be as important as treatment strategies for heart disease risk factors (and might help patients to adhere to those strategies).
‡ These estimates are based on a total of 4,075 people with cancer, 12,971 people with cardiovascular disease (coronary heart disease, stroke, transient ischemic attack, peripheral vascular disease), 4,890 people with COPD, and 32,792 people with a mental health condition (including depression, anxiety, schizophrenia, anorexia, bulimia, alcohol or other substance misuse) in our sample.
The complex care of people with multiple conditions
The care of people with multiple conditions is often complex, is delivered by many parts of the NHS, and can demand much time and interaction with the health care system., In our analysis, we took a detailed look at care for those with multiple conditions to learn about the complexity of the care they receive and which parts of the NHS they have to navigate. As our analysis is based on information available from electronic health records in primary care and administrative data in secondary care, it summarises the number of visits they made to primary and secondary care, but does not include community health care and social care. Neither does it capture the experience from the patient’s perspective, and so may omit important elements such as the difficulty of arranging transport to attend appointments, the impact of care on their daily lives, and which elements of NHS care they find most valuable.,
Figure 4: Most common additional conditions for people with cancer, cardiovascular disease, chronic obstructive pulmonary disease or a mental health condition

Patients with multiple conditions make more visits to outpatient departments (Figure 5) than patients with a single condition. Over the 2 years of our study, those with 4+ conditions averaged 8.9 outpatient visits in 2.8 specialties. Traditionally, specialists in outpatient departments are not set up to provide joined-up treatment, though increasingly there are examples of specialties working together. If a patient is receiving treatment from multiple specialists, those specialists might be treating the patient according to condition-specific guidelines, rather than considering what other conditions the patient has and coordinating their advice and treatment. It is important to develop greater collaboration between specialists, as otherwise information from different specialists will only be brought together by the GP and the patient.
Figure 5: Outpatient and primary care interactions by number of conditions

Unsurprisingly, we found that the number of primary care consultations a patient has increased with each additional condition (Figure 5). Over the 2-year study period, those with 4+ conditions had an average of 28.9 consultations, compared with 10.0 consultations for those with a single condition. Most of the consultations (24.6/28.9) for patients with 4+ conditions were face-to-face GP consultations. The process of recording the patient’s symptoms, diagnosing, and identifying appropriate medications is likely to be more complex for those with multiple conditions, yet the average GP consultation time was not strongly related to the number of conditions. Patients with 4+ conditions received only an additional 14 seconds per consultation on average, compared with patients with a single condition.
Patients with 4+ conditions were prescribed an average of 20.6 different medications or other therapies by their GP over the study period. Taking more medications increases the risk of side effects and drug interactions. Taking multiple medications on strict schedules can be challenging, so patients may find it difficult to adhere to the treatment their doctor prescribes.
Over the 2-year study period, three times as many people with 4+ conditions (3/100) were admitted to hospital than people with a single condition (1/100). We might expect patients with more conditions to have more hospital admissions as an appropriate part of their care, and both routine and emergency admissions were more common for people with multiple conditions. However, we know that hospital admissions are often undesirable for patients, and there is some evidence that if GP care is managed by the same practitioner over a long period of time, patients have fewer emergency admissions. We also know that some patients with multiple conditions find it difficult to manage their own health away from the NHS, and that those who find it difficult to manage their own health have more emergency admissions. Further work is needed, but research suggests that emergency admissions are not inevitable for patients with multiple conditions, and could be avoided through improved continuity of care, or if patients were supported to improve their ability and confidence to manage their own health conditions.
Planning NHS care for people with multiple conditions
As life expectancy has increased in recent decades, so has the number of people with multiple conditions. The NHS must make realistic plans to provide appropriate care for this growing group. To illustrate the potential impact on the NHS, we calculated the average use and cost of primary and secondary care services according to the number of conditions a person has.
Hospital and primary care records don’t directly contain information on the cost of treatment. For secondary care (emergency department, outpatient and inpatient care), we used national tariff costs. Each occurrence of care was assigned to a health care resource group and the national tariff payment system provided a cost for each group. For primary care, as no tariff costs are available, we used estimated unit costs from the nearest available year. The cost of each primary care prescription was obtained by linking the therapy code to item-specific costs from the national drug tariff.
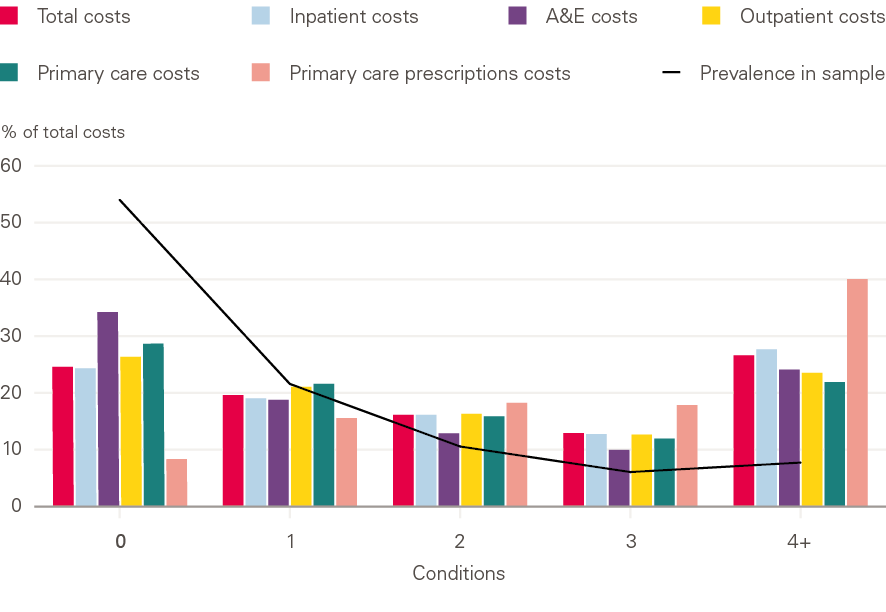
The costs we calculated are underestimates. First, the database we used did not include community care, specialist mental health care, or specialised commissioning. Second, it was not possible to get unit costs for around 15% of prescriptions, and GP administration costs were not included in our analysis. Despite the limitations of the dataset, however, the impact of the growing number of people with multiple conditions on the NHS is clear. Around 50% of hospital admissions, outpatient visits and primary care consultations were for people with 2+ conditions. Around 23% of hospital admissions, outpatient visits and primary care consultations and 26% of primary care prescriptions were for people with 4+ conditions (Figure 6).
This increased activity in the NHS translates into share of spending across primary and secondary care: over 55% of NHS costs (for hospital admissions and outpatient visits) and over 75% of the costs of primary care prescriptions were for people with 2+ conditions (Figure 7). This trend is likely to continue, with consequences for the resources needed to sustain the NHS. Hospitals have treated more and more patients with multiple conditions over the last decade. If this trend continues, total hospital activity will increase by 14% and costs by £4bn over the next 5 years.
Figure 6: Percentage of total health care use by number of conditions

Figure 7: Percentage of total health care costs by number of conditions
The same relationship between additional conditions and greater use of primary and secondary care is seen when we look at four specific clinical areas: cancer, cardiovascular disease, COPD, mental health conditions. In all four areas, the average cost per patient increased as the number of additional conditions increased (Table 1). It should be noted that our calculations do not necessarily include the cost of active treatment of cancer because our sample included all patients diagnosed in the previous 5 years. This is as we would expect: patients with more ill health use services more, which incurs greater costs. These higher costs do not fall equally across all parts of the NHS, and particularly affect spending on primary care prescribing.
Table 1: Mean health care costsa by number of additional conditions for patients with a clinical priority condition
|
Clinical priority condition |
NHS costs per additional conditions |
NHS costs relative to no additional conditions |
||||
|
0 |
1 |
2+ |
0 |
1 |
2+ |
|
|
Cancerb |
||||||
|
n |
732 |
936 |
2,407 |
732 |
936 |
2,407 |
|
Total costs |
£4,700 |
£5,600 |
£7,200 |
1 |
1.2 |
1.5 |
|
Inpatientc |
£2,700 |
£3,000 |
£3,600 |
1 |
1.1 |
1.3 |
|
Outpatient |
£1,500 |
£1,800 |
£2,000 |
1 |
1.2 |
1.3 |
|
Primary care consultations |
£300 |
£400 |
£700 |
1 |
1.3 |
2.3 |
|
Primary care prescriptions |
£200 |
£300 |
£700 |
1 |
1.5 |
3.5 |
|
Cardiovascular disease |
||||||
|
n |
1,094 |
2,012 |
9,865 |
1094 |
2012 |
9,865 |
|
Total costs |
£2,200 |
£3,000 |
£5,700 |
1 |
1.4 |
2.6 |
|
Inpatientc |
£1,100 |
£1,500 |
£2,800 |
1 |
1.4 |
2.5 |
|
Outpatient |
£500 |
£700 |
£1,200 |
1 |
1.4 |
2.4 |
|
Primary care consultations |
£300 |
£400 |
£700 |
1 |
1.3 |
2.3 |
|
Primary care prescriptions |
£200 |
£300 |
£700 |
1 |
1.5 |
3.5 |
|
Chronic obstructive pulmonary disease (COPD) |
||||||
|
n |
366 |
745 |
3,779 |
366 |
745 |
3,779 |
|
Total costs |
£2,400 |
£3,000 |
£6,300 |
1 |
1.3 |
2.6 |
|
Inpatientc |
£1,000 |
£1,200 |
£2,900 |
1 |
1.2 |
2.9 |
|
Outpatient |
£400 |
£700 |
£1,200 |
1 |
1.8 |
3.0 |
|
Primary care consultations |
£400 |
£500 |
£800 |
1 |
1.3 |
2.0 |
|
Primary care prescriptions |
£300 |
£500 |
£1,000 |
1 |
1.7 |
3.3 |
|
Mental health condition |
||||||
|
n |
9,782 |
8,130 |
14,880 |
9,782 |
8,130 |
14,880 |
|
Total costs |
£1,500 |
£2,600 |
£5,200 |
1 |
1.7 |
3.5 |
|
Inpatientc |
£600 |
£1,000 |
£2,200 |
1 |
1.7 |
3.7 |
|
Outpatient |
£300 |
£600 |
£1,100 |
1 |
2.0 |
3.7 |
|
Primary care consultations |
£300 |
£500 |
£800 |
1 |
1.7 |
2.7 |
|
Primary care prescriptions |
£100 |
£300 |
£800 |
1 |
3.0 |
8.0 |
a Costs are means based on 2-year follow-up from 1 April 2014 and rounded to the nearest £100. Costs are estimated from activity in primary and secondary care and include primary care consultations, prescriptions, and hospital care (inpatient and outpatient) but do not include community care, some specialist mental health care, or specialised commissioning.
b All patients diagnosed with cancer in the previous 5 years are included in this table and so these costs do not include the cost of active cancer treatment for all patients, but this does not differ according to number of additional conditions.
c The majority of patients have £0 inpatient costs as they were not admitted to hospital in the 2-year follow-up period.
As shown in Table 1, people with cancer, cardiovascular disease or COPD and 2+ additional conditions have primary care prescription costs that are over three times the level for those with no additional conditions. The prescription costs are eight times as high for people with a mental health condition and 2+ additional conditions, compared with those with a mental health condition alone. The close link between physical and mental health, and the need to improve access to physical health care for people with mental health problems, is well recognised, and our findings demonstrate the need to sustain pioneering efforts to integrate treatment for mental and physical health conditions.
Socioeconomic deprivation and multiple conditions
The risk of having multiple conditions is greater in socioeconomically deprived areas. For example, 28% of people 65–74 years of age in the most-deprived fifth of England had 4+ conditions, compared with 16% in the least-deprived fifth. As shown in Figure 8, there is a graded relationship between deprivation and multiple conditions – even those with a medium level of deprivation have a greater risk of multiple conditions than those in the least deprived areas. Therefore, while initiatives targeted at the most disadvantaged areas may be a priority, it is also important to consider patients across the full socioeconomic spectrum when aiming to reducing the prevalence of multiple conditions.
Figure 8: Percentage of people with 4+ conditions by age and level of socioeconomic deprivation
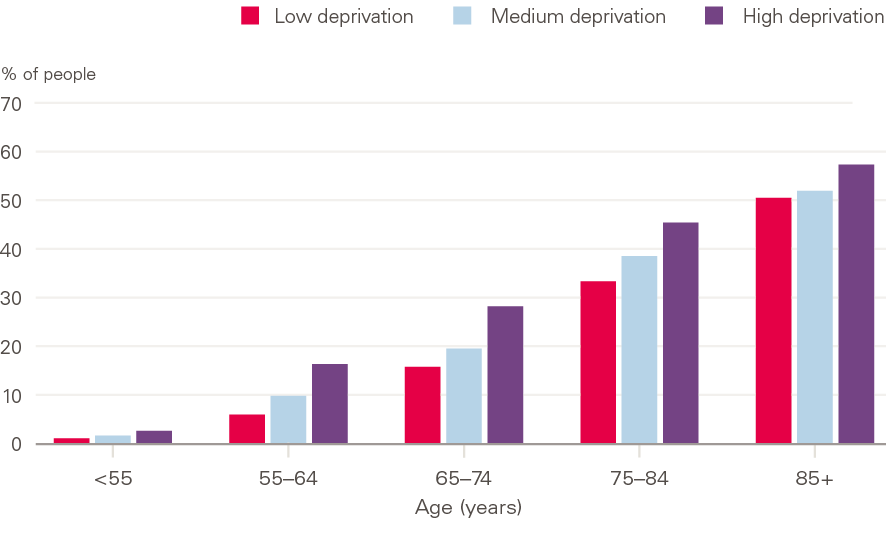
It is well known that the risk of having multiple conditions rises with age, but it is striking how deprivation adds to this risk. People living in the least-deprived fifth of England had an average of two conditions when they were aged 71, whereas those living in the most-deprived fifth reached the same level of illness a decade earlier, at 61 years of age (Figure 9).
Figure 9: Average number of conditions by age and level of socioeconomic deprivation
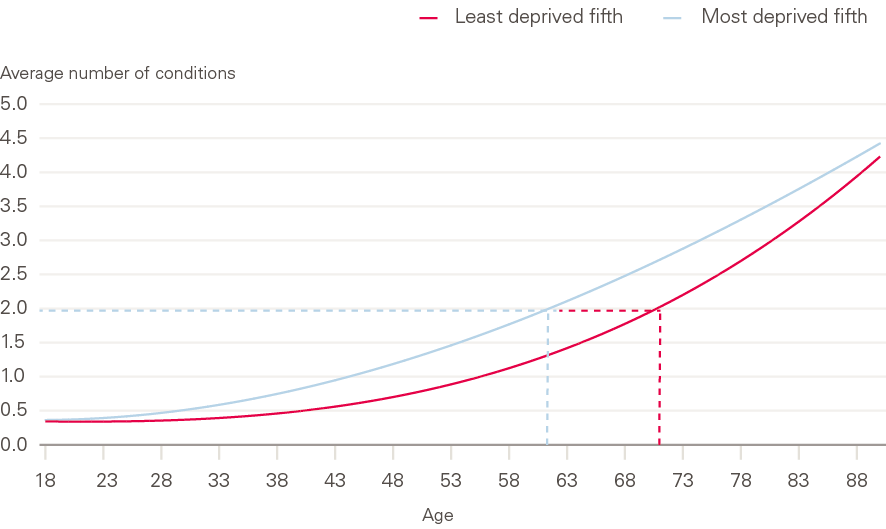
A similar picture was seen in a large Scottish study. Young and middle-aged adults in the most socioeconomically deprived areas had the same number of multiple conditions as those 10–15 years older in the least-deprived areas. These findings suggest that socioeconomic disadvantage accelerates when patients develop conditions and illness often associated with old age,,, resulting in high levels of multiple conditions among younger people in deprived areas. Having multiple conditions is a barrier to remaining in work. Policies to increase productivity and to extend working lives need to consider the impact of multiple conditions on working hours and workforce exit. Policies to reduce health inequalities require a focus on improving care for people with multiple conditions, since this group is concentrated in more disadvantaged areas.
Although living with multiple conditions is often thought of as a challenge of old age, our analysis and earlier studies have found that the number of people under 65 years of age with 2+ conditions is higher than the number aged 65 and over., Almost a third of people with 4+ conditions are under 65 years of age. At all ages, having multiple conditions is associated with greater use of health services. These analyses show that attention should be paid to multiple conditions in all parts of the NHS and other sectors, not only in services targeting frail, elderly people.
Implications for the NHS
Following the recent announcement that the government will increase NHS spending in England over 5 years from 2019, the NHS is putting together a long-term strategy on how this funding should be used and will then need to develop implementation plans.
While plans to target specific disease areas are important, our analysis shows that virtually everybody with cancer or a mental illness has additional conditions that can affect their
outcomes and need for care. We also show that the NHS faces significant challenges in meeting the needs of people with multiple health conditions, as this group is already using over half of NHS resources across primary and secondary care and could need an even bigger share in the future.
People with multiple conditions are at risk of receiving fragmented care across the various parts of the NHS. Without more joined-up care that recognises their needs, these patients may continue to experience poorer outcomes, such as increased mortality risk and longer length of stay, than patients with no additional conditions., We suggest six key steps that any long-term strategy and implementation plans should include to improve care for patients.
NHS long-term planning: Six steps to improve care for people with multiple conditions
1. Supporting those with multiple conditions to live well
People with multiple conditions are prescribed an average of 20 medications, and to manage their health may need to frequently attend GP appointments (over once a month in our analysis) and outpatient appointments (over four times a year). Daily life with multiple conditions can mean an overwhelming focus on symptom management and health care tasks.
A substantial proportion of people with complex health problems need support to manage their care. Over a quarter of people with multiple long-term conditions (and a third of those with multiple mental health conditions) report being overwhelmed by the requirements of managing their health, and these people are also least able to manage their health conditions. Of people with multiple conditions, those least able to manage their health are 17% more likely to attend a GP appointment, 32% more likely to attend an emergency department, and 38% more likely to have an emergency admission than those most able.,
There are many approaches, such as health coaching or peer support, to help people develop the knowledge, skills and confidence to manage their health conditions. Using tools that measure these abilities would show policymakers that patients vary widely in capacity and confidence, and track changes over time. It would also allow clinicians to identify those who could benefit most from extra support. While some areas are implementing health coaching and goal-setting with patients with health conditions, and NHS England is encouraging more areas to do this, the NHS could also do more to encourage patients to access peer support, including via online platforms.
As it is more common for people living in more-deprived areas to have multiple conditions, their clinical needs may be compounded by social factors. They might not have access to the financial support or community services that others in more affluent areas may have. Social prescribing – referring patients to non-medical, community-based sources of support – might be particularly valuable in more-deprived areas (if properly resourced). Examples of social prescribing include advice on finances, navigating access to local community groups to reduce isolation, and prescribing exercise to improve wellbeing and mobility. However, further investigation and evaluation of the effectiveness of social prescribing for people with multiple conditions is needed to identify which interventions should be prioritised.
Although initiatives such as social prescribing are important, a person’s health is the result of many factors, including their quality of housing, where they live, good quality work and affordable food. Therefore, urgent and cross-government action is needed to tackle the underlying causes of health conditions, along with investment in public services that affect people’s health. Furthermore, social prescribing is reliant on services and support being available in the community. These are often delivered by the voluntary or local government sector, which are both underfunded and not always available in the deprived areas where they are most needed. Therefore, social prescribing cannot be a substitute for continued efforts to address the underlying social determinants of health, and this is particularly relevant for those with multiple conditions who are more likely to live in deprived areas.
2. Developing new models of NHS care for those with multiple conditions
Meeting the needs of people with multiple conditions, at the same time as the NHS is treating more patients than ever, will require continued investment in developing new models of care. These models should be person-centred (ie their care should be focused on the needs of the person rather than on the needs of the service) and coordinated across primary, secondary, community and social care. Fragmented care poses a risk to quality and safety; for example, if care is duplicated or omitted, or if the trade-offs that can be inherent in managing multiple conditions are not properly recognised. Integrating care can reduce this risk. Integrating care also allows the needs of patients (not just clinical needs but social care needs, such as assistance with daily tasks or extra support on discharge from hospital) to be effectively coordinated by health and social care providers.
Integrated care is a feature of many of the vanguards in the New Models of Care Programme. For example, the Fylde Coast vanguard is aiming to provide an ‘extensive care’ service to people with multiple conditions (based on the CareMore model from the US). Following an assessment with the patient to identify their needs, a dedicated extensive care hub team takes over full clinical responsibility, providing all primary and secondary care. The patient is discharged back into the care of their GP when they are unlikely to further benefit from the extensive care scheme. An independent evaluation of this new model by the Improvement Analytics Unit (IAU), a partnership between NHS England and the Health Foundation, is underway.
Multidisciplinary care teams consist of practitioners who meet regularly to discuss the needs of their most complex patients and coordinate their care between them. They work together to manage complex situations and the needs of the patients. A recent evaluation by the IAU of multidisciplinary care teams in North East Hampshire and Farnham showed that they did not lead to lower emergency admissions for their patients, at least in the short term. However, these teams have the potential to reduce fragmentation in care and improve the patients’ experience of care.
3. Resourcing the vital role of primary care
Whatever new models are developed, the most important service for people with multiple conditions is still likely to be general practice. People with multiple conditions attend general practice more than any other NHS service and rely on GPs to coordinate their care. This role has been recognised by policymakers – improving the workforce, skills and infrastructure of general practice has been a priority since the publication of the Five year forward view for the NHS in England, while better coordination between general practice and other services, including social care and hospitals, has been an explicit aim of the New Models of Care Programme launched at the same time.
The General practice forward view, published in 2016, promised an additional 5,000 GPs by 2020/21. However, the latest data from NHS Digital suggests that far from this target being met, more GPs are leaving than joining. In March 2018, there were 33,686 full-time equivalent GPs: 235 fewer than in March 2017.
As we noted earlier, people are more likely to have multiple conditions if they live in socioeconomically deprived areas. Primary care practitioners, especially those working in more-deprived areas, need additional resources to provide the best care for their population. For many years, practices in more-deprived parts of the UK have had too few doctors relative to the health needs of their population.,, This fact is well recognised, and efforts to improve the distribution of the primary care workforce across different socioeconomic areas may be having some success. But challenges remain for professionals providing care and for people managing their conditions in the face of socioeconomic deprivation.
There are several ways in which primary care might better meet the needs of people with multiple conditions. Boosting continuity of care (eg seeing the same primary care practitioner over time) can improve patients’ experience of care and reduce emergency admissions. However, further research and improvement activity is needed to establish models of service delivery that achieve these gains. A ‘3D’ approach to care (based on dimensions of health, depression and drugs) that aimed to improve the continuity, coordination and efficiency of patients’ care by implementing practice-level changes was recently trialled. Significant improvements were seen in patients’ experience of well-designed, patient-centred care, but there was no measurable impact on quality of life or service use in the short term.
Further work is needed to develop primary care models that can improve outcomes for people with multiple conditions. The Royal College of General Practitioners has identified the importance of longer consultation time, continuity of care, medication reviews, multi-disciplinary teams, better collaboration with secondary care, better training, and a better-developed evidence base to provide tools and resources for GPs and patients. Our analysis shows that patients with multiple conditions have more consultations but not necessarily longer ones. More flexible appointment schedules, allowing for longer consultations at times, might benefit patients with multiple conditions, particularly in more-deprived areas.
The current shortage of GPs makes it hard to deliver a sustainable model of primary care, let alone develop and implement the sort of person-centred care that people with multiple conditions need. Proposed solutions must be mindful of the realities in general practice. The Health Foundation is currently working with five primary care teams to test approaches to improving continuity of care.
4. Designing secondary care around those with multiple conditions
Our analysis shows that having additional conditions is the norm for people with cancer, cardiovascular disease, respiratory disease, or a mental health condition. Specialists in secondary care services need to effectively organise and coordinate services for patients with multiple conditions. Traditionally, specialist advice is accessed in outpatient hospital departments, which are organised by clinical area. This disease-focused approach means that a patient with multiple conditions may be under the care of several specialists and may not receive person-centred care. There are examples of flourishing clinical alliances between different outpatient specialties and between outpatient specialists and primary care practitioners., Such models could be spread more widely and adapted for a wider range of patients.
Initiatives to reduce the treatment load for patients are also being tested. These include virtual clinics and co-located services (services located in the same physical location) so that patients don’t have to visit multiple outpatient departments. A workforce that is trained to care for patients with multiple conditions is also key for the NHS. The Royal College of Physicians has emphasised the need for generalism to be valued in medical training and medical careers. It has also highlighted the need to improve transitions between primary and secondary care. Collaborative planning for what is needed in secondary care and better sharing of information should improve continuity of care.
5. Using data and sharing information to improve care for those with multiple conditions
Sharing information within and across care providers is essential for integrated care models and to offer better joined-up care for patients. Sharing electronic records and other patient information should reduce the need for people to repeat their medical histories and care goals and reduce unnecessary, repeated tests. Sharing information should help those providing care to better understand the patient’s condition and context.
Incompatible information systems and lack of clarity on information governance are often barriers to timely information-sharing. The Local Health and Care Record Exemplars programme is supporting local areas to adopt best practice in collecting, protecting and sharing patient information to improve patient care. The Global Digital Exemplars programme is supporting digitally advanced providers to spread best practice and innovation in using information and technology. It aims to improve services by giving clinicians timely access to accurate information and patients access to their own records.
Linking data across health care and social care will allow the NHS to better plan services and track outcomes for people with multiple conditions. At present, it is difficult to understand how care in one part of the system depends on care in another part. Modelling can be used to predict future demand based on population projections or to test alternative scenarios where new initiatives are being considered. A system-wide view of the effects of service changes would be invaluable. To achieve this, greater investment in analytical capability is needed so that the NHS and its partners can turn data into insights.
6. Robustly evaluating what works
There are many unanswered questions about how to best care for people with multiple conditions. The challenge of caring for the rising number of people with multiple conditions is well known to practitioners and health system leaders, but there is not yet clear evidence on what works.
Encouragingly, research efforts are underway. A recent systematic review summarised the evidence from interventions in primary and community care. However, trials and other evaluations have so far only been able to report on short-term outcomes. Even if recent trials of new approaches have shown mixed results to date,, we need investment in the design and delivery of excellent health care services for people with multiple conditions. These models must be carefully evaluated in a timely and rigorous way.
An innovative partnership between NHS England and the Health Foundation is providing quantitative evaluation to show whether local change initiatives, implemented as part of major NHS programmes, are improving care and efficiency. The NIHR Applied Research Collaborations have signalled multimorbidity as a key challenge to be tackled. Learning from other health systems in international studies is also providing us with more evidence on what might work to improve care for people with multiple conditions (eg the Selfie Project and ICARE4EU)., Promising models must be identified and spread throughout the NHS.
Conclusion
Meeting the needs of people with multiple conditions at the same time as the NHS is treating more patients than ever is a complex challenge. Preventing people from developing conditions or delaying the onset of conditions will have the greatest benefits for individuals, their families, the economy and the NHS.
People living in more-deprived areas are at greater risk of developing multiple conditions earlier in life. To ensure that everyone has an equal opportunity to live a healthy life, urgent cross-government action is needed to tackle the underlying causes of multiple conditions, as is investment in the public services that affect people’s health.
At the same time, the high, rising number of people with multiple conditions and the level of NHS resources needed to provide treatment for them cannot be ignored. Long-term planning for the NHS needs to include a focus on those with multiple conditions, and find ways to galvanise and accelerate efforts to improve their care.
There are six key steps an NHS programme of work should include to improve care for patients:
- supporting those with multiple conditions to live well, for example by investing in self-management support for people with multiple conditions
- developing new models of NHS care for those with multiple conditions
- resourcing the vital role of primary care, particularly in deprived areas
- designing secondary care around those with multiple conditions
- using data and sharing information to improve care for those with multiple conditions, including greater data linkage
- robustly evaluating what works.
References
- Charlesworth A. Running to Stand Still – Why £20.5bn is a Lot But Not Enough to Do Everything. Health Foundation, 24 August 2018 (www.health.org.uk/Running-to-stand-still-why-20-5bn-is-a-lot-but-not-enough).
- Kingston A, Robinson L, Booth H, Knapp M, Jagger C. Projections of multi-morbidity in the older population in England to 2035: Estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018; 47: 374–80.
- Dayan M, Ward D, Gardner T, Kelly E. NHS at 70: How Good is the NHS? Health Foundation, 2018.
- Steventon A, Deeny S, Friebel R, Gardner T, Thorlby R. Emergency Hospital Admissions in England: Which May be Avoidable and How? Health Foundation, 2018.
- Kanesarajah J, Waller M, Whitty JA, Mishra GD. Multimorbidity and quality of life at mid-life: A systematic review of general population studies. Maturitas. 2018; 109: 53-62.
- Williams JS, Egede LE. The association between multimorbidity and quality of life, health status and functional disability. Am J Med Sci. 2016; 352: 45–52.
- Boakye D, Rillmann B, Walter V, Jansen L, Hoffmeister M, Brenner H. Impact of comorbidity and frailty on prognosis in colorectal cancer patients: A systematic review and meta-analysis. Cancer Treat Rev. 2018; 64: 30–9.
- Rushton CA, Satchithananda DK, Jones PW, Kadam UT. Non-cardiovascular comorbidity, severity and prognosis in non-selected heart failure populations: A systematic review and meta-analysis. Int J Cardiol. 2015; 196: 98–106.
- Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012; 50: 1109–18.
- Taskforce on Multiple Conditions. ‘Just One Thing After Another’: Living with Multiple Conditions. Richmond Group of Charities, 2018.
- National Institute of Health and Care Excellence. Multimorbidity: Clinical Assessment and Management [NG56]. National Institute of Health and Care Excellence, 2016.
- National Institute of Health and Care Excellence. Multimorbidity [QS153]. National Institute of Health and Care Excellence, 2017.
- Academy of Medical Sciences. Multimorbidity: A Priority for Global Health Research. Academy of Medical Sciences, 2018.
- Aiden H. Multimorbidity. Understanding the Challenge. Richmond Group of Charities, 2018.
- World Health Organization. Multimorbidity. World Health Organization, 2016.
- Whitty CJM. Triumphs and challenges in a world shaped by medicine. Clin Med. 2017; 17: 537–44.
- Barker I, Steventon A, Williamson R, Deeny SR. Self-management capability in patients with long-term conditions is associated with reduced healthcare utilisation across a whole health economy: cross-sectional analysis of electronic health records. BMJ Qual Saf. 2018; doi: 10.1136/bmjqs-2017-007635.
- Deeny S, Thorlby R, Steventon A. Reducing Emergency Admissions: Unlocking the Potential of People to Better Manage their Long-Term Conditions. Health Foundation, 2018.
- Ham C. Making Sense of Integrated Care Systems, Integrated Care Partnerships and Accountable Care Organisations in the NHS in England. King’s Fund, 20 February 2018 (https://www.kingsfund.org.uk/publications/making-sense-integrated-care-systems).
- Cassell A, Edwards D, Harshfield A, Rhodes K, Brimicombe J, Payne R, Griffin S. The epidemiology of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. 2018; 68: e245-51.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet. 2012; 380 (9836): 37–43.
- Payne RA, Abel GA, Guthrie C, Mercer SW. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ. 2013; 185: e221–5.
- Medicines and Healthcare Products Regulatory Agency. Clinical Practice Research Datalink [website]. Medicines and Healthcare Products Regulatory Agency, 2018 (www.cprd.com).
- Health Foundation. Information Governance and Data Security: Use of Patient Information. Health Foundation, 2018 (www.health.org.uk/information-governance-and-data-security-use-patient-information).
- University of Cambridge. CPRD @ Cambridge – Codes Lists Version 1.1 – October 2018. University of Cambridge, 2018 (https://www.phpc.cam.ac.uk/pcu/cprd_cam/codelists).
- NHS Digital. Patients Registered at a GP Practice – September 2018. NHS Digital, 2018 (https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice/september-2018).
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: A meta-analysis. Psychosom Med. 2004; 66: 802–13.
- Guys and St Thomas’ Charity. From One to Many: Exploring People’s Progression to Multiple Long-Term Conditions in an Urban Environment. Guys and St Thomas’ Charity, 2018 (www.gsttcharity.org.uk/what-we-do/our-programmes/multiple-long-term-conditions/one-many-exploring-peoples-progression).
- Patient Information Forum. Patient Experiences of Life with Long Term Conditions [webpage]. Patient Information Forum, 2015 (www.pifonline.org.uk/patient-experiences-of-life-with-long-term-conditions).
- Tzortziou Brown V, Patel I, Thomas N, Tomlinson J, Roberts R, Rayner H, et al. New ways of working; Delivering better care for people with long-term conditions. London J Prim Care (Abingdon). 2017; 9 (5): 60–68.
- Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care, 2006; 29: 725–31.
- Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: Cross sectional study of routinely collected, person level data. BMJ. 2017; 356: j84.
- NHS Improvement. Reference Costs [webpage]. NHS Improvement, 2017 (https://improvement.nhs.uk/resources/reference-costs).
- Personal Social Services Research Unit. Unit Costs of Health and Social Care [webpage]. Personal Social Services Research Unit, 2018 (www.pssru.ac.uk/project-pages/unit-costs).
- Mental Health Taskforce. The Five Year Forward View for Mental Health. Mental Health Taskforce, 2016.
- NHS England. Integrated IAPT Early Implementers [webpage]. NHS England, 2018 (www.england.nhs.uk/mental-health/adults/iapt/mus/sites).
- Department for Communities and Local Government. The English Indices of Deprivation. Department for Communities and Local Government, 2015.
- Marmot MG. The Status Syndrome: How Social Standing Affects Our Health and Longevity. Times Books, 2004.
- Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, Kivimäki M, et al. Health behaviours, socioeconomic status, and mortality: Further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med. 2011; 8: e1000419.
- Fiorito G, Polidoro S, Dugue PA, Kivimaki M, Ponzi E, Matullo G, et al. Social adversity and epigenetic aging: A multi-cohort study on socioeconomic differences in peripheral blood DNA methylation. Sci Rep. 2017; 7: 16266.
- Smith SM, Wallace E, O’Dowd T, Fortin M. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Syst Rev. 2016; 3: CD006560.
- Finch D, Bibby J, Elwell-Sutton T. Taking Our Health for Granted: Plugging the Public Health Grant Funding Gap. Health Foundation, 2018.
- NHS England. Models of Care [webpage]. NHS England, 2016 (www.england.nhs.uk/new-care-models/about).
- Hostetter M, Klein S, McCarthy D. CareMore: Improving Outcomes and Controlling Health Care Spending for High-Needs Patients. Commonwealth Fund, 2017 (www.commonwealthfund.org/publications/case-studies/2017/mar/caremore).
- NHS England. MDT Development: Working Toward an Effective Multidisciplinary/Multiagency Team. NHS England, 2014.
- Lloyd T, Brine R, Pearson R, Caunt M, Steventon A. The Impact of Integrated Care Teams on Hospital Use in North East Hampshire and Farnham. Health Foundation, 2018.
- NHS England. Five Year Forward View. NHS England, 2014.
- NHS England. General Practice Forward View. NHS England, 2016.
- Health and Social Care Information Centre. General and Personal Medical Services, England, March 2018 Final and June 2018 Provisional: Experimental Statistics. NHS Digital, 2018 (https://files.digital.nhs.uk/D0/35A78B/GPMS%20Mar%20Final%20Jun%20Prov%202018.pdf).
- O’Brien R, Wyke S, Guthrie B, Watt G, Mercer S. An ‘endless struggle’: Aqualitative study of general practitioners’ and practice nurses’ experiences of managing multimorbidity in socio-economically deprived areas of Scotland. Chronic Illn, 2011; 7: 45–59.
- McLean G, Sutton M, Guthrie B. Deprivation and quality of primary care services: Evidence for persistence of the inverse care law from the UK Quality and Outcomes Framework. J Epidemiol Community Health, 2006; 60: 917–22.
- Mercer SW, Fitzpatrick B, Guthrie B, Fenwick E, Grieve E, Lawson K et al. The CARE Plus study – A whole-system intervention to improve quality of life of primary care patients with multimorbidity in areas of high socioeconomic deprivation: Exploratory cluster randomised controlled trial and cost-utility analysis. BMC Med, 2016; 14: 88.
- Asaria M, Cookson R, Fleetcroft R, Ali S. Unequal socioeconomic distribution of the primary care workforce: Whole-population small area longitudinal study. BMJ Open, 2016; 6: e008783.
- Salisbury C, Man M-S, Bower P, Guthrie B, Chaplin K, Gaunt DM et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet, 2018; 392 (10141): 41–50.
- Royal College of General Practitioners. Responding to the Needs of Patients with Multimorbidity: A Vision for General Practice. Royal College of General Practitioners, 2016.
- Health Foundation. Increasing Continuity of Care in General Practice [webpage]. Health Foundation, 2018 (www.health.org.uk/programmes/increasing-continuity-care-general-practice).
- Winpenny EM, Miani C, Pitchforth E, King S, Roland M. Improving the effectiveness and efficiency of outpatient services: a scoping review of interventions at the primary-secondary care interface. J Health Serv Res Policy, 2017; 22: 53–64.
- Thomas R. Dacre: Ignore Generalist Training at Your Peril. Health Service Journal, 7 July 2015 (www.hsj.co.uk/commissioning/dacre-ignore-generalist-training-at-your-peril/5087162.article).
- Farneden J, Singh I. Local Health and Care Record Exemplars. Local Government Association, NHS England, 2018.
- NHS England. Global Digital Exemplars [webpage]. NHS England, 2018 (www.england.nhs.uk/digitaltechnology/connecteddigitalsystems/exemplars).
- Corbett J, d’Angelo C, Gangitano L, Freeman J. Future of Health: Findings from a Survey of Stakeholders on the Future of Health and Healthcare in England. Rand Corporation, 2017.
- National Institute for Health Research. Applied Research Collaborations [webpage]. National Institute for Health Research, 2018 (www.nihr.ac.uk/funding-and-support/funding-to-support-research/funding-to-support-research-in-the-nhs/applied-research-collaborations.htm).
- Selfie 2020. What is the Selfie Project [webpage]? Selfie 2020, 2018 (www.selfie2020.eu/selfie-project).
- ICARE4EU. ICARE4EU [website]. ICARE4EU, 2018 (www.icare4eu.org).
- Horton T, Illingworth J, Warburton W. The Spread Challenge. Health Foundation, 2018.