Key points
- Despite extensive evidence of the impact of social determinants on people’s health, public discourse and policy action is limited in acknowledging the role that societal factors such as housing, education, welfare and work play in shaping people’s long-term health.
- There are many reasons for this, but one factor that merits greater attention is the way in which the evidence is communicated to and understood by the public. Building public awareness and understanding is a necessary foundation for securing social change.
- The Health Foundation is working with the FrameWorks Institute to develop a deeper appreciation of the ways in which people understand and think about their health in order to develop more effective approaches to communicating evidence.
- Surveys of public attitudes suggest that the public consider individual behaviours and access to health care to have the greatest effects on health.
- FrameWorks has identified a range of ‘cultural models’– common but implicit assumptions and patterns of thinking – that give deeper insight into how people think about what makes them healthy.
- Understanding which cultural models promote – or obscure – people’s awareness of the importance of social determinants is an important first step in developing effective ways of framing the evidence.
- The media can reflect and shape public thinking. Analysis of media narratives about health by FrameWorks showed that they tended to reinforce individualistic ways of thinking about health.
- This briefing presents the main findings of research commissioned by the Health Foundation and carried out by FrameWorks. It also presents findings from questions sponsored by the Health Foundation in the 2017 British Social Attitudes survey.
Introduction
Good health is important for both individuals and society as a whole, but not everyone has the same opportunities for good health. Extensive research has shown that differences in social and economic circumstances lead to deep inequalities in health outcomes.,, For example, there is currently a 19-year gap in healthy life expectancy between women in the most- and least-deprived areas of the UK.
Yet public, media and policy discourse tends to be dominated by concerns about the NHS and issues such as diet, exercise and smoking. This means that public debate rarely acknowledges the health effects of issues like housing, education, welfare and transportation. As a result, policy and investment decisions often miss opportunities to protect and enhance health. For example, while investment in the health care system in England has increased in recent years, there have been deep cuts to public spending in areas relevant to the social determinants of health, including public health.
If the necessary action to improve health and reduce health inequalities is to be taken, there needs to be greater awareness of the social determinants of health, beyond those working in the field. This type of policy shift – like shifts on other social issues such as tobacco control, use of plastics and climate change – is only achieved when it is in step with broader public opinion.
Achieving such a change in public attitudes is difficult, but not impossible. It requires careful and effective communication of the evidence, which in turn needs to be informed by a detailed understanding of the public’s prevailing views and assumptions. How a message is understood depends on people’s underlying beliefs, which shape the way they interpret the information they receive.
The FrameWorks Institute – an independent, non-profit organisation – works with organisations and social movements to discover the patterns in public thinking and discourse that impede social change and identify reframing strategies that can drive change. They start from the premise that how communicators choose to frame issues – how they present information, including what they emphasise, how they explain things and what they don’t say – influences how people make sense of and engage with these issues. In turn, adopting better ways of framing issues can lead to changes in the way the public thinks about and engages with these issues.
Using this methodology, FrameWorks explored public understanding of the social determinants of health. This work identified several distinct challenges that need to be understood and addressed in order to better communicate the evidence on the issue.
This work is designed to inform and empower public health professionals, policymakers, civil-society leaders and anyone who has an interest in promoting a broader understanding of how to build a healthier society. The second stage of this work, planned for 2019, will develop and test detailed messages and tools for communicating the social determinants of health more effectively.
Box 1: What are the social determinants of health?
The social determinants of health, also known as the wider determinants of health, are the conditions in which people are born, grow, live, work and age. They include social, cultural, political, economic, commercial and environmental factors.
The strongest influences on people’s health are social determinants such as their level of education, income, quality of housing and employment.
What do the public currently think about health?
Surveys give some insight into current public attitudes to health. NatCen’s British Social Attitudes survey is an annual survey of around 3,000 (population-representative) people on a range of social issues. In 2017, the Health Foundation sponsored a set of questions in the survey to understand public attitudes to the social determinants of health and responsibility for health.
The responses to these questions show there is a strong connection in people’s minds between health and health care, and a strong belief in the impact of individual behaviours (‘lifestyle factors’) on health (see Figure 1). Almost three-quarters (73%) thought access to free health care has a very large impact on health, and almost three-fifths (59%) thought individual behaviours have a very large impact on health.
By contrast, other determinants – such as education, employment, social support and the area in which someone lives – were rated as considerably less important by the public in terms of their impact on health.
Figure 1: Proportion of people who think that different determinants have a ‘very large’ or ‘quite large’ impact on people’s health
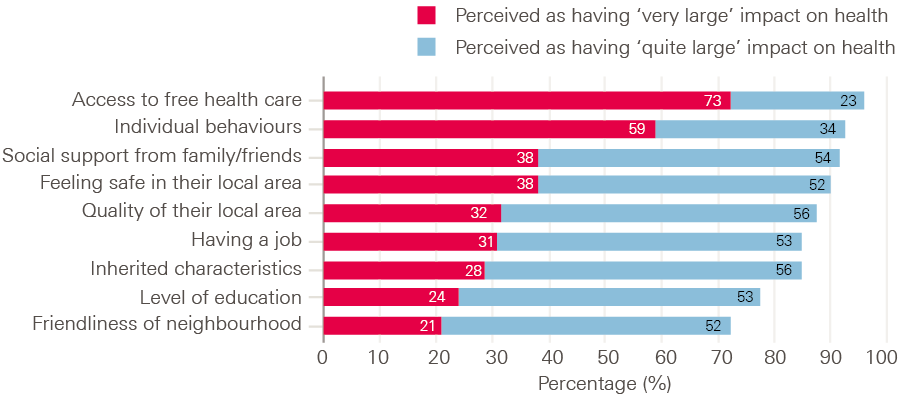
Source: British Social Attitudes survey 2017 (n=2,942).
Only 1% of respondents thought the government was entirely responsible for people’s health, while almost a third (30%) thought individuals were entirely responsible for their own health (Figure 2).
Figure 2: Public attitudes on the extent to which the individual or the government is responsible for a person’s health
Source: British Social Attitudes survey 2017 (n=2,942).
These findings point to a prevailing view that health care and individuals’ choices are the primary drivers of health. However, survey findings of this kind are limited in how far they can explain public understanding of complex issues. Although these results make clear that health care and individual behaviour dominate public thinking, they do not explain why. This makes it difficult to know how to shift the public’s attention toward, and change public thinking on, societal factors. In addition, the results are strongly influenced by the wording and ordering of questions, and people may hold multiple, conflicting views on health, which survey methodologies such as those used in the British Social Attitudes survey cannot uncover. The research conducted by FrameWorks explores these nuances.
Understanding how the public thinks about health
While surveys of public attitudes help us understand what people think about health, they give limited insight into how people think. To broaden our understanding of the social determinants, we need a deeper understanding of the ‘cultural models’ – the assumptions, underlying beliefs and ways of thinking – that shape how people understand messages about health.
The research approach
FrameWorks conducted interviews with members of the public and those working in the field of social determinants of health, including academics, public health professionals and policy makers. Interviews with individuals working in the field of social determinants enabled FrameWorks to capture the ‘untranslated story’ of social determinants – the key ideas that members of the field want those not working in the field to understand or support. By comparing these with the way the public currently thinks about health, as captured by interviews with members of the public, FrameWorks were able to identify the gaps that must be bridged for the public to have a fuller understanding of the social determinants of health.
FrameWorks, in consultation with the Health Foundation, selected interviewees working in the field of social determinants to reflect a diversity of perspectives and areas of expertise. In 13 semi-structured, 1-hour interviews, researchers asked questions and used hypothetical scenarios designed to capture their understanding of what a healthy society is. They used follow-up questions to encourage the interviewees to elaborate on and clarify their answers. The interviews were analysed using a grounded-theory approach, in which researchers identified common ideas and categorised them, allowing themes to emerge from the data.,
Members of the public were interviewed using semi-structured, 2-hour interviews exploring their understanding of health, allowing researchers to capture the broad implicit assumptions and patterns of thinking (cultural models) that people use to make sense of the topic. Participants were selected for interview through a market-research organisation, based on criteria that were chosen to ensure the demographics of the sample were similar to that of the UK population. Interviews were analysed using ‘cultural models’ techniques, which are not designed to identify differences in understanding between population sub-groups, but rather, to identify common ways of thinking. The sample of 36 participants contained enough demographic variability (for example in age, gender, ethnicity, education, political affiliation and income) to ensure that identified patterns of thinking are truly shared across demographic lines.
By analysing these interviews, FrameWorks identified a series of cultural models that underlie how the British public thinks about health (Box 2).
Box 2: Cultural models
Cultural models are common, but implicit, assumptions and patterns of thinking that underlie how people make sense of the world around them.
People may draw on multiple, conflicting models to think about any given issue. Different models may be activated in people’s minds at different times, though some are dominant and used more consistently than others. Understanding which cultural models are most productive, and which are most likely to obscure people’s understanding, is an important first step in developing effective ways of framing an issue.
The cultural models referred to in this briefing are as follows:
- Absence of illness: defining health as not being ill, rather than as a positive state of wellbeing.
- Health is medical: understanding health primarily in relation to medicine, doctors and health care.
- Health individualism: understanding health outcomes as being driven primarily by individual choice.
- Mentalism: explaining individual behaviour as the result of individual discipline and willpower, or a lack thereof.
- Genetic exception: using genetics and ‘fate’ to explain exceptions to the rule or cases where health cannot be explained by individual choice.
- Health consumerism: a belief that money allows people to buy good (or better) health by adopting healthy individual behaviours such as healthier diets or access to a gym.
- Behavioural constraints: recognising that social and environmental factors affect individual health outcomes by restricting or encouraging particular behaviours.
- Cultural norms: seeing communities or family units as having accepted standards about what is ‘normal’ and ‘healthy’, and that health outcomes are a result of these.
These cultural models fall into two broad strains of thought:
- an individualistic strain, which assigns a central role to individual choice and willpower – for example, the health individualism and mentalism cultural models
- an ecological strain, which sees health, at least in part, as a product of social and environmental influences – for example, the health consumerism and behavioural constraints cultural models.
The research found the individualistic strain to be dominant in public thinking.
More details of the research methods, samples and findings are available in reports by FrameWorks.,
Communicating the social determinants of health
FrameWorks’ research identified four communication challenges that can act as barriers to wider public acceptance of the evidence on social determinants of health.
Challenge 1: Broadening what is understood by the term ‘health’
Participants initially tended to understand health as an absence of illness, defining health primarily by what it is not, rather than what it is. One interviewee said:
‘Good health is never having to go to the doctors. Ironically, good health is never having to use the NHS. I say ironically because of how much I respect the NHS, but if I never have to use it […] that’s good health.’
This also illustrates the strong connection in public thinking between health and medicine. The members of the public interviewed saw health as being a medical issue. They saw doctors and health professionals as authoritative voices on how to maintain health through daily behaviours, and they saw medicine as offering innovative ways to treat illness.
By contrast, individuals who work in the field of social determinants of health spoke of a healthy society as one in which people can experience physical and mental wellbeing, make meaning of their lives and have the sense of control needed to pursue life goals. This difference in the understanding of health leads to different ideas about how to maintain and improve health.
Viewing health as an absence of illness makes it difficult for people to think explicitly about how health might be created, as well as narrowing people’s focus to clinical treatment and individual-level prevention.
Challenge 2: Increasing understanding of the role of social determinants of health
The predominance of the individualistic strain of thinking was illustrated by how members of the public thought about the factors that shape people’s health. They assumed that choices relating to diet, exercise, smoking and drinking alcohol are the primary influences on health. When thinking in this way, people assigned responsibility to individuals for making healthy choices. This led some to assume that when people experience poor health, it is their own fault.
‘Yeah, that “responsibility” word – it starts with you, and it ends with you. Nobody else is responsible for you – nobody.’
Within this strain of thinking was the ‘mentalism’ model – seeing individuals’ choices as primarily determined by their self-discipline and willpower. This way of thinking was also applied by many participants to mental health issues such as depression and anxiety, which were seen as being determined by an individual’s mindset.
By contrast, those working in the field of the social determinants argued that health is a product of societal systems. Individual behaviour, they said, is strongly constrained and shaped by social and environmental factors. As a result, individual behaviours should be seen as the endpoint in a long chain of causes and consequences that produce health outcomes.
Another way that public participants thought about health, linked to the individualistic strain, was the ‘genetic exception’ model: where they could not explain health outcomes through individual choice or willpower, people often turned to genetics or fate to account for these exceptions to the rule.
‘I’ve known people that have never smoked before in their life, but then got lung cancer. So, it’s not one thing leads to another. I think sometimes you’re just a bit unlucky.’
When thinking in the individualistic strain, participants saw health outcomes as being determined either by individual choice and willpower, or by genetics. This led to a sharp distinction between self-inflicted and accidental illness; between the ‘deserving’ and ‘undeserving’ ill.
By placing all the emphasis on personal choice, they saw those who had an avoidable illness (such as lung cancer or obesity) as less deserving of care than those with a genetic illness (such as multiple sclerosis). One implication for communicators is that messages about an ‘NHS crisis’ may reinforce the view that limited health care resources should be targeted at those who are ‘more deserving’.
These results show that there is a big difference between experts and the public in terms of their underlying assumptions about the determinants of health. One of the main challenges for communicators is to shift the public away from individualistic ways of thinking about health and open up space for thinking about the role of social determinants.
Challenge 3: Increasing understanding of how social and economic inequalities drive health inequalities
Advocates of the social determinants of health described deep health inequalities among different groups as being driven by wider inequalities in power, wealth and resources. Public participants did recognise that certain neighbourhoods, cities or countries have better health than others, and so were able to recognise that social and environmental factors can lead to health inequalities. However, the ecological cultural models that people used to explain these differences only provided a partial understanding of how environments shape health, and they often fell back on more individualistic models to explain things.
For example, when thinking about the link between wealth and health, participants applied a health consumerism cultural model, explaining actions in terms of purchasing power. They assumed that wealthier people can buy good health through being able to afford the best foods, gym memberships, housing and private health care.
‘[People with money] might be able to buy the more healthy options. Trying to eat healthily does cost more money than the junk food.’
Public participants also described how social and environmental factors can restrict or encourage certain behaviours – the ‘behavioural constraints’ model. For example, they recognised that a time-consuming job can make it harder for people to eat well or take enough exercise.
However, both the health consumerism and behavioural-constraints models were relatively weak. Participants often defaulted to more individualistic strains of thought, as illustrated by the following quote:
‘I think you always have a choice… And I think anyone on any budget could work a way out to eat relatively healthy food or significantly less bad food.’
A common explanation for health differences between communities focuses on cultural norms. When thinking in this way, public participants assumed that communities or family units set different norms about what is healthy, and that these in turn shape individual behaviour in a way that is almost inescapable. They thought some cultural norms promoted health while others were detrimental to health.
‘There are some people in [working-class] communities that don’t work… I think there’s just a culture at the moment where a lot of people are just after free handouts. It’s unhealthy, and it’s unproductive. I think if you’re not working, you’re sitting around watching telly. You’re just hanging about doing nothing. I think that has a big impact on your health and your life expectancy.’
So while people active in the field of social determinants of health saw health inequalities as being driven by wider inequalities in power, wealth and resources, the members of the public interviewed often explained them wholly in cultural terms. This ‘cultural norms’ model of thought can obscure structural inequities and further contribute to the stigmatisation of ill health. It can lead to health inequalities being seen as resulting from a ‘bad culture’ as well as poor individual choices.
Although members of the public had some productive – and some less productive – ways of thinking about ecological influences, there was a lack of awareness among participants of how racism, discrimination and other types of power imbalances generate health inequalities. People had a sense that discrimination and stigma can be a consequence of certain types of health problems, but they tended not to think of them as a determinant of health, and struggled to understand how inequalities in power might affect health outcomes.
Communicators, therefore, need strategies for bringing a range of ecological models forward in the public’s thinking and deepening the way they think about social determinants to better reflect the full range of ways in which our environments shape our health.
Challenge 4: Generating an understanding of the policy action needed to keep people healthy
When thinking about how health can be fostered for society as a whole, the public participants focused primarily on ‘raising awareness’ and health care. These solutions flowed directly from assumptions about what health is and how it is shaped. When people thought about health as being primarily shaped by individual choice, they saw raising awareness as the obvious solution, because the only thing society can do is provide information for people to make ‘good’ choices. And when health was associated with medicine, health care was the default solution. These patterns were illustrated in one participant’s answer to a question about the role of government:
‘One part is awareness. The other part is the NHS – obviously huge. It accounts for just under a third of all government spending. So, obviously, the government is responsible for that. Anything I can’t do, the government should be responsible for. I can’t install a pacemaker. I can’t set a broken bone. I can’t stitch up a giant gash in my neck.’
By contrast, those working in the field of social determinants argued that the way to create a healthy society is through increased investment in public services that protect and improve the health of the population over the long term. In this view, while the NHS is important, the protection of the NHS budget at the expense of other health-creating services puts the long-term wellbeing of the population at risk.
Communicators advocating for broader public policy solutions to health issues, therefore, need effective ways of explaining how public investment and policy in these areas can lead to improvements in individual health.
How does the media talk about health?
The media both reflects and shapes public thinking. Understanding how the media communicates issues around health and health inequalities helps us understand both the challenges and opportunities we face in broadening out the debate on health. As part of their research, FrameWorks analysed a random sample of 209 newspaper articles about health and 182 materials from third-sector organisations to identify common narratives about the determinants of health.
They found that these narratives tended to reinforce an individualistic understanding of health. When discussing the determinants of health, media materials mentioned behavioural factors slightly more often than social factors. However, tellingly, when talking about solutions they focused primarily on the role of individuals and families (for example, raising public awareness or encouraging different dietary choices) and health care (Figure 3).
Figure 3: Who is targeted by the solutions mentioned in 209 newspaper articles about health in 2016?
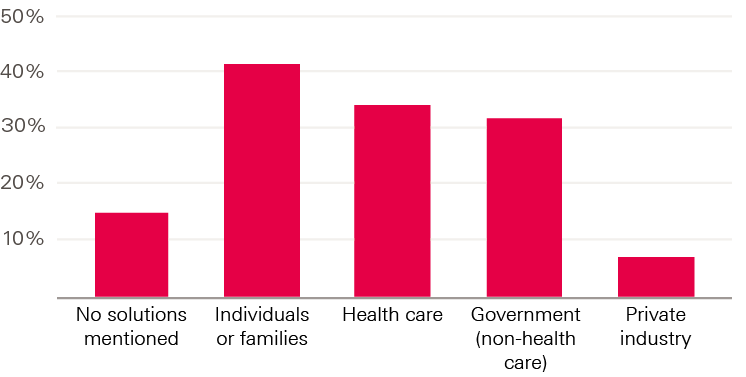
Source: Adapted from Levay et al.
One common media narrative – ‘health consumerism’ – locates the causes of, and solutions to, health issues entirely in people’s choices and behaviours; social and environmental factors are wholly absent from this narrative. This approach addresses the readers as consumers, and highlights the importance of individuals’ decisions about purchasing various products – for example, healthy food or gym memberships.
Where media stories discussed solutions to health problems, they similarly focused on changes in individual and family behaviour, and health care. This narrative can constrain the public’s appreciation of the available solutions for improving health and reducing health inequalities.
The media analysis also found a lack of discussion about health inequalities in the news (Figure 4). While there was some limited discussion about health inequalities in relation to location, gender or socioeconomic status, there was very little in relation to factors such as ethnicity, sexual orientation or disability. This means that the public does not consistently hear about the true scale and nature of health inequalities, much less the inequalities in power that underlie them.
Figure 4: Level of attention devoted to health inequalities in 209 newspaper articles about health in 2016
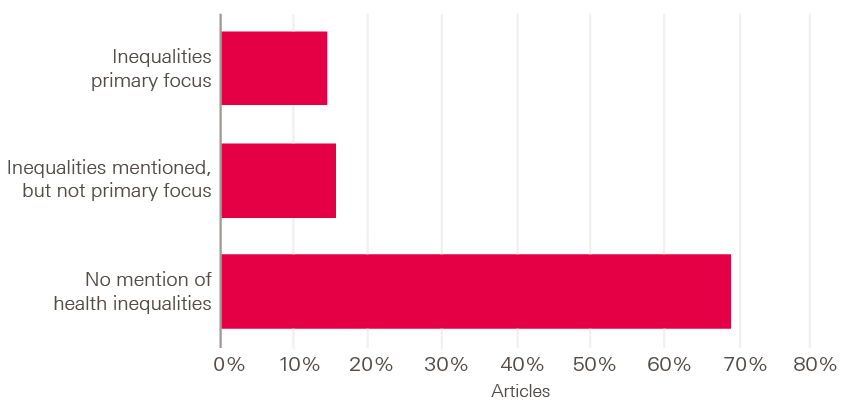
* FrameWorks researchers selected a random sampling of articles (print and online) from these sources using a search strategy designed to capture a range of topics related to health. Details are given in Levay et al.8
Implications for communicators
To build support for the policies and programmes that are needed to improve health and reduce health inequalities, there needs to be a wider awareness and understanding of the social determinants of health. The research outlined in this briefing illustrates some of the challenges that exist in communicating these issues.
Although the research found that the way the members of the public involved think about health is multi-faceted, the dominant individualistic strain undermines support for policies and initiatives that focus on social determinants. However, this strain of thought sits alongside cultural models that are more productive, as people do recognise a role for social and environmental factors. The challenge for advocates of a social-determinants approach is to find ways to build on this ecological strain to create a more expansive way of thinking about health.
The next stage of this work is to develop and test detailed strategies to address the communication challenges outlined in this briefing. However, based on the work done so far, and previous work done by FrameWorks, we can outline some preliminary implications for those wanting to communicate more effectively on these issues:
- Beware of gesturing towards the importance of individual choice or responsibility. Communicators may be tempted to open discussions by acknowledging the role of the individual and then pivoting to their message. Communications research has found gesturing in this way toward an unproductive understanding to be unhelpful in most situations – it reinforces existing ways of thinking, rather than challenging them.
- Avoid ‘crisis messaging’. Rising rates of chronic disease are often described as ‘epidemics’ and the strains on the NHS as a ‘crisis’. While this is intended to increase people’s sense of urgency and motivation, research shows that crisis messaging frequently backfires by reinforcing people’s sense of fatalism. The result is often less support for solutions and rapid disengagement from the issue.
- Use step-by-step, causal explanations of how social determinants affect health. Outlining the causal links between different social and environmental factors and health outcomes is critical to deepening the public’s understanding of how these factors shape health.
- Provide concrete examples of how the social determinants influence people’s health to expand the public’s awareness of possible solutions. This is essential to cultivate an understanding of how health can be built at the societal level.
Next steps
In 2019, the Health Foundation will work with FrameWorks to develop and test strategies to reframe the health debate. This will include the development of publicly available tools to help people communicate more effectively about the social determinants of health. We want to involve stakeholders who are communicating about health and the social determinants of health, including public health professionals, policymakers and activists, in the development of these messages.
To find out more about the project and download the first two research reports,, visit www.health.org.uk/framing-health. And if you would like to be involved in this work, please get in touch with us at info@health.org.uk.
References
- Department of Health and Social Security. Inequalities in Health: Report of a Working Group Chaired by Sir Douglas Black. DHSS, 1980.
- Acheson D. Independent Inquiry into Inequalities in Health: Report. TSO (The Stationery Office), 1998.
- Marmot M. Fair Society, Health Lives: The Marmot Review. The Marmot Review, 2010.
- Office for National Statistics. Health State Life Expectancies, UK: 2014 to 2016. Office for National Statistics, 2017.
- Finch D, Bibby J, Elwell-Sutton T. Taking Our Health for Granted: Plugging the Public Health Funding Gap. Health Foundation, 2018.
- Lovell N, Bibby J. What Makes Us Healthy? An Introduction to the Social Determinants of Health. Health Foundation, 2018.
- Glaser B, Strauss A. The Discovery of Grounded Theory; Strategies for Qualitative Research, Observations. Aldine PubCo, 1967.
- Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Sage Publications, 1990.
- Levay K, Gibbons C, Down L, O’Neil M, Volmert A. Only Part of the Story: Media and Organisational Discourse about Health in the United Kingdom. FrameWorks Institute, 2018.
- L’Hôte E, Fond M, Volmert A. Seeing Upstream: Mapping the Gaps Between Expert and Public Understandings of Health in the United Kingdom. FrameWorks Institute, 2018.