Introduction
The idea of partnerships and collaboration across organisational boundaries is not new in the NHS in England, but it is reaching a zenith in policymakers’ minds. The 2017–19 planning guidance for the NHS put it simply: partnership behaviours are becoming ‘the new norm’ and ‘What makes most sense for patients, communities and the taxpayer should always trump the narrower interests of individual organisations.’
This idea underpins the sustainability and transformation partnerships and the new models of care set out in the Five year forward view for the NHS in England. It also builds on the experience of initiatives that have been tried over the past decade, ranging from new forms of organisational links (eg buddying and franchises) to building networks and communities of practitioners to help improve health service delivery.
The Health Foundation has contributed to developing the evidence base for networks – for example, by funding programmes to help clinical communities improve quality of care in specific areas of practice, reviewing how to develop and manage effective networks to support quality improvement, and developing Q, a connected community of people who have improvement expertise from across the UK.
But less is known about what makes for successful partnerships between providers at an organisational level. For this reason, the Health Foundation commissioned the Health Services Management Centre (HSMC) at the University of Birmingham to look at a range of current organisational partnerships, and draw some tentative learning to help inform and guide both policymakers and providers.
This briefing by the Health Foundation and HSMC summarises the main findings of the research report and what providers and policymakers can learn. The research report, Partnering for improvement: inter-organisational developments in the NHS, is available at www.birmingham.ac.uk/partnering-for-improvement.
What did the research find?
Partnering is an integral part of improvement efforts
Preparatory interviews with national stakeholders by the HSMC research team confirmed that partnering will be a central component of efforts to improve services for the foreseeable future. Policymakers now expect that all provider organisations should explore how partnering could improve services within the local health economy, as well as in their own organisations.
Partnering is also a clear theme in many national policy documents. The need to move beyond organisational boundaries to improve services for patients was emphasised in the Five year forward view in 2014 and in Sir David Dalton’s review of options for NHS providers later that year. Both reports outline the range of ways that two or more providers could work in partnership to improve quality of care for patients, from joint ventures and management contracts to primary and acute care systems and hospital chains.
The language of both the Dalton review and the Five year forward view emphasises a degree of voluntarism – there is no ‘one size fits all’ model for provider organisations or for service delivery, and providers should select and adapt the approach that best suits their own aims and objectives. But some of the most recent examples of partnering have been mandatory, and involve building relationships between organisations when there may be a power imbalance between the two. An example of this is buddying, introduced in 2013 as part of the special measures regime. Special measures were created following the report of the Mid Staffordshire NHS Foundation Trust Public Inquiry, and trusts placed into special measures have to be buddied with high-performing trusts for advice and support, as part of a regulated programme of improvement.
Many different types of partnership can be applied
The preparatory background research for this project established that partnerships in the NHS may:
- take many different shapes and forms, with a range of ambitions, objectives and mechanisms to drive improvement
- range enormously in scope, from small-scale collaborations between individual clinicians to the structural integration of entire organisations
- be initiated voluntarily to pursue opportunities for improvement, or be mandated by regulators as part of a response to organisational or quality failures.
From this initial sweep of examples, the HSMC research team developed a typology to reflect current interests and practice in partnering in the NHS (Table 1), which vary in terms of nature, scale and form.
Table 1: Typology of interests and practice in partnering in the NHS
|
Nature |
|
|
Mandated: |
Partnering that has been brokered by a body outside of the organisation, such as a regulator. |
|
Voluntary: |
Partnering that has been instigated by the involved organisations. |
|
Scale |
|
|
Individual: |
Partnering that primarily occurs through a limited number of individuals or services within the partner organisations. |
|
Structural: |
Partnering which is of larger scale and more formally constituted. This could include mergers, acquisitions and contractual agreements. |
|
Form |
|
|
Merger: |
Partnering where two organisations combine their resources to form a new organisation. |
|
Acquisition: |
Partnering where one organisation becomes subsumed by another. |
|
Buddying: |
Partnering where individuals or organisations with more experience help, mentor, advise, or train others. |
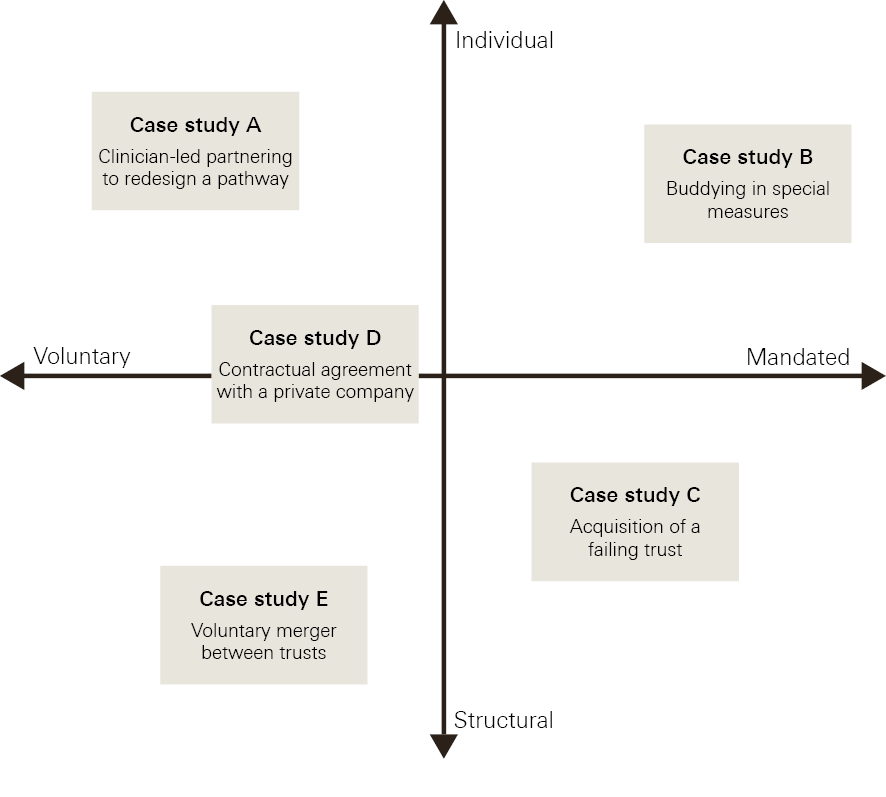
A rapid review of the literature (summarised in the full report) suggested that most research has focused on the impact of structural mergers and acquisitions between health care providers. Studies show that realising financial or quality benefits from mergers of health care organisations is far from straightforward and often takes years to materialise. On the other hand, while buddying schemes are popular across occupational sectors, there is little academic research available on the effects or effectiveness of these more informal forms of partnership. Accordingly, the research team selected five case studies to explore examples situated on different points of the typology above (Figure 1).
Figure 1: Typology of the five case studies explored in the research
* Stakeholder interviews were completed with representatives from: the Department of Health; arm’s length bodies, including the Care Quality Commission, and Monitor and the Trust Development Authority (before these two organisations merged to become NHS Improvement); representative bodies; NHS trusts and foundation trusts with experience of improvement; and academics with expertise in this area of policy and practice.
What did the case studies show?
At the site of each of the five case studies, 10–12 people were interviewed, including representatives from the executive directors, senior managers, clinicians and support staff. The interviews explored perceptions and experiences of the partnerships, and asked about factors that might have led to any improvements in quality. To fulfil ethics and governance requirements, and the wishes of some of the participants, the case studies are anonymised.
Voluntary partnering at an individual level – case study A
Clinician-led partnering to redesign a pathway
Riverside is a specialist NHS centre for respiratory medicine and Valley High is one of the local district hospitals. Home ventilation services were traditionally initiated by Riverside, with patients at Valley High waiting to be transferred despite being otherwise ready for discharge. The partnering arrangement was developed by two clinicians and has led to patients starting home ventilation at Valley High. Following discharge, patients have a follow-up assessment at Riverside to make sure the equipment is configured correctly and patients are confident in how to use it.
Outcome of the partnership
This is an example of a partnership built out of a strong professional connection between two consultants in different organisations.
‘It was a Saturday... I saw the patients waiting were from Valley High, and so I just wrote an email one Saturday saying “Do you think we could do this?” and he said “Interesting, I was just going to write the same thing to you.”’
Consultant (Riverside)
Their proposal to work together to redesign the pathway was received positively by their teams, and underpinned by the team members’ respect for the two lead consultants. The project involved some changes, including adding new responsibilities for staff at Valley High, and required the collaboration of nurses and technicians across the two trusts.
This partnership was done without additional resources and, although it needed the backing of operational managers and the boards from both trusts, it did not place demands on the wider organisation. No formal quality improvement methods were used, and staff carried out the additional activity within their normal working routines, using existing systems (for example, email was used instead of an electronic referral system). At the time of the interviews, the partnership had been running for 12 months, and interviewees felt it had improved patients’ experience by shortening stays in hospital and enabling patients to be at home for longer. Formal evaluation and monitoring has yet to take place, but is planned, and the clinical team strongly believes that the partnering arrangements should be sustained and probably expanded in the future.
‘it’s a very manual, very personal service, which is fine, but once it starts expanding, you have to kind of industrialise the process and the scale. So we’ve been talking internally about how do we create more formalised referral routes in and some form of workflow that sits behind it.’
Operational manager (Riverside)
Mandated partnering at an individual level – case study B
Buddying in special measures
Green Bay NHS Trust is a multisite acute hospital provider that was placed into special measures by the Care Quality Commission (CQC). As part of an organisation-wide improvement effort, it engaged in a number of partnering activities. This included buddying with another trust, Regency Vale NHS Trust, and being connected with a US-based institute and a number of consultancy firms.
Outcome of the partnership
This partnership was formed in the upheaval after Green Bay NHS Trust was placed into special measures, which resulted in replacement of the board and an overhaul of the management and governance systems. The buddying arrangement was set up to support the new chair and chief executive, and drew on a previous working relationship.
‘It was a mentoring arrangement... the Trust and I worked together in the past so we knew each other very well... the approach by this Trust wasn’t to invite another organisation to take us over or to send in all their troops because that wouldn’t help them, they have a job to do as well. It was to test whether the approach we were taking was actually sensible, pragmatic and would stand up to scrutiny.’
Chair (Green Bay NHS Trust)
Board members from both trusts framed this arrangement more as a mentoring arrangement to assist Green Bay NHS Trust with thinking through and testing ideas to improve aspects of their performance and strategy. The input of the mentoring trust was valued by the board at Green Bay NHS Trust, but questions were raised by those outside the buddying arrangement about whether the buddying trust was the right fit for the organisation, given that it was different in size, scale and performance. The impact of this partnership is difficult to disentangle from the other partnerships running contemporaneously, and the very intense overhaul of management and procedures required for the trust to exit special measures. The negative impact of special measures surfaced regularly in interviews with managerial and clinical staff.
‘We were one of the first [trusts placed in special measures] so it really affected our recruitment and retention. People left, people didn’t want to come and work here.’
Senior clinician (Green Bay NHS Trust)
‘everybody’s scrutinising you and you can’t get away from it. So there are, I don’t know how many, meetings a month where people are holding you to account, whether or not you’re doing what you should be doing to get out of special measures. And that is hugely time consuming.’
Senior manager (Green Bay NHS Trust)
Through a combination of actions, of which buddying was a part, Green Bay NHS Trust has considerably improved its performance in terms of financial management and staff engagement, and a CQC report shows no more red (inadequate) ratings. Improvements have also been attributed to other partnering arrangements that Green Bay NHS Trust was involved in. The voluntary partnership with the US-based organisation was seen by senior management as a useful tool for embedding quality improvement, although more generally it was acknowledged that it would take time for it to have an impact throughout the organisation, and was not viewed positively by all.
Mandated partnering at a structural level – case study C
Acquisition of a failing trust
St Phillips is a standalone, single-site trust of medium-to-large size. The trust has consistently achieved against regulatory targets for finance, quality and safety, and was rated as outstanding by the CQC.
Rowheath Park was failing and had a very poor reputation. Rated as inadequate by the CQC, Rowheath Park was put into special measures at the beginning of 2014. As polar opposites, the CQC saw St Phillips as a solution for dealing with the poor management that Rowheath Park had endured. Following discussion, the board for St Phillips agreed to acquire Rowheath Park.
Outcome of the partnership
This is the most mandatory of the partnership cases presented here: an acquisition at the request of the regulator, on the grounds that less formal partnerships, or indeed a full merger, would not have led to Rowheath Park adopting the culture and processes of the acquiring trust, which the CQC saw as the route to improvement.
‘If you’re merging two corporate cultures, which are likely to be quite different, I don’t know how you generate, at speed, a new corporate value, culture… at least with us it was like, “Fine. We’re coming in, it’s an acquisition. The St Phillips culture, the St Phillips corporate identity, the St Phillips values are going to come to Rowheath Park.”’
Medical director (St Phillips)
The stability of St Phillips’s board and the overall health of the organisation provided a strong and resilient foundation for the improvement efforts, which were led by the chief executive. To prepare for the acquisition, the clinical directors at St Phillips provided buddying support to their colleagues in Rowheath Park, observed activities, gave advice, and acted as a sounding board for service improvement ideas. This preparatory work aimed to create peer-to-peer contact between clinicians, provide visibility and openness to questions and discussion, and gather intelligence for St Phillips’s board.
Focus groups at Rowheath Park were used to introduce an HR-led programme to develop a new culture based on the values of St Phillips. A new clinical governance structure was introduced across the new integrated structure of the organisation. The acquisition also benefited from external resources: bridging finance from the Department of Health, and an external committee to oversee quality with external stakeholders acting as a sounding board.
This acquisition was challenging for both sides: interviews at St Phillips described the emotional labour of leading the change, being visible and having extensive face-to-face conversations. Even though St Phillips’s board was high performing and secure, the time committed to the new site meant that the organisation was at risk of failing to develop and nurture its own culture. On Rowheath Park’s side, some staff felt the experience of being taken over was traumatic, and perceived St Phillips as having a superior attitude.
Nevertheless, the improvements were substantial: Rowheath Park’s CQC rating went from inadequate to good within 12 months, and it met all NHS Improvement’s quality standards. Staff survey scores also improved, with Rowheath Park moving from the bottom 20% to the top 20% of comparable trusts.
Voluntary partnering at a structural level (contractual) – case study D
Contractual agreement with a private company
Southside is a specialist NHS centre that provides regional and national tertiary services. It began partnering with a private company, Diagnostic UK, on a limited basis by contracting them to provide a mobile imaging service. This arrangement grew into the building of a fixed scanning facility on a hospital site in the region that Southside covers.
Diagnostic UK has now secured a contract from Southside to deliver imaging and improvement support across England, which will involve the development of a national collaborative network.
Outcome of the partnership
The partnership between Southside and Diagnostic UK developed incrementally in response to demands or opportunities that arose. Initial small scale projects were underpinned by contracts between the organisations, providing clarity over respective roles and connected funding. This process enabled the organisations to build a foundation for more ambitious, larger scale projects – for example, by building trust between the respective executive teams that their partner would fulfil their responsibilities and could be trusted to share risk responsibly. The organisations were also willing to negotiate what their respective roles would be, making sure that both were satisfied with their own and each other’s contribution.
The initial partnering also built relationships between clinical, managerial and technical staff, exposing NHS staff, for example, to different ways of working and more productive approaches to using scanners. This collaboration at non-executive level created the foundation for the national partnership, which is aiming to build new fixed sites at 30 locations across England.
Moving to a national partnership has required mobilising more resources and infrastructure to, for example, expand the scope of data collection, which was previously limited to collecting activity data and simple patient feedback. The organisations have also had to create a governance structure at executive level, but they have been keen that the governance processes should not dictate what happens, and responsibility for taking forward the partnering has lain with clinical leads and senior managers. In Southside, those responsible include medical clinicians, physicists, and training and finance leads.
Interviews with Southside staff suggested that the experience of working closely with staff from Diagnostic UK had helped to break down perceived barriers between private and public organisations. They reported that despite some initial concerns about working with a non-NHS organisation, Diagnostic UK had a shared commitment to improving patient care. Despite being from different sectors, there was therefore sufficient cultural fit between the organisations to allow them to work comfortably together in relation to this partnering arrangement.
Voluntary partnering at a structural level (merger) – case study E
Voluntary merger between trusts
Greenpoint and Middleton Way are two specialist acute providers of small-to-medium size, which operate in a large, diverse metropolitan area. Driven by a range of contingent factors, the trusts began a process of collaboration that led to them merging. Middleton Way had financial problems and was dealing with the negative findings of a CQC report, leading to board turnover. Greenpoint was a high-performing specialist trust that had for some time been looking to build a new site near to Middleton Way.
Outcome of the partnership
The merger between Greenpoint and Middleton Way was built around a series of board-level discussions. Given the relative instability of Middleton Way, discussion between the trusts about the governance issues facing Middleton Way led to the chief executive of Greenpoint becoming the joint chief executive across both trusts.
As information and awareness of the situation at Middleton Way became apparent to Greenpoint, board-level discussions moved on to formally acquiring Middleton Way. A 12-month buddying relationship ensued, in which the chief executive and chair occupied joint roles. Other executives and non-executives from Greenpoint then followed, moving into joint trust roles 4–5 months ahead of the formal merger.
During this period, the approach taken by Greenpoint’s board was to instil a shared vision of ‘we are one trust’. Framing the language and behaviours around the acquisition as a collective effort was central to Greenpoint’s approach.
The merger was built around changes to corporate service functions. For example, the payroll provider aimed to make savings by consolidating back office and corporate services, thereby bringing financial stability to Middleton Way.
With the formal aspects of the merger only recently completed, the anticipated range of benefits around cost and improved responsiveness have yet to be realised. The proposed move to a single-site model would provide financial stability, as well as additional benefits of improved staff satisfaction and patient care. Quality improvement measures drawing on improvement science methods were developed to understand the impact of the changes being introduced.
The merger was facilitated by additional drivers. The application process was accelerated by the planning process for the sustainability and transformation partnerships, and the expectation that these partnerships would have a more system-wide leadership approach. Where previously it would have taken years to develop, the current environment allowed the merger to be completed in 12 months. This speed of development was challenging for Middleton Way, as perceptions of a takeover led to uncomfortable situations and feelings of inferiority. But, to support these efforts, plans were being put in place as the merger proceeded to further invest in organisational development, leadership and culture development for staff in both organisations.
‘we had to reassure the staff here that actually it’s a bigger health economy, you can no longer be a shining star in a sea of failing organisations, it’s about, “How do we survive together as a system, not as an organisation?”... we’ve had to take this organisation through that journey really’.
Organisational development lead (Middleton Way)
The experience also highlights the competing needs and demands of the regulators. While NHS Improvement was increasingly encouraging a fast-track transaction, the underlying processes rested on previous guidance and templates developed by Monitor and the Competition and Markets Authority. These processes were at odds with a fast-track approach, taking time to complete and were difficult to navigate.
‘I think we’ve gone through the process in spite of the regulatory framework and we kind of worked around it. Not because it’s helped us.’
Strategy lead (Greenpoint)
The negotiation of funding to support the merger also proved to be a challenge. The mixture of capital and revenue for the process, and support for the transition phase of the merger, meant negotiating with multiple bodies. This was only resolved when escalated to very senior staff in the NHS.
Ingredients for a successful partnership
The case studies reflect different scales of partnering (individual versus structural) and different natures of partnering (mandated versus voluntary). They suggest that all these types of partnering can make a positive contribution to improved quality, given the correct opportunities, investment and environment.
- Individual partnering can provide a cost-effective means to introduce new practices, and enable mentoring and reflection for those leading improvements. It has the potential to drive entrepreneurial activity, injecting innovation and energy to improvement efforts.
- Structural partnering facilitates more fundamental and sustained change across organisations and systems. The formality of agreement enables partners to have the confidence to invest capacity and energy in the arrangements and increase the scale of impact. Partnering can be successful between NHS and private organisations and bring helpful diversity of resources, skills and networks.
- Mandated partnering by regulators can make a positive contribution to the recovery of a struggling organisation. It requires careful assessment of the factors underlying the poor performance, and the partner to have sufficient capacity and motivation to respond to these factors.
- Voluntary partnering has the potential to tap into the intrinsic interests of those involved. However, appropriate coordination and governance is needed to plan and periodically analyse impact to make sure benefits are being realised.
Leading and managing partnering is different
The importance of senior and clinical leaders in achieving successful change is well established. This is also true in partnering, where engagement and influence has to cross organisational and service boundaries. Staff members not only need to have faith in their own leaders but also in those of their partnering organisations. A clear rationale is therefore needed in any partnering arrangement.
Managing across partners provides additional complexity due to different financial processes, internal accountabilities and underlying cultures. These complexities must be recognised to enable logistical issues to be considered and addressed. For example, HSMC’s research finds that structural partnering requires a formal infrastructure with support from shared project management capacity. Individual partnering may start informally, but will eventually need a framework to be sustained in the face of clinical work pressure. Testing out potential partners through smaller projects provides an opportunity to explore if the considerable investment in management time will be worthwhile. Rushing in to structural partnering and a presubscribed arrangement may lead to a poor fit and considerable diversion of management time.
Individual trust will always be key
Whatever the scale of the partnering, there will always be individuals whose personal collaboration will be key to success. Entering into such arrangements voluntarily will entail additional risk to resources, reputation and capacity. Successfully managing this risk will involve these key people being able to trust that their partner is sensitive to their requirements and pressures, and that they will act in joint rather than self interest. Previous positive interaction provides a foundation for collaboration, but such relationships will not always be in place. To otherwise enable trust, partners need the opportunity to progressively build a relationship over time through less risky and lower intensity projects, and their values need to be well aligned in relation to the partnership endeavour.
Mandated partnering arrangements that are brokered by an external body may not benefit from a good cultural fit. In such cases, the organisations will need to adopt one of their cultures – usually that of the organisation perceived to be higher performing – or develop a new, shared culture.
Doing so will require considerable and sustained effort across all levels of each organisation, which will take years rather than months. In such cases, trust will be fostered by transparency in what is being planned and initial agreements being honoured. Requiring a provider to engage with multiple partners as part of an organisational improvement plan will mean that multiple cultures need to be understood and responded to, which may be an unfeasible expectation at such a time of change.
Meaningful data are vital
Generating relevant, accurate and timely data to show the impact of partnering is a challenge. HSMC’s research finds that structural partnering has to consider a wider range of factors, but its scale has some advantages in that aggregated CQC and NHS staff survey performance measures may have some relevance. Smaller, more contractually based arrangements can include targeted data gathering and connected resourcing as part of the contract agreement.
There are also practical challenges of accessing data from across multiple providers with different information governance arrangements. In structural partnering, a joint performance board – which develops the dataset, considers related analytics and acts on the findings – is essential. In mandated partnering, regulators being part of such a board can provide a similar assurance.
Given the local contextual arrangements, individual partnering may require customised approaches initially, so organisations entering into such partnerships need to recognise the capacity cost. Patient perspectives can be invaluable in testing if partnering is leading to improved experience, which will motivate clinicians to maintain their commitment.
The environment can make or break partnering
The environment plays a major role in helping the partnering arrangement to achieve its potential, or preventing it from doing so.
Overly simplistic expectations and additional reporting requirements from external bodies could provide interference and distraction. Those who create such environments through commissioning, policy and regulatory processes must therefore be aware of their influence and use this responsibly. They should also recognise the limitations and costs of mandated partnering and that sometimes other types of partnering may be more appropriate.
Mandated partnering should not purely focus on the organisation of concern but also seek to engage the wider system. This can provide opportunities for partners to draw on additional resources and help to generate public approval for such arrangements. Quality oversight committees that involve regulators and other national bodies can provide an effective forum, enabling relevant connections and giving assurance.
Mandated partnering should be considered with caution and may be best seen as an option that can be offered rather than insisted on. If more directive intervention – such as integration of two or more organisations – is deemed necessary, then it is crucial for regulators to be open about these arrangements to engage staff and wider stakeholders.
Conclusion
Partnering is at the heart of current reforms in the NHS in England. New types of alliances are being explored to improve care and maintain quality despite pressures on budgets. These partnerships reflect the partnering arrangements being used in other sectors and countries, and build on similar assumptions about the benefits of diversification, sharing good practices and pooling resources.
This research confirms the findings from previous analyses, that while partnering does have potential benefits, these are not easy or quick to achieve. To have a meaningful impact on the quality of care, the right form of partnering needs to be used in the right context and, as we summarise in Table 2, it needs to be accompanied by the right set of enabling factors.
Table 2: Partnering types and impacts
|
Partnering arrangement |
Main advantages |
Helpful context |
Key enablers |
|
Voluntary – individual |
Facilitating clinician-led improvement projects across a common pathway Securing support from immediate teams Introducing new practices quickly (although at small scale) |
Previous positive working across the services Organisational support for partnering in general and with the suggested partner(s) Identified need or opportunity to improve patient care |
Leads within individual services communicate well and share responsibilities Engaging operational managers from both partners Structuring in time for shared reflection on progress Mainstreaming within normal processes and data capture |
|
Mandated – individual |
Provides a mentoring opportunity to share concerns and discuss potential opportunities Relatively low cost and easy to organise without major organisational disruptions on either side |
Organisation seen as requiring improvement recognises the need for change and is looking for support Organisation seen as requiring improvement has resources required to implement changes Individual partnering is linked to wider internal and external change programmes |
Individuals in both organisations have sufficient time to meaningfully engage Individuals in both organisations remain connected throughout the process Prioritise and focus on key partnering opportunities rather than introducing several major changes at the same time |
|
Mandated – structural |
Enables acquiring organisation to have legitimacy and power to introduce its practices Internal and external stakeholders understand the basis of the relationships Acquiring organisation can shape the new entity to meet its overall strategy |
Acquiring organisation is already looking for the opportunity to partner Acquiring organisation has a strong financial position and a stable board Regulator and commissioner are willing to provide financial support and time for the acquisition to be undertaken |
Thorough communication to staff and stakeholders of both organisations Seeking relevant data, patient experiences and staff perspectives to assess the current position Introducing shared governance and management structures Enabling key stakeholders to have regular updates and contribute insights Recognise strengths within acquired organisation and avoid negative stereotyping |
|
Voluntary – structural |
More formal sharing of resources and risks Partnering provides resources and influence to fulfil an individual organisation’s objectives Opportunity to add value beyond fragmented organisational responses |
Organisations are in strong financial positions and have stable boards Organisations are comfortable with partnering in general Previous positive experiences of working together through smaller scale projects Opportunity to attract new resources to deliver shared project(s) |
Dedicating sufficient resources to develop more formal and large-scale partnering Key values of organisation are similar in relation to the project(s) in question Opportunity for key individuals within the organisations to directly engage with their counterparts Clear vision of what partnering will achieve with the positive support of board and executive members |
References
- NHS England, NHS Improvement. NHS operational planning and contracting guidance 2017–2019. 2016: p4, paragraph 4. Available from: www.england.nhs.uk/wp-content/uploads/2016/09/NHS-operational-planning-guidance-201617-201819.pdf
- NHS. Five year forward view. 2014. Available from: www.england.nhs.uk/publication/nhs-five-year-forward-view
- The Health Foundation. Closing the gap through clinical communities. Available from: www.health.org.uk/programmes/closing-gap-through-clinical-communities
- The Health Foundation. Effective networks for improvement: Developing and managing effective networks to support quality improvement in healthcare. 2014. Available from: www.health.org.uk/publication/effective-networks-improvement
- The Health Foundation. Q. Available from: https://q.health.org.uk
- Miller R, Millar R. Partnering for improvement: inter-organisational developments in the NHS. 2017. Available from: www.birmingham.ac.uk/partnering-for-improvement
- Dalton D. Examining options and opportunities for providers of NHS care: the Dalton review. 2014. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/ 384126/Dalton_Review.pdf
- Monitor, Care Quality Commission, Trust Development Authority. A guide to special measures: updated February 2015. Available from: www.cqc.org.uk/sites/default/files/20150211_a_guide_to_special_measures_updated_Feb_2015.pdf
Acknowledgements
Thank you to all those who contributed their time and insights to this research.
About the authors
Robin Miller is Deputy Director of the Health Services Management Centre (HSMC). Ross Millar is a Senior Lecturer in Health Policy and Management, and Director of Learning and Teaching at HSMC. Tim Gardner is Senior Policy Fellow at the Health Foundation. Will Warburton is Director of Improvement at the Health Foundation.